The Crisis in Rural Health Care
What if you had an accident and the closest Emergency Room was over 30 minutes away?
What if you were sick and there were no physicians or hospital beds in your community?
What if you were pregnant and the closest place to deliver your baby was an hour away?
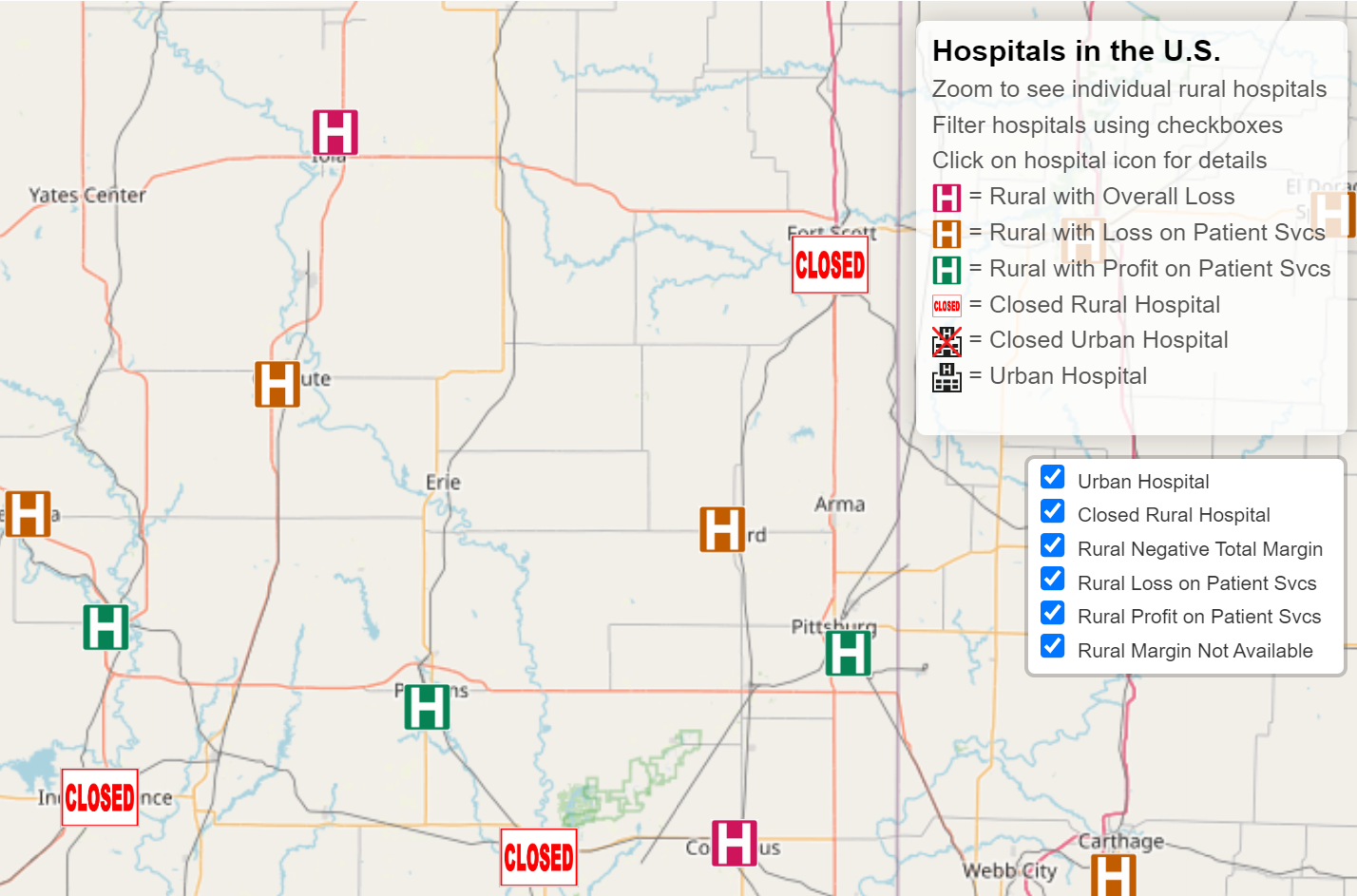
Millions of Americans are facing these situations because rural hospitals are being forced to close or eliminate services.
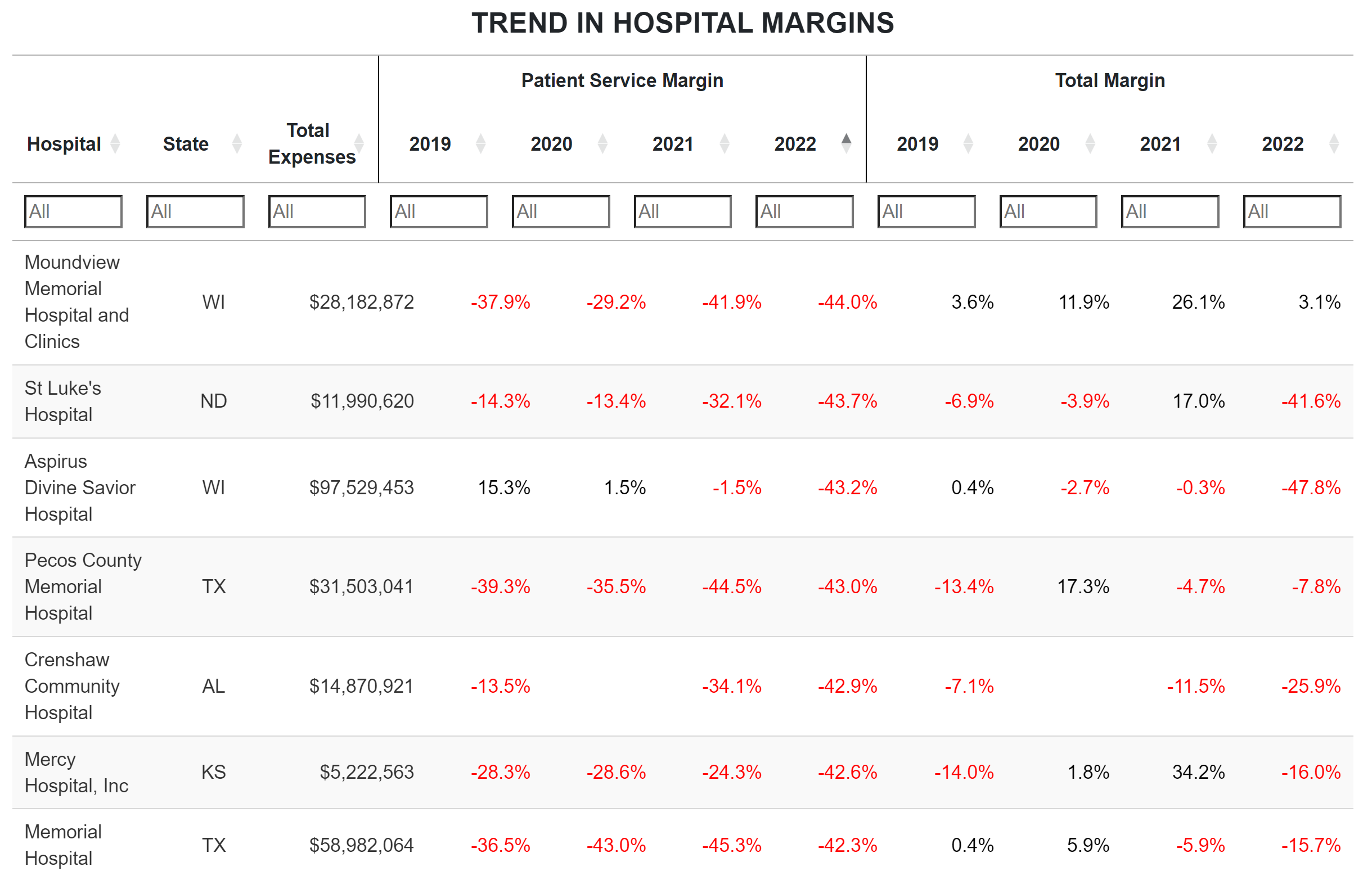
More than 100 rural hospitals have closed over the past decade, and over 700 additional rural hospitals – one-third of all rural hospitals in the country – are at risk of closing in the near future. Even if the residents of these communities have insurance to pay for health care services, there is nowhere in their community they can use the insurance.
Over 100 rural hospitals have stopped delivering babies over the past 5 years, and less than half of all rural hospitals still have labor and delivery services.
The primary cause of these problems is that payments from health insurance plans are not adequate to sustain essential services in rural communities. Current federal programs don’t solve the problems facing small rural hospitals, and some proposed changes would make the problems worse. Rural hospitals need both adequate payments and a better payment system in order to provide essential healthcare services for their communities.
Learn more about the problems, the causes, and the solutions here:
Overview of Causes and Solutions
Stopping the Loss of Rural Maternity Care
The Importance of Rural Hospitals
The Causes of Rural Hospital Problems
The Cost of Rural Hospital Services
Reports on Problems & Solutions
Reports describing rural hospital problems and solutions are available at no charge here.
Data on Hospitals
Data on the financial status of individual rural and urban hospitals are available here.