Global Budgets
The primary goal of most global hospital budget programs has been to reduce hospital spending, not to prevent closure of small hospitals. Although “global hospital budgets” have been proposed as a way of helping small rural hospitals, most global budget programs were created in order to limit or reduce payments to hospitals, not to address shortfalls in payment or prevent closure of small rural hospitals. Although Maryland’s global budget program has been cited as an example of how rural hospitals can benefit from this approach, the smallest rural hospital in Maryland closed in 2020 despite operating under the global budget system. Under the Pennsylvania Rural Health Model, hospitals receive global budgets that are based on the amount of revenues they received in the past, and there is no assurance the budgets will cover the current cost of delivering essential services. Under the CMS CHART Model, hospitals that participate would receive less revenue than they have received in the past, even if past revenues were insufficient to cover the costs of services.
Hospital global budget programs are far more complex than they seem. In Maryland, a state agency regulates the fees each hospital is paid for each individual services, and it uses complex formulas to establish an annual budget for each hospital. The hospital has to adjust its service fees during the year in order to stay within the budget, unless the state approves a modification to the budget. In Maryland, all payers are required to pay the hospital the fees approved by the state, including Medicare and Medicaid.
Some rural hospitals could benefit from a global budget program in the short run, but most would likely be harmed financially. Hospitals in communities that are experiencing significant population losses or that deliver unnecessary services could benefit from a global budget program, at least in the short run, because revenues would no longer decrease when the volume of services decreases. However, hospitals that experience higher costs or higher volumes of services due to circumstances beyond their control would likely be harmed, since their revenues would no longer increase to help cover the additional costs.
Access to care for patients could be harmed by a global budget. Under a global budget, a hospital receives the same amount of revenue regardless of how many services it delivers. This can result in delays in patients receiving the services they need. For example, after implementation of global budgets, Maryland had the longest emergency department wait times of any state in the country.
Other countries have moved away from using global budget systems. Global hospital budgets have been used for many decades outside of the U.S. However, because of concerns about long waiting times for services, many countries have modified or replaced global budgets with “activity-based” payment systems, similar to some of the fee-for-service payment systems used in the U.S.
The Concept of a “Global Budget” for a Hospital
Over the past several years, there has been growing discussion about using “global budgets” as a way of reducing financial problems for rural hospitals and preventing closures. Under a global budget, a hospital’s revenue is no longer based on the number of services that it delivers, so the hospital will not lose revenue if it delivers fewer services because of either a decline in population in the local community, improved health of the residents, or reluctance of residents to obtain services during a pandemic.
Although various forms of global budgets for hospitals have been used in a number of other countries for decades, they have been used only rarely in the United States. However, the State of Maryland now requires the use of global budgets for all hospitals in the state, and the CMS Center for Medicare and Medicaid Innovation (CMMI) has funded a demonstration project in Pennsylvania under which several hospitals are receiving a portion of their payments based on a global budget model. Interest in global budgets increased in 2020 because many hospitals experienced significant reductions in revenue due to the lower volume of elective healthcare services during the coronavirus pandemic, and some or all of those revenue losses could have been prevented if the hospitals had been paid through a global budget. In August 2020, CMMI announced the “Community Health Access and Rural Transformation (CHART) Model;” the CHART “Community Transformation Track” includes a component in which hospitals in up to 15 regions can receive payments under a global hospital budget model.
In contrast to fee-for-service payments and cost-based payments, there is no standard way of defining a global budget or paying a hospital based on one. The impact of a global budget on a small rural hospital will depend heavily on the details of how the budget is designed, and also on the size and characteristics of the community the hospital serves. The approach being used in Maryland is very different from the approaches being used in Pennsylvania and in the CHART Model, and all three of those are different from the payment models used for hospitals in other countries. Importantly, the primary goal of the global budget programs both in the U.S. and other countries has been to limit or reduce the amount of spending on hospitals, not to reduce financial losses and prevent closures of small, rural hospitals.
Global Budgets in Maryland
How Global Budgets Work in Maryland
Since 2014, no hospital in Maryland has been permitted to receive more revenue for inpatient and outpatient services during a year than the amount of “Approved Regulated Revenue” the state has approved in advance. This revenue amount is determined through the state’s Global Budget Revenue program and is commonly referred to as the hospital’s “global budget.”
The global budget in Maryland is, in fact, a budget, not a payment. A hospital in Maryland is still paid a fee for each individual service it delivers by the individual health insurance plan that insures the patient who received the service. The way the hospital stays within the budget is by changing the amounts of the fees that it charges for individual services. If the hospital’s revenue exceeds its budget, it must cut the fees that it charges for individual services. If the hospital’s revenue falls short of its budget, it is permitted to increase its fees to make up the difference.
Maryland can ensure that a hospital receives no more and no less than the global budget amount because the state has a power no other state has – it regulates the fees that hospitals charge for inpatient and outpatient services and every payer is required to pay the hospital those fees. This includes payments for services delivered to Medicare beneficiaries, because Maryland is the only state in the country that has been given authority by Congress to determine the amounts that the Medicare program will pay for hospital services in the state.
As a result, if a hospital has to charge more for services in order to get the full amount of revenue specified in the global budget, all health insurance plans, Medicaid, and Medicare must pay the higher fees. Conversely, if the hospital needs to cut its fees in order to stay within the budget, the state can require that it do so. A hospital is permitted to increase or decrease its fees by up to 5% during the year in order to stay within the budget, and it can increase or decrease fees by as much as 10% if it receives approval from the state to do so. If the hospital’s actual revenue during the year ends up being higher or lower than the approved budget, then the hospital’s fees have to be increased or decreased during the following year to make up the difference.1
In contrast to other states, where there are typically large differences in the amounts paid for the same service by Medicare, Medicaid, and different health insurance plans, in Maryland, all payers pay essentially the same amount for each individual service.2 Moreover, the amounts payers pay are set at levels the state views as sufficient to cover the hospital’s cost of caring for uninsured patients.
Both fees for individual services and the global budget amounts are determined by the Maryland Health Services Cost Review Commission (HSCRC), an independent state commission led by 7 gubernatorially-appointed commissioners. The Commission was created in 1971 and it has been setting hospital rates for both Medicare and private payers since 1977. The Commission sets rates for 47 acute general hospitals, 3 specialty hospitals, and 3 psychiatric hospitals. It has over 40 staff, and its budget is funded through an assessment on hospitals rather than through general state tax revenues.3
The HSCRC only regulates the prices of inpatient and outpatient hospital services. It does not control the amounts that physicians and other providers are paid for the services they deliver, nor does it regulate other services that hospitals offer. The formal name for the global budget is “Approved Regulated Revenue” because only the revenue for the services whose prices are regulated by HSCRC is included.
The History and Goals of the Maryland Global Budget System
Maryland’s global budget system was not created to solve financial challenges facing small or rural hospitals in the state. The state’s rate regulation system already allowed it to ensure that a hospital received enough revenue to cover its costs, since the state could authorize rate increases that all payers would have to pay.
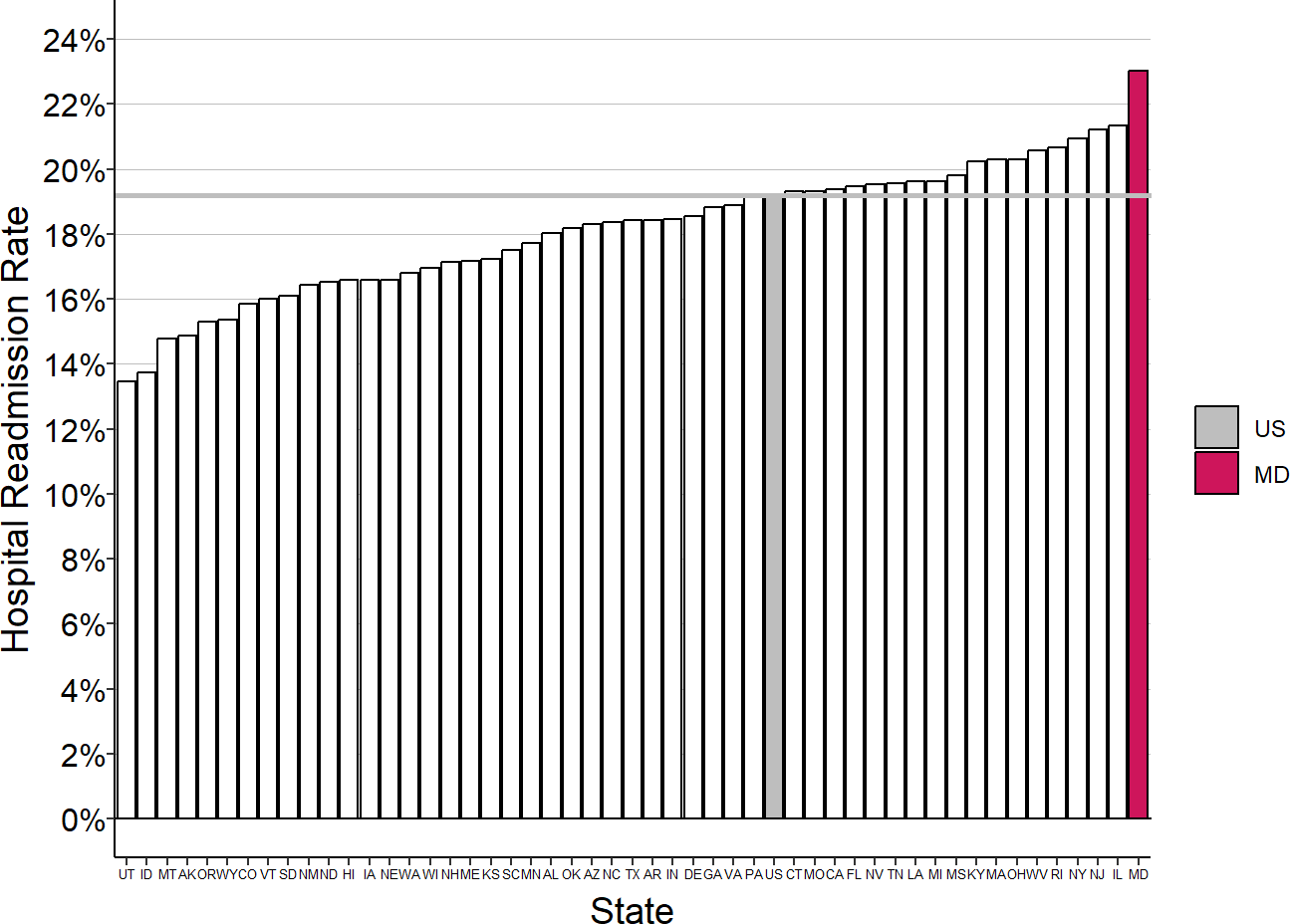
The problem Maryland was trying to address was over-utilization of hospital services. Maryland had the highest rate of hospital readmissions for Medicare beneficiaries in the country in 2010, and it also had one of the highest rates of hospital admissions. The global budgets were explicitly intended to serve as a “revenue constraint and quality improvement system” to “provide hospitals with strong financial incentives to manage their resources efficiently and effectively in order to slow the rate of increase in health care costs and improve health care delivery processes and outcomes.”4
Figure 1
Medicare Hospital Readmission Rates by State, 2010
Source: Medicare Geographic Variation Public Use File. US=National average.
Hospitals in Maryland, like those in every other state, were paid based on how many hospital admissions they had, so they were financially penalized if they reduced avoidable hospital admissions and readmissions. Maryland’s rate regulation authority gave it the ability to eliminate that penalty by allowing a hospital to charge more for services when utilization decreased. However, doing this threatened to violate the terms of the federal waiver that allowed the state to set Medicare payment amounts. The federal waiver was conditional on payments per admission for Medicare beneficiaries in Maryland increasing at a slower rate than the amounts Medicare paid in the rest of the country. Even if total Medicare spending on hospital admissions in Maryland decreased because the number of hospital admissions decreased by more than the payment per admission increased, the state’s waiver was based solely on how much the Medicare payment per admission increased.
To avoid this, Maryland entered into a revised agreement with CMS in 2014 that held the state accountable for controlling Medicare spending on hospital services per beneficiary rather than the amount spent per admission. Under what was known as the Maryland All-Payer Model, in return for the continued ability to set hospital payment rates for Medicare, Maryland agreed to do the following things over a 5-year period:
Limit annual all-payer per capita inpatient and outpatient hospital cost growth to the previous 10-year average annual growth in gross state product (3.58%).
Generate $330 million in “savings” to Medicare based on the difference in the Medicare per-beneficiary total hospital cost growth rate between Maryland and that of the nation overall.5
Reduce the 30-day readmission rate to the unadjusted national Medicare average.
Reduce the rate of potentially preventable complications by nearly 30 percent.
Limit the annual growth rate in per-beneficiary total cost of care (TCOC) for Maryland Medicare beneficiaries to no greater than one percentage point above the annual national Medicare growth rate in that year.
Limit the annual growth rate in per-beneficiary TCOC for Maryland Medicare beneficiaries to no greater than the national growth rate in at least 1 of any 2 consecutive years.
Submit an annual report demonstrating performance on various population health measures.
How Global Budgets in Maryland Are Set
The process of setting global budgets for each hospital in Maryland is very complex. In order to encourage reductions in hospitalization and to satisfy the terms of the new Medicare waiver, a multi-step process is used to determine the global budget for each hospital. Each year, the HSCRC determines a new budget for a hospital using the following factors:6
the amount of the hospital’s global budget in the previous year;
inflation in costs of drugs, supplies, and wages;
the hospital’s performance in improving quality, reducing readmissions, reducing hospital-acquired conditions, and reducing other types of potentially avoidable utilization;
changes in the amount of uncompensated care at the hospital;
changes in insurance coverage in the state that affect utilization of services;
changes in the size and composition of the population served by the hospital;
unanticipated events that significantly increase utilization of hospital services (e.g., a natural disaster or epidemic);
changes in the hospital’s market share among Maryland residents (but only for services that are not deemed to represent “potentially avoidable utilization”);
changes in the number of out-of-state residents using a hospital’s services;
the hospital’s efficiency in delivering services relative to other hospitals;
shifts in the delivery of services to unregulated settings (e.g., ambulatory surgery centers or physician practice offices);
transfers of patients from one hospital to another;
amounts the hospital is required to pay the state under various tax/assessment programs;
the variance between actual and approved revenue in the prior year;
the extent to which the state has generated the total amount of statewide savings in Medicare spending promised as part of the state’s agreement with CMS;
the growth in total hospital spending in Maryland relative to the state economy; and
changes requested by the hospital to support new service lines, capital needs, etc.
Not only is the overall process complex, the calculations for many of the individual steps make it even more complex. For example, the budget is adjusted for changes in the population of the hospital’s service area using a Demographic Adjustment Factor determined through a complex series of steps.
(.)
A Virtual Patient Service Area (VPSA) is defined for each hospital based on the communities where the hospital’s patients live. In more rural areas, the VPSA is defined in terms of counties, whereas in the rest of the state, it is defined in terms of zip codes.
Each hospital is assigned a portion of the population of the VPSA as follows:
For each hospital, the number of Equivalent Case Mix Adjusted Discharges (ECMADs) is calculated for six separate age cohorts (0-14, 15-54, 55-64, 65-74, 75-84, and 85+) in each county or zip code in the VPSA. The ECMAD includes both inpatient and outpatient services; outpatient visits are converted to equivalent inpatient discharges using the ratio of average inpatient charges per discharge to the average outpatient charge per visit. The case mix adjustments are determined for inpatient charges using the 3M APR-DRG grouper and for outpatient charges using the 3M EAPG (Enhanced Ambulatory Outpatient Groups) grouper.7
In each VPSA, estimates are made of the number of residents in each of the six separate age cohorts for the base year and the current year.
The hospital is assigned a proportion of the base year population in each age cohort and county/zip code based on the number of ECMADs the hospital delivered to residents of that county/zip code in that age cohort relative to the total ECMADs delivered by all hospitals to residents of that county/zip code in that age cohort. For example, if there are 1,000 individuals ages 55-64 living in zip code X, if there were 20 Equivalent Case Mix Adjusted Discharges of 55-64 year-old residents of zip code X at all hospitals in the base year, and if Hospital A delivered 10 of those discharges, then Hospital A would be assigned 50% (10/20) of the 1,000 55-64 residents in zip code X.
The hospital’s assigned population in each age cohort and each county/zip code in the VPSA are summed to determine the hospital’s total base year service population.
The age-adjusted population growth rate for the hospital’s service population is determined as follows:
A relative cost weight is determined for each age cohort by taking the total statewide hospital charges per capita for patients in each age cohort and dividing by the total statewide hospital charges per capita for all ages. For example, if the average total charge per patient for patients age 55-64 is 1.5 times the overall average charge per patient, then the age 55-64 cohort is assigned a weight of 1.5.
In each age cohort in each county/zip code, the percentage growth in the number of residents between the base year and the projection year is estimated.
The population growth rate in each age cohort and county/zip code is multiplied by the relative cost weight for that age cohort and county/zip code. For example, if the number of 55-64-year-olds living in a particular zip code is estimated to have increased by 10% and the cost weight for 55-64-year-olds is 1.5, then the adjusted growth rate for that age cohort is 15%.
The adjusted growth rate in each age cohort and county/zip code is multiplied by the hospital’s assigned population in that age cohort and county/zip code, and the products are summed over all age cohorts and counties/zip codes in the VPSA and divided by the hospital’s total base year service population to determine the hospital’s age-adjusted projected population-related growth.
A Demographic Adjustment Factor for the hospital is determined from the age-adjusted population growth rate for the hospital’s service area as follows:
The percentage of the hospital’s revenue that is determined to have resulted from Potentially Avoidable Utilization (PAU) is calculated. PAU is determined by using computer programs to examine each of the hospital’s discharges and outpatient services and categorize them as either PAU or not. This includes:8
30-day, all-cause, all-hospital inpatient readmissions, excluding planned readmissions;
Prevention quality indicator overall composite measure (PQI #90) as defined by the Agency for Healthcare Research and Quality (AHRQ) except for PQI 02 (Perforated Appendix) and PQI 09 (low birth weight);
65 potentially preventable conditions (PPCs) determined by 3M software; and
Outpatient rehospitalizations in the emergency room or observation occurring between 1 to 30 days of an inpatient admission.
The hospital’s age-adjusted population growth rate is reduced by the PAU percentage. For example, if the hospital’s age-adjusted population growth rate is 5% and if 20% of the hospital’s revenue was determined to be potentially avoidable, the growth rate would be reduced to 4%.
An “efficiency adjustment” may then be applied to this rate if the PAU/age-adjusted growth rates for all hospitals would result in total statewide hospital spending that exceeds the overall target population increase allowance. For example, if the total statewide increase in hospital spending would be 2% but the target growth rate is 1%, then a 50% efficiency adjustment would be applied to every hospital’s PAU/age-adjusted rate to determine its final Demographic Adjustment Factor.
Since many patients will have a choice of two or more hospitals for some or all of the services they need, adjustments have to be made to hospital budgets if patients begin using different hospitals for their services. A complex methodology is used to distinguish an increase in a hospital’s market share from an increase in the number of services the hospital delivers to the same patients; the key steps are:
The number of inpatient and outpatient services that each hospital delivers to patients living in a specific zip code or county is determined. The number of admissions is calculated separately for each of 47 service lines (defined by groups of APR-DRGs), and the number of outpatient services is calculated separately for 11 different service lines.
Any inpatient or outpatient services that are determined to represent Potentially Avoidable Utilization are excluded from the totals. This is designed to avoid giving a hospital credit for treating a patient who may not have needed the service and to avoid penalizing a hospital for not treating such a patient. In addition, a series of highly-specialized services such as organ transplants are excluded.
The growth in volumes at hospitals with utilization increases is compared to the decline in volumes at hospitals with utilization decreases. The lesser of the total volume gains and losses is determined, and each hospital then receives its relative proportion of that total.
The Impact of Maryland’s System on Small Rural Hospitals
Figure 2
Edward W. McCready Hospital, Maryland
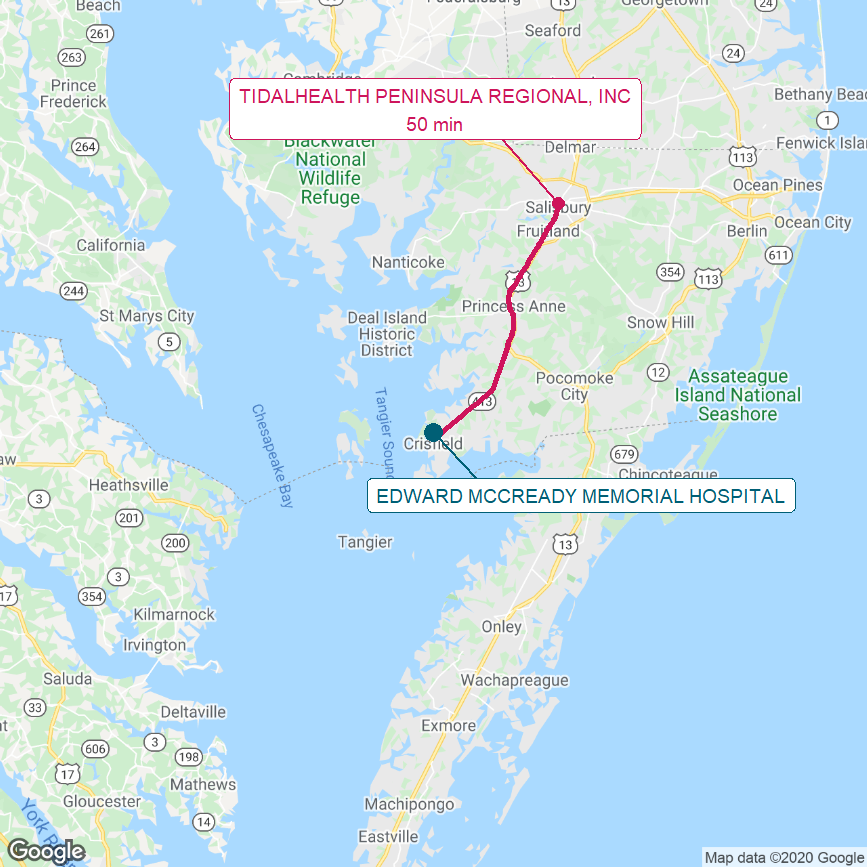
Map shows the Lower Eastern Shore of Maryland. The red line shows the most direct driving route from McCready Hospital to the next-closest hospital and the estimated travel time.
Maryland has no Critical Access Hospitals, and it had only one rural hospital that was as small as the hospitals discussed in The Causes of Rural Hospital Problems – the Edward W. McCready Memorial Hospital, located in the town of Crisfield on Maryland’s Lower Eastern Shore.
In 2019, McCready Hospital had total operating expenses of $17.8 million and an average daily acute census of 1.9 patients. It was the only hospital in Somerset County, Maryland and served a population of about 7,000. The next closest hospital is the Peninsula Regional Health System in Salisbury, which is a 50-minute drive from Crisfield.
Despite participating in the global budget program, McCready Hospital lost money every year from 2015 to 2019. Losses were about -4% from 2016-2018, and then increased to more than -5% in 2019, and the hospital’s current net assets (current assets minus current liabilities) decreased every year as a result.
Figure 3
Total Margin and Net Current Assets Prior to Closure
Edward W. McCready Hospital, Maryland
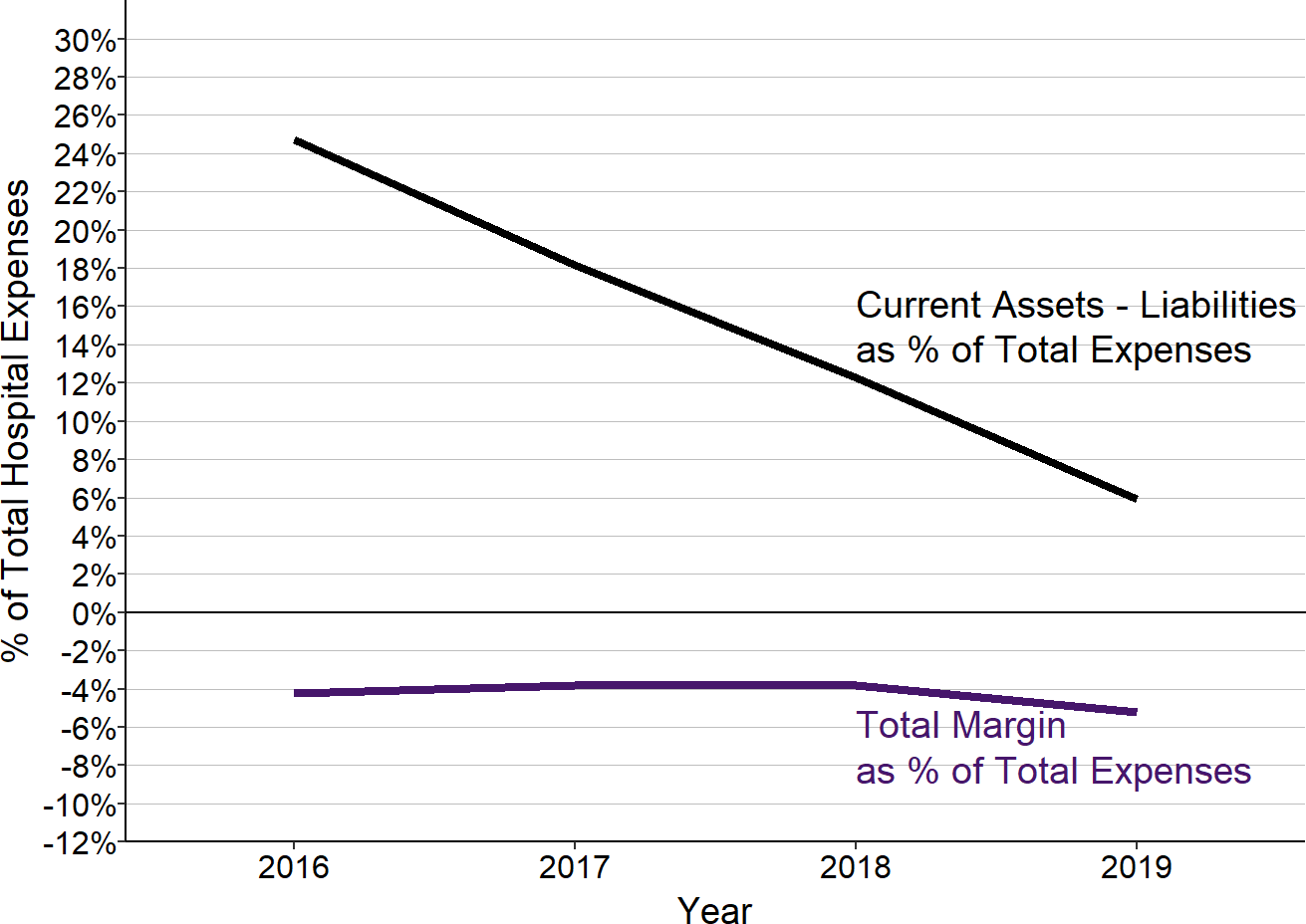
McCready Hospital closed in 2020.
Because of the losses, McCready was forced to close as a free-standing hospital in 2020. Peninsula Regional Health System, which operates Peninsula Regional Medical Center (the largest hospital on the Eastern Shore with 266 beds) and Nanticoke Memorial Hospital (a 139-bed hospital in Seaford, Delaware), acquired the hospital’s facilities and it has stated that it plans to continue operating the emergency department and primary care clinic and providing laboratory/imaging services at the same site until it builds a new outpatient facility several miles away. Inpatient and surgical services will no longer be delivered in Crisfield.
A 2017 case study9 describing McCready Hospital stated that the HSCRC rate setting process was a “complicated and lengthy negotiation” that was “rarely finalized by the start of the fiscal year when it takes effect” and required hiring a consultant for “guidance in completing the complex rate-setting worksheet.” The case study noted that because of the impact of utilization variability on the hospital’s margins, the hospital staff had to continuously review revenues in order to make adjustments in fees to stay within the global budget, and because of the hospital’s small size, it was difficult to make fee changes that would offset changes in utilization. In a year when the hospital experienced significant and unexpected growth in the volume of surgeries, the state reportedly worked with the hospital to increase the global budget. Moreover, changes in fees made during the year in order to stay within the global budget meant that patients could pay different amounts for the same test during the same year. The case study also reported that McCready Hospital was able to open an urgent care center in a town 14 miles away because revenue from services delivered there would not be included under the global budget.10
The Impact of Maryland’s System on Larger Rural Hospitals
Almost all of the hospitals in Maryland are in urban areas. Only five of the hospitals that have participated in the global budget program were located in a rural community, and the smallest of those (McCready Hospital) closed in 2020. The four rural hospitals that are still open are large in size relative to rural hospitals in other parts of the country; all of them have more than $45 million in total annual expenses, and one spends over $200 million per year. However, despite participating in the global budget program, all but the largest hospital had operating losses in 2019.
Several studies11 have examined the impact of the Maryland global budget system on “rural hospitals,” but five of the eight hospitals examined in these studies are actually large hospitals that are not federally-designated as rural hospitals, while three of the six Maryland hospitals that are located in a rural area were not included in the analyses.12 The eight hospitals in these studies are those where HSCRC implemented its initial version of the global budget methodology (the Total Patient Revenue system, or “TPR”) in 2010. The TPR hospitals are described as “rural” by HSCRC because each is the only hospital located in its community; HSCRC began implementation of global budgets at these hospitals because there was less need to make adjustments for changes in hospital market share than in areas that have multiple hospitals. Two of the other rural hospitals in the state (including the smallest hospital, McCready Hospital) began participating in a global payment arrangement with HSCRC before 2010, and the studies excluded those two from the analyses because of that.
The TPR hospitals are much larger and deliver far more inpatient care than most rural hospitals in other states. The median acute census of the TPR hospitals is 55, whereas the median number of acute patients in rural hospitals nationally is only 6. The median total expense of the TPR hospitals was over $165 million, over four times the median of $36 million for rural hospitals nationally.
As shown below, expenses in all of the core service lines are much higher at the Maryland “rural” hospitals than they are at most rural hospitals in other states. The difference is particularly large for inpatient care, which is consistent with the fact that Maryland has had much higher rates of hospital utilization than other states. However, this difference means that the Maryland hospitals had much bigger opportunities to reduce inpatient admissions and spending than rural hospitals in other states would have, and the financial losses at the hospitals from such reductions would be much greater in Maryland than in other states in the absence of the global budget system.
Figure 4
Service Line Costs in Maryland TPR Hospitals
and U.S. Rural Hospitals
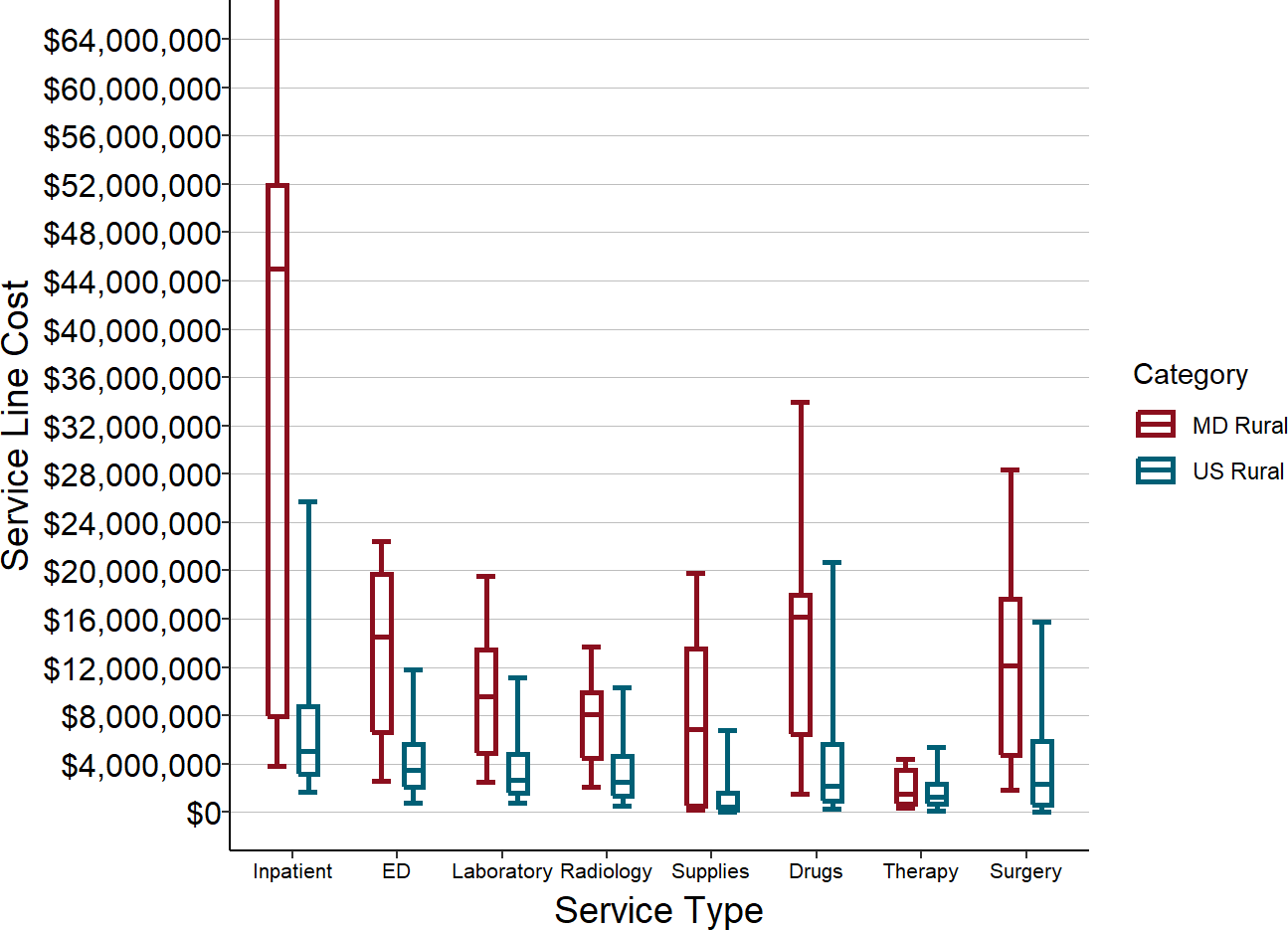
Values shown are median costs for the most recent three years available. TPR = Maryland Total Patient Revenue
Since the primary goal of creating the global budgets was to encourage reductions in unnecessary hospital admissions and outpatient services, the primary focus of all of the studies has been determining whether the number of services delivered at the hospitals increased or decreased. Three of the studies13 found there was no reduction in hospital admissions or readmissions at the TPR hospitals compared to similar hospitals that were not participating in the global payment arrangement, but a fourth study found that inpatient admissions decreased.14 Three of the studies found large reductions in outpatient services such as clinic visits and surgeries, but no significant change in Emergency Department visits.15 However, all of these studies only examined changes during the first few years after the global budgets and none examined changes in utilization or spending after 2013.
In 2014, the global budget program was expanded to include all hospitals in Maryland. CMS conducted an evaluation of the impacts of the overall program that examined changes in utilization and spending through 2018.16 This study found that there had been reductions in spending on hospital care and overall healthcare services for Medicare beneficiaries, but not for commercial insurance patients. While the study found there were reductions in inpatient admissions for Medicare, Medicaid, and commercial insurance patients, the reductions were only statistically significant for Medicare patients. The study authors reported that they did not find any consistent differences in the impacts for rural vs. urban residents, but they defined “rural” as living in non-metropolitan areas, which included urban areas as well as rural areas.
The Impact of Maryland’s System on Patient Access to Services
One of the principal concerns about a global budget system is whether it will be more difficult for a patient to obtain services. If a hospital’s revenue is no longer tied to the number of services it delivers, then it no longer experiences any financial penalty if patients are denied services or if they have to wait to receive them, and it no longer has the ability to generate the additional revenue needed to pay for expanded service capacity.
Many countries that have used global budgets for hospitals have national systems for monitoring the amount of time that patients have to wait to receive services, but the U.S. has no such system because there have not been concerns about delays in service under fee-for-service or cost-based payment systems.
As part of its Hospital Compare program, CMS used to collect information on the amount of time patients spend waiting to be seen in Emergency Departments and it still collects information on the amount of time patients who need to be admitted wait in the ED for a hospital bed. The data show that patients in Maryland waited longer to be seen in the ED than in any other state in 2017. In addition, patients in Maryland who needed to be admitted had a median wait of over 6 hours for a hospital bed, the second highest of any state.17
Figure 5
Median Time Spent Waiting in ED Before Being Seen, 2017
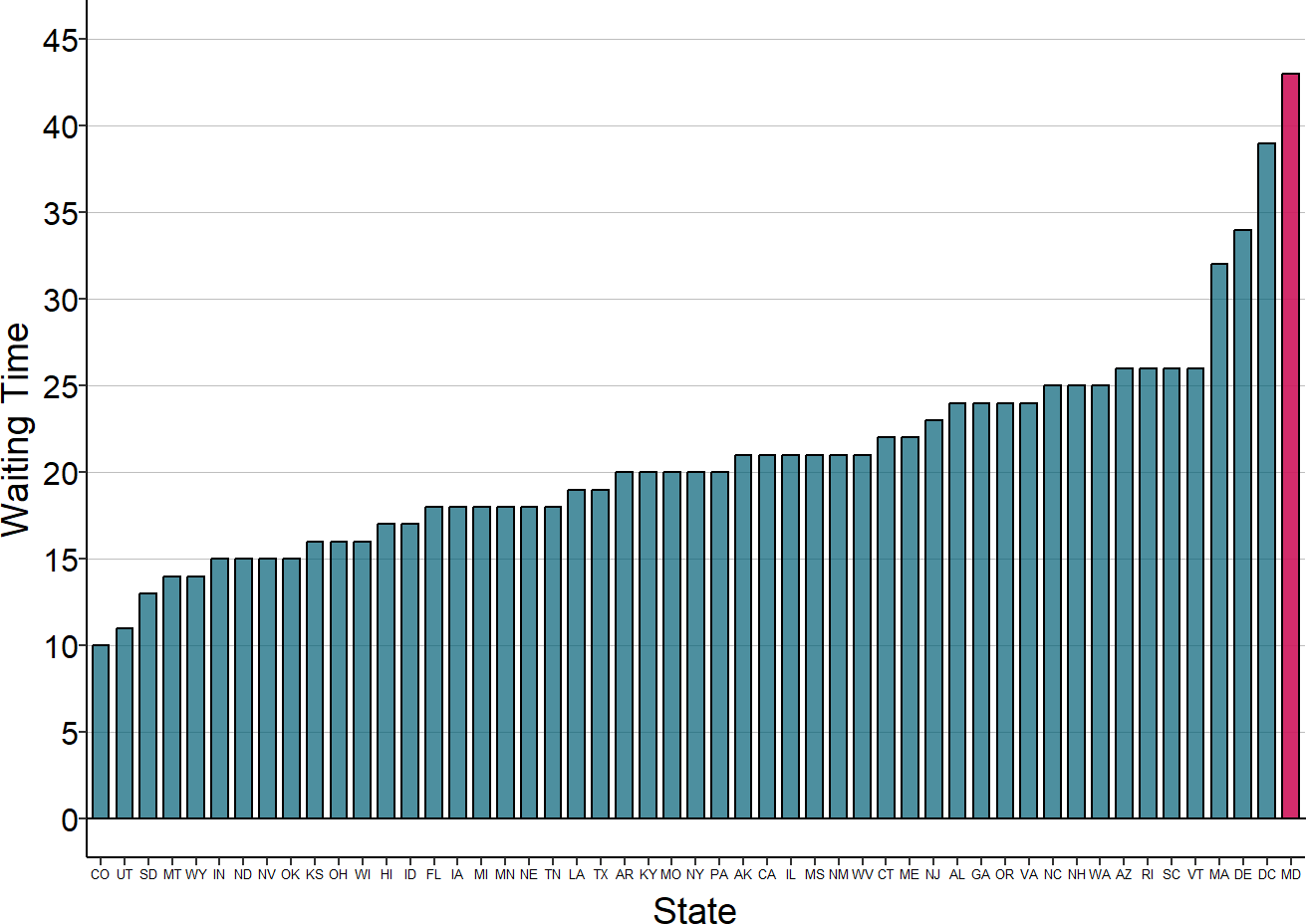
Source: Average by state from CMS Hospital Compare. Red bar is average for Maryland
The evaluation of the Maryland model conducted by CMS did not look at the issue of wait times for services. The study found that patients reported their experience in Maryland hospitals was worse than patients reported for comparison hospitals on nearly every experience measure examined, but the experience measures in Maryland did not worsen under the global budgets. The study did find that Medicare beneficiaries were more likely to obtain services from physicians’ offices than from hospital outpatient departments after the global budgets were put in place.18
The Pennsylvania Rural Health Model
The History and Goals of the Pennsylvania Rural Health Model
The Pennsylvania Rural Health Model was a demonstration project that was created in 2017 by the CMS Center for Medicare and Medicaid Innovation (CMMI) specifically for rural hospitals in Pennsylvania. It was designed to test whether paying rural hospitals a fixed, predetermined amount for all hospital-based inpatient and outpatient services (i.e., a “global budget”) will enable the hospitals “to invest in quality and preventive care, and to tailor their services to better meet the needs of their local communities.”19 The demonstration ended at the end of 2024.
The Pennsylvania Rural Health Model was not designed to increase payments to rural hospitals in order to eliminate or prevent financial losses; in fact, it was required to reduce the total amount that Medicare spends on hospital services for Medicare beneficiaries who live in the communities served by rural hospitals. This included both the Medicare payments to the rural hospitals under the global budget and payments to any other hospitals that provide services to the residents of the rural hospital’s service area, regardless of where those other hospitals are located. Pennsylvania was expected to achieve a cumulative total of $35 million in Medicare savings on hospital services for residents of the rural hospitals’ service areas by the end of the project. “Savings” were calculated by comparing what Medicare actually spent on hospital services to a projection of what would have been spent if spending had increased at the rate that Medicare hospital spending increased in rural areas nationally. In addition, the project was monitored to determine whether Medicare spending on all services, not just hospital services, has increased more than in other states.
In order to receive the global budget payments, hospitals were required to prepare a “Rural Hospital Transformation Plan,” which had to be approved by both the state and CMMI. CMMI provided $25 million in grant funding to the state to create a Rural Health Redesign Center Authority to oversee the program, but there was no funding for the individual hospitals.
The Pennsylvania Rural Health Model (PRHM) was not a permanent program. Changes in Medicare payment ended after the 6-year period.
The hospital global budgets were originally supposed to begin in January 2018, but due to difficulties in recruiting hospitals to participate, the first hospitals did not begin participating until 2019. The Pennsylvania Rural Health Redesign Center Authority was supposed to be established by January 2018, but the Pennsylvania General Assembly did not enact the enabling legislation until November 2019.
How Global Budgets Worked in Pennsylvania
The global budgets used in the Pennsylvania Rural Health Model worked very differently from those in Maryland:
Budgets were Payer-Specific, not truly “Global.” In Maryland, hospitals have a single global budget for their inpatient and outpatient revenue from all payers, and each payer’s share of the budget may differ from year to year depending on how many of that payer’s members received services during the year and what kinds of services they received. In Pennsylvania, a hospital had a separate budget amount for each payer, and there was no requirement that those budgets change in proportion to the relative numbers and types of services received by each payer’s insured patients.
Hospitals Received Periodic Budget Payments, Rather Than Fees for Services. In Maryland, hospitals continue to get paid fees for individual services; the global budget is a mechanism for forcing the fee amounts to increase or decrease so that total revenue stays within the global budget amount. In Pennsylvania, Medicare and participating payers no longer paid fees to a participating hospital for individual services delivered; instead, they paid the hospital a predetermined amount regardless of the number of services the hospital delivered to patients insured by that payer.
Pennsylvania Had No Authority to Ensure Budgets Are Adequate to Support Costs of Services for Insured and Uninsured Patients. In Maryland, the HSCRC has the power to regulate the amounts that every payer, including Medicare, pays each hospital for its services, and it can use that power to ensure that a hospital’s total revenue is adequate to support the costs of services, including the costs of serving uninsured patients, and that each hospital receives revenues equal to its global budget. Although the Pennsylvania Rural Health Redesign Center Authority was supposed to determine what the global budgets for hospitals should be, it could not force Medicare or any health insurance plan to pay hospitals based on those budgets.
Not All Pennsylvania Hospitals Were Eligible to Participate. In contrast to Maryland, where all hospitals are required to participate in the global budget system, participation in the Pennsylvania Rural Health Model was limited to hospitals in counties designated as “rural” by the Center for Rural Pennsylvania.
Participation by Hospitals in Pennsylvania was Voluntary. Whereas all hospitals in Maryland are required to be paid under a global budget, participation in the Pennsylvania Rural Health Model was voluntary, and continued operation of the program was contingent on a minimum number of hospitals agreeing to participate. The agreement between CMMI and Pennsylvania required that a minimum of 6 hospitals participate in the program during the first year and that a minimum of 18 hospitals participate during the second year. However, only 5 hospitals agreed to participate in the first year and only 13 hospitals signed up for the second year (2020), even though a total of 67 hospitals were eligible to participate (two of the eligible hospitals closed since the program was first created). Four additional hospitals agreed to participate in 2021.
Participation by Payers in Pennsylvania was Voluntary. In Maryland, all payers are required to participate in the global budget structure, but payer participation in the Pennsylvania Rural Health Model was voluntary. Not all commercial plans in the state participated, including several large national payers. The agreement between CMMI and Pennsylvania required that at least 90% of hospitals’ revenues come from payers who are participating in the program, but no information has been released as to whether that has happened.
Patient Cost-Sharing Was Not Controlled in Pennsylvania. Maryland regulates the amounts paid by all payers, which includes the prices charged to individual patients who do not have insurance; moreover, by regulating the prices charged to insurance companies, Maryland also indirectly controls the cost-sharing amounts paid by insured patients. However, in Pennsylvania, the amounts that Medicare and other payers paid the hospital under the global budget represented only the insurer’s share of the payment for services. The hospital still billed for individual services, and patients were still required to pay their share of those bills –patients without insurance were responsible for 100% of the hospital’s charge, and patients with insurance were responsible for the cost-sharing required under their insurance plan.
Because of these differences, the impacts of the Pennsylvania Rural Health Model on hospitals, patients, and payers were very different from the impacts seen under the Maryland system. For example:
In Pennsylvania, a hospital’s total revenue would still increase or decrease based on changes in the volume of services delivered to patients whose insurance plans are not participating in the model. If a hospital delivered fewer services to these patients, the hospitals would experience financial losses.
In Pennsylvania, a participating payer could unilaterally reduce the size of its global budget at a hospital regardless of whether patients were receiving fewer services, and it could refuse to increase the size of the budget even if the hospital’s costs had increased for reasons beyond its control. A payer whose membership decreased in the community served by a hospital could decide to reduce the budget amount it contributed, while a payer that had an increase in membership could refuse to increase its contribution. These kinds of changes could lead to financial losses at participating hospitals.
In Pennsylvania, a hospital could still increase its total revenue by increasing the amounts it charges patients for services, since there is no global budget for the revenues the hospital receives directly from patients. Pennsylvania does not regulate the prices hospitals charge, and an insurance plan participating in the global budget program would no longer have any reason to negotiate the amounts paid for individual services because the insurance company is paying the same amount in total regardless of what the hospital charges for individual services. Consequently, patients could pay significantly more for services than they did prior to use of the global budget regardless of whether the volume of services decreases.
In Pennsylvania, if patients began going to non-participating hospitals to receive services instead of participating hospitals, the hospitals delivering the services would receive more revenue, since those hospitals would be paid through standard fees for services.20 Since the Pennsylvania Rural Health Model was required to limit the growth in total Medicare hospital spending, an increase in the number of services delivered at non-participating hospitals would mean that the global budgets at the participating hospitals had to be reduced, potentially causing financial losses for the hospitals.21
In addition to the above differences, the Pennsylvania Rural Health Redesign Center Authority was funded entirely with federal funds under a grant from CMMI, whereas the HSCRC in Maryland is funded through an assessment on the hospitals in the state. Although the Pennsylvania General Assembly enacted legislation creating the Pennsylvania Rural Health Redesign Center Authority, it did not appropriate any state funds to support it nor did it provide any other mechanism for it to generate funding. Consequently, there is no assurance that it will continue operating after the federal grant funds run out.
How Global Budgets in Pennsylvania Are Set
In the first year that a hospital participated in the Pennsylvania Rural Health Model, its global budget payment from Medicare was determined using a simple formula. The global budget was supposed to be equal to the greater of: 1) the hospital’s Medicare revenue from the most recent fiscal year for which complete claims data are available or 2) the average of the revenue in the three prior years. Although there was a presumption that a similar methodology will be used by other payers, there was no requirement that they do so.
Even if a hospital had been losing money with current fee-for-service or cost-based payment amounts, there was no explicit provision for increasing the initial global budget amount to ensure it is adequate to cover the cost of delivering services at the hospital. The presumption was that the flexibility provided by the global budget would enable the hospital to modify its services in some fashion to reduce its costs without harming the quality of care for patients.
Most payment model demonstrations developed by the CMS Center for Medicare and Medicaid Innovation have set the initial payment amounts for participants at a level below the amount they would otherwise have expected to receive in order to produce savings for the Medicare program. Presentations by CMMI about the global budget concept in Pennsylvania indicated that some kind of “discount” would be applied to the global budget payments, either initially or after several years, in order to reduce spending for payers, so depending on the amounts and timing of these reductions, they could potentially create financial losses for hospitals that had not had losses to date and they could increase current losses rather than reduce them.
In subsequent years, the hospital’s global budget amount for Medicare was to be determined by adjusting the prior year’s budget for inflation, demographic shifts, service line changes, shifts in patient volume between hospitals, the hospital’s performance on quality measures and population health outcome measures, expected reductions in potentially avoidable admissions, and other factors. However, no details on how these adjustments were made have been publicly released, so it is unclear whether and how it will differ from the Maryland methodology.
There was a provision in the Pennsylvania Rural Health Model for increasing a hospital’s global budget amount from Medicare in later years if (1) there had been a reduction in Medicare’s total spending for patients living in the hospital’s service area and (2) the overall program had been successful in achieving at least two of three population health goals: a) increasing access to primary and specialty care, b) reducing rural health disparities through improved chronic disease management and preventive screenings, and c) decreasing deaths from substance use disorder and improving access to treatment for opioid abuse. However, there was no explicit mechanism for increasing the global budget amount to provide the participating hospitals with additional resources to achieve those goals. Here again, there was an implicit presumption that the flexibility provided by the global budgets would enable participating hospitals to reallocate their resources in a way that would result in better outcomes.
Hospital Participation in the Pennsylvania Rural Health Model
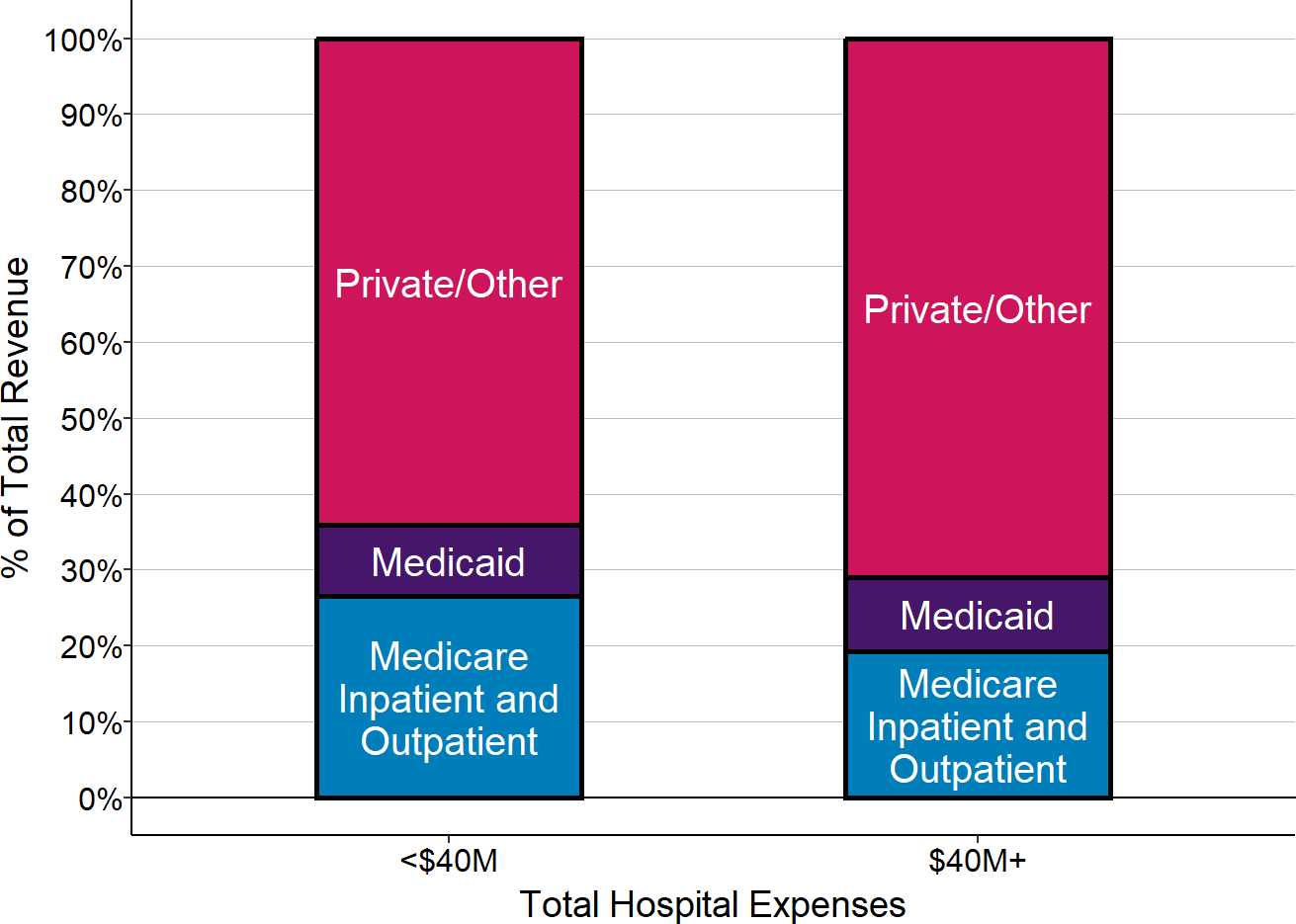
Most of the hospitals that agreed to participate in the Pennsylvania Rural Health Model were not small, rural hospitals. Because the program defines “rural” differently than other federal programs, nearly one-third (5) of the 18 hospitals participating were not classified as rural hospitals under standard CMS or HRSA definitions, and some hospitals that were classified as rural under federal standards were not eligible to participate in the Pennsylvania program. Of the participating hospitals that were located in rural areas, two-thirds had total expenses of more than $45 million, and one-third had total expenses of $100 million or more. Only 4 hospitals were the kinds of small rural hospitals that are having the most serious problems nationally.
The four small rural hospitals that participated in the program had been losing money when they agreed to join, but the primary causes of the losses differed from those experienced by small rural hospitals in other parts of the country. The losses for the four small rural hospitals in the Pennsylvania Rural Health Model were primarily coming from low Medicaid payments and patient bad debt (which likely represents either uninsured or underinsured patients). Unlike most small rural hospitals across the country (and unlike other small rural hospitals in Pennsylvania), the majority of the small rural hospitals that were participating in the Pennsylvania program had not been losing money on their private pay patients. Since the Pennsylvania program is not designed to increase Medicaid payments and since private payers appear to already have been paying more than the cost of services at most hospitals, it not clear how the global budget payments in the program would help the hospitals reduce their financial losses. The most recent data available indicate that the majority of the hospitals were still losing money despite participating in the program.
Figure 6
Components of Total Margin at Small Rural Hospitals
Participating in the Pennsylvania Rural Health Model
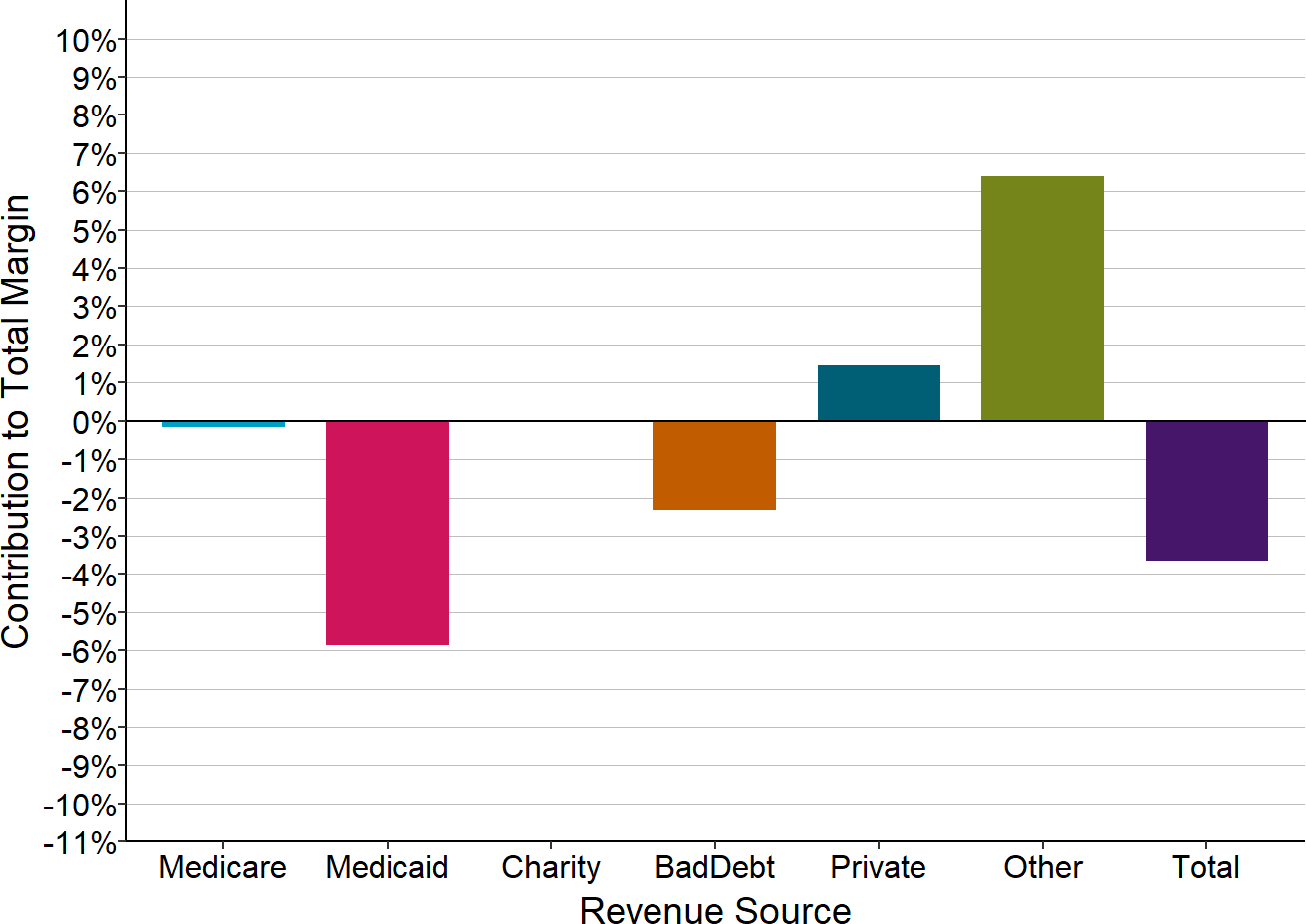
Median for most recent year available (2023 or 2024). Margin for payer is divided by hospital’s total expenses. Includes only rural hospitals with less than $45 million total expenses that were participating in the PA Rural Health Model in 2024.
The CMS CHART Model
In August 2020, the CMS Center for Medicare and Medicaid Innovation (CMMI) announced the “Community Health Access and Rural Transformation (CHART) Model.”22 The “Community Transformation Track” of the CHART Model included a component in which rural hospitals could be paid by Medicare, Medicaid, and potentially other payers through a global hospital budget approach.23 A Notice of Funding Opportunity (NOFO) for the Community Transformation Track was issued on September 15, 2020.24 In September of 2021, CMMI selected 4 states - Alabama, South Dakota, Texas, and Washington - as sites to implement the Community Transformation Track.
In February 2023, CMMI announced that it was terminating the Community Transformation Track (and thereby the entire CHART Model) because rural hospitals were unwilling to participate. 25
The CHART Community Transformation Track had some similarities to the Pennsylvania Rural Health Model, but it also differed in significant ways.
How Rural Hospitals Would Have Been Paid in the CHART Model
Eligibility Criteria for Rural Hospitals
Rural hospitals were only eligible to participate in the Community Transformation Track of the CHART Model if they provided services to residents in one of 15 rural “Communities” across the country. The Communities were selected by CMMI based on applications submitted by state Medicaid agencies and other eligible “Lead Organizations.”26
A Community had to consist of one or more counties or census tracts, all of which are classified as rural by the Federal Office of Rural Health Policy. A Community needed to be relatively large, since its counties and census tracts would collectively need to have at least 10,000 Original Medicare beneficiaries living within them.27 Most Communities would likely have needed to have total populations of more than 60,000 total residents in order to qualify.28 Medicare beneficiaries who are enrolled in Medicare Advantage plans did not count toward the 10,000-beneficiary minimum, so Communities had to be larger in rural areas that had a high penetration of Medicare Advantage plans.
A rural hospital was eligible to participate in the CHART Model if either:
- it was located in one of the selected Communities and received at least 20% of its Medicare revenue from eligible hospital services provided to residents of that Community; or
- regardless of where the hospital is physically located, it delivered services representing at least 20% of the amount Medicare spends on eligible hospital services for all Medicare beneficiaries living in the Community.
In other words, either the residents of the Community had to represent a large share of the hospital’s services, or the hospital had to deliver a large share of the hospital services the residents of the Community received.
In addition, in order to participate in the CHART Model, the hospital had to agree to implement activities described in a Transformation Plan developed by the Lead Organization and to report quality and other information to CMMI.
The eligibility criteria precluded most rural hospitals from participating individually. Only 16% of rural hospitals are located in a county that has 10,000 or more residents on Original Medicare, and less than 10% of small rural hospitals are located in such a county. This means that in most cases, multiple counties would have to be included and two or more hospitals would have to agree to participate in order for a Community to qualify.
Figure 7
Number of Rural Hospitals Located in Counties With More or Less Than 10,000 Medicare Beneficiaries
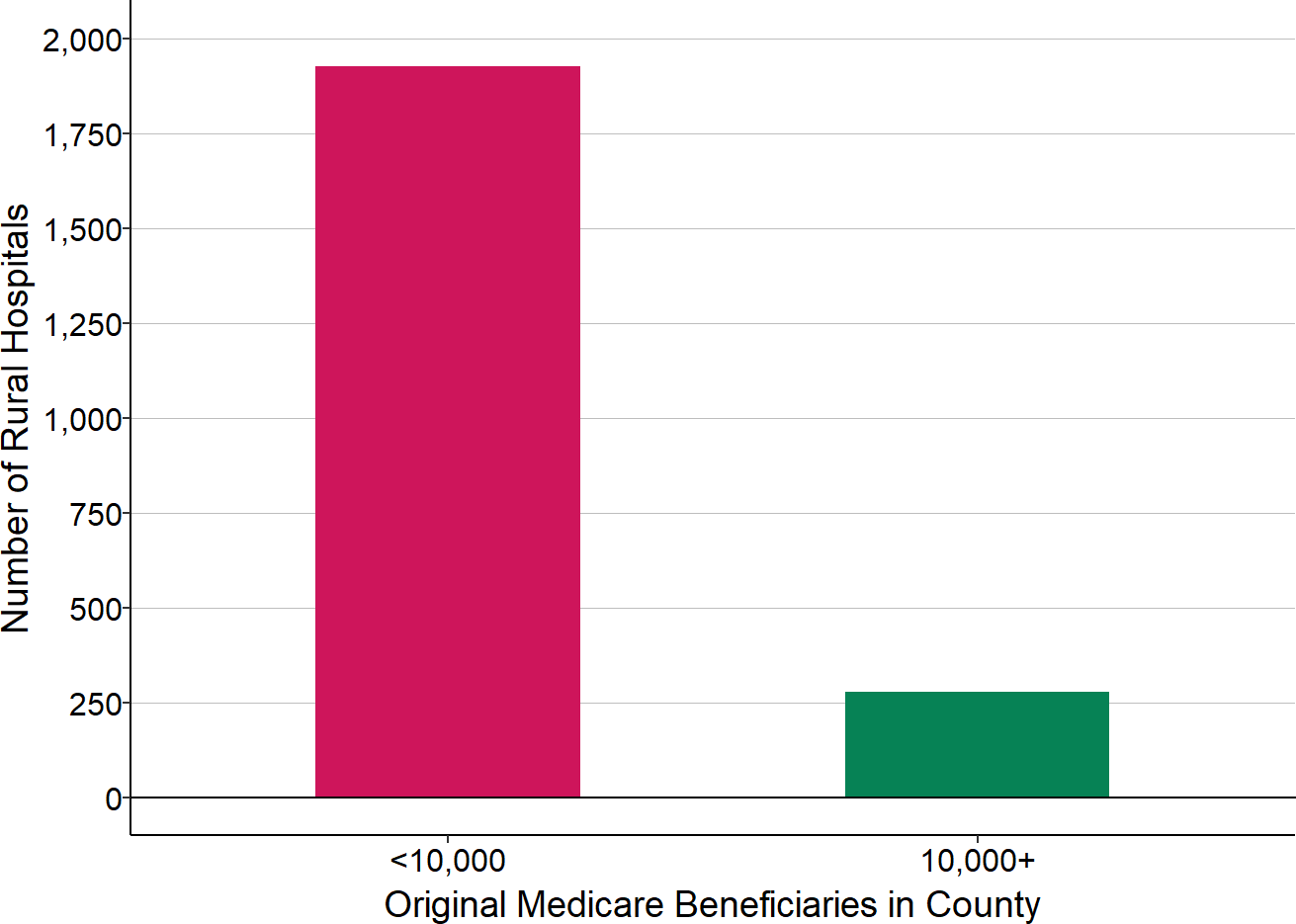
Source: CMS Geographic Variation Public Use File and Provider of Services File
Over 70% of small rural hospitals (those with less than $30 million in total expenses) are located in counties with fewer than 4,000 Medicare beneficiaries, and more than 40% are in counties with fewer than 2,000 beneficiaries, so this means that 3, 4, 5, or even more small hospitals would have all needed to be part of the same Community in order for any of the small rural hospitals to be eligible.
Figure 8
Number of Medicare Beneficiaries in Counties Where Small Rural Hospitals Are Located
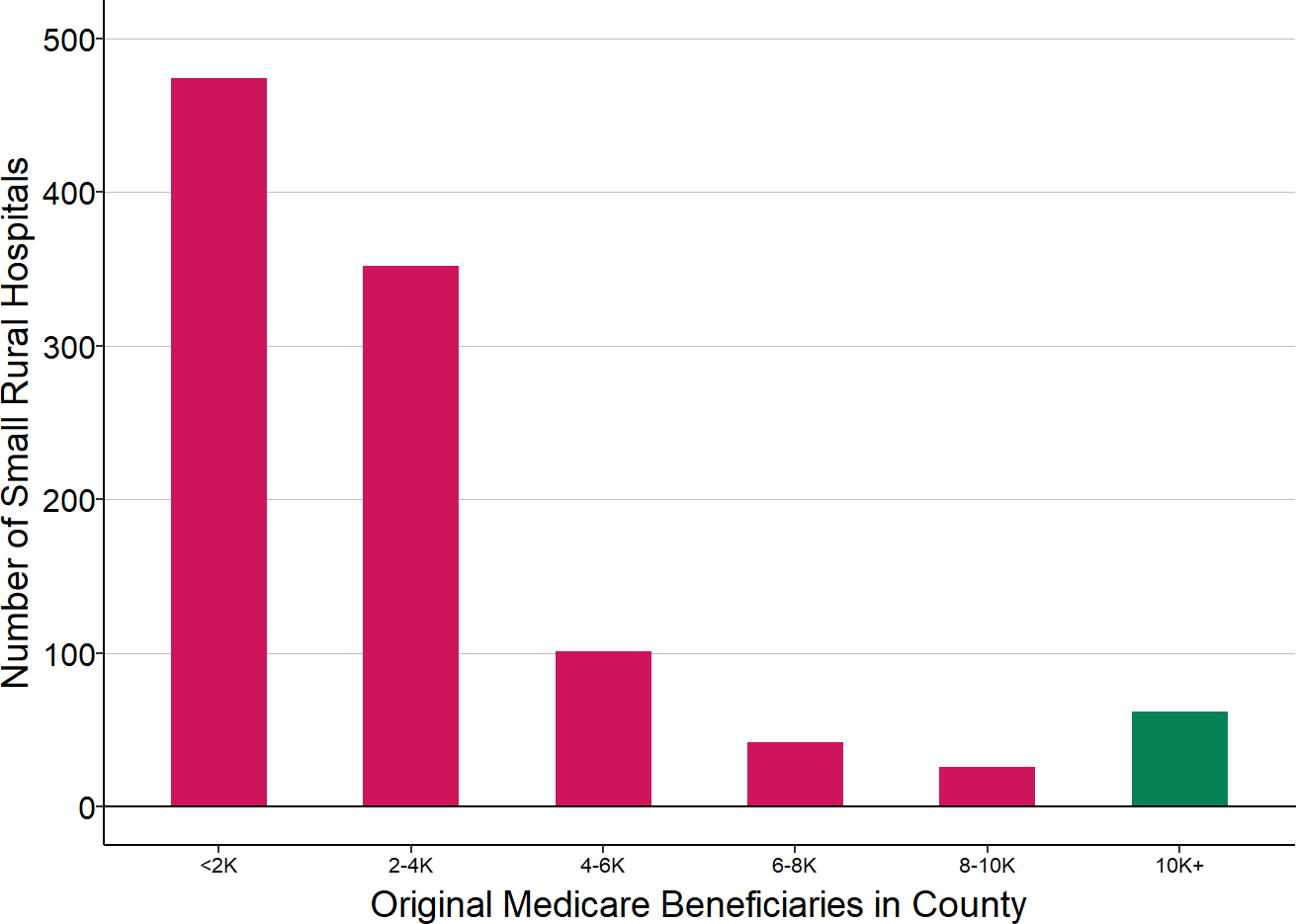
Source: CMS Geographic Variation Public Use File and Provider of Services File. Small rural hospitals are those with less than $45 million in total expenses in the most recent year for which financial data are available. K = 000s
Method of Payment for Inpatient and Outpatient Services
If the hospital met the eligibility criteria and wished to participate in the CHART Model, the hospital would have received a single, predetermined Capitated Payment Amount (CPA) each month. This would have served as the hospital’s full payment for the eligible inpatient and outpatient services it delivered to Medicare beneficiaries. The hospital would no longer receive standard Medicare payments for these services, i.e., Critical Access Hospitals would no longer receive cost-based payments, and other hospitals would no longer receive DRG-based payments for inpatient admissions or payments under the Outpatient Prospective Payment System (OPPS) for outpatient hospital services.
The Capitated Payment Amount would have applied only to (1) inpatient hospital services, (2) outpatient hospital services, and (3) inpatient rehabilitation services that are delivered in swing beds at Critical Access Hospitals. There would have been no change in the way a rural hospital was paid for physician services and other professional services, Rural Health Clinic services, swing bed services at non-Critical Access Hospitals, home health services, hospice services, ambulance services, or inpatient rehabilitation services outside of swing beds. It was not clear whether the CPA would only apply to hospital services delivered to beneficiaries who resided in the community, or whether it would have also replaced standard Medicare payments for services delivered to beneficiaries who do not live in the Community.29
The CPA amount would have been the same each month regardless of how many or what types of inpatient or outpatient services the hospital provided to residents of the Community during the month. For example, if the hospital admitted fewer Medicare beneficiaries for inpatient care in a particular month, it would have still received the same CPA amount as it received in the previous month, and if it delivered more outpatient testing to Medicare beneficiaries, it would not have received any additional payments from Medicare. However, as described below, the amount of payment in future years would have changed based on how what proportion of the total hospital services in the Community the hospital delivered.
Determination of the Capitated Payment Amount
Obviously, the impact of the CHART Model on a rural hospital’s finances would have depended heavily on how large the Capitated Payment Amount was compared to the payments the hospital would have otherwise received. In the Notice of Funding Opportunity, CMS described the methodology it would use to determine the Capitated Payment Amount, although it stated that the description was “for informational purposes and may change at CMMI’s sole discretion” and that “the final CPA financial methodology will be detailed further in a time and manner to be specified by CMMI.”30
Payment Amount in the First Year
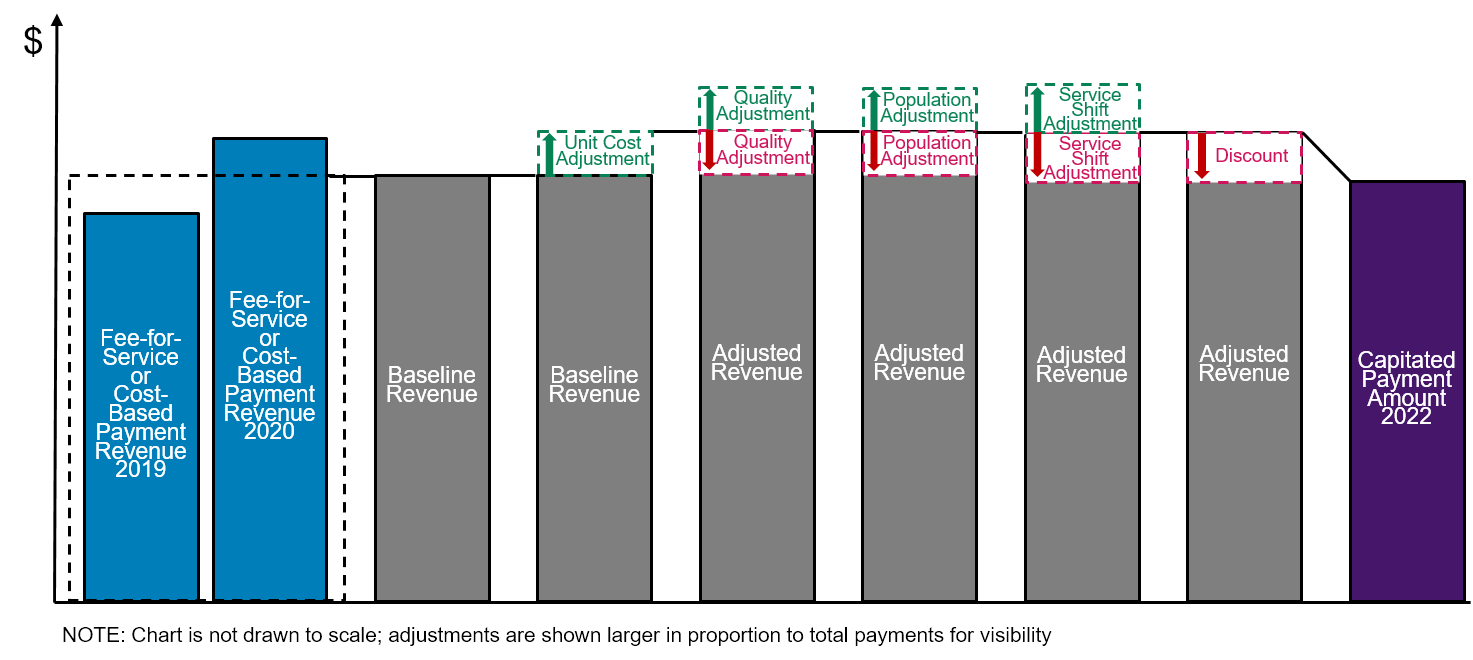
The Capitated Payment Amount (CPA) in the first year of the CHART Model was to have been determined through a complex series of steps:
- The hospital’s “baseline revenue” is calculated. The amounts Medicare paid the hospital for eligible inpatient and outpatient services two years and three years prior to the start of the model would be determined and averaged. (Because of the impacts of the pandemic, CMS announced that initally, the baseline revenue would be the average of the Medicare payments to the hospital during 2018 and 2019. )31
- A “unit price adjustment” is made. The baseline revenue reflected the amounts paid for services 2-3 years in the past, but the costs of delivering individual services and the amounts Medicare pays for services would have changed between that period and the year in which the Capitated Payment Amount is paid. The unit price adjustment was presumably intended to address this. The adjustment was to be calculated differently for Critical Access Hospitals and other hospitals:
- Critical Access Hospitals. According to the CMS methodology, “the unit price adjustment consists of the change in the interim payment rate between the cost report that the Critical Access Hospital (CAH) submitted for the baseline years and the most recently available, adjudicated cost report.”32 It is not clear exactly what “payment rate” was being referred to, since a CAH is paid for inpatient services using a per diem rate and it is paid for outpatient services based on a cost-to-charge ratio applied to the charges for services. The most recently available cost report available when the rate is initially set would likely be the later of the two baseline years (e.g., since the payments for 2023 would need to be determined in 2022, the most recent adjudicated cost report would be for 2021). There was a provision for adjusting the Capitated Payment Amount mid-year if a more recent cost report has been filed and adjudicated.
- Other hospitals. For hospitals paid through the Inpatient Prospective Payment System and Outpatient Prospective Payment System, there were two components to the unit price adjustment. (The Notice of Funding Opportunity did not describe exactly how these two components would be combined or used to adjust the baseline revenue.)
- Geographic Adjustment Factor. The changes in the wage index and capital geographic adjustment factor applicable to the hospital would be used to adjust the inpatient and outpatient portions of the baseline revenue.33
- Trend. In addition, an adjustment would be made based on the “expected” percentage change in national Medicare FFS expenditures from the baseline period to the year in which the payment will be made. This would not really be a “unit price” adjustment, since the change in total expenditures is a function of not only changes in the prices of services but in the volume and mix of services delivered to Medicare beneficiaries. Because the Capitated Payment Amount was to be set prior to the beginning of the year, the actual national Medicare spending amount for the year would not be known, so it would have to be estimated by CMS. According to the methodology description, “If the observed regional trend differs from the projected national trend by more than three percentage points, CMS may retrospectively update the trend at the time that end-of-year adjustments are made,” which presumably means that the CPA could be increased or decreased after the year ends depending on how accurate the estimate of spending was.34 It is not clear what exactly was meant by “the regional trend” or what adjustment would be made if there was a difference of more than three percentage points.
- Adjustments are made for quality. The payment would have been adjusted for any changes in the penalties applicable to the hospital under the CMS Value-Based Purchasing Program, the Hospital Acquired Condition Reduction Program, and the Hospital Readmissions Reduction Program between the baseline years and the current year. Since these programs only apply to inpatient services, not outpatient services, presumably the adjustment would have only appled to the subset of the baseline revenues derived from inpatient services.
- Adjustments are made for changes in the population served. This would have included three separate components:
- Population size adjustment. The population served was to be defined as the number of Original Medicare beneficiaries who “reside” in the Community for the majority of the 12 month period35 that began 18 months prior to the year in question (i.e., either the baseline years or the current year) times the number of months they are there.36 The number of beneficiaries in the community in the baseline years would have been compared to the number in the current year, and the CPA would be adjusted based on the change in the number of beneficiaries. The methodology did not specify exactly what the adjustment would be, but presumably if the number of beneficiaries had increased or decreased by a certain percentage, the CPA would be increased or decreased by the same percentage. (The document stated that “the population adjustment will avoid over-payment for Eligible Hospital Services by reducing revenue from a Participant Hospital’s baseline CPA if the population served by the Participant Hospital decreased between the baseline years and the Performance Period.”37)
- Demographic adjustment. The demographic-only HCC scores of the population in the two time periods were to be compared to determine whether the population had increased in age or the gender mix had changed.38 The methodology did not specify whether the CPA would be adjusted in direct proportion to the change in the average HCC score.
- Shift in eligible hospital services. The third adjustment was to be based on whether there had been a “change in the distribution of services between hospitals.” The method of calculating this was not specified, but the document stated the adjustment was intended to “avoid over-payment for Eligible Hospital Services by reducing revenue from a Participant Hospital’s baseline CPA if … Eligible Hospital Services shifted between health care providers between the baseline years and the Performance Period,” so presumably this meant that if the residents of the community received a higher proportion of their hospital services at other hospitals, the CPA for the rural hospital would be reduced.39
- A “discount” is applied. After all of the other adjustments had been made, the resulting amount would be reduced by a percentage that CMS referred to as the “discount.” The discount in the first year was 0.5% (i.e., one-half of one percent). The document stated that the discount was included “in order for payers to realize savings.”40
- Mid-year adjustments are made. The Capitated Payment Amount was to be adjusted mid-year if additional data became available about changes in the population served or if a newly adjudicated cost report for a Critical Access Hospital became available.
- Additional adjustments are made after the end of the year. Although the Capitated Payment Amount was supposed to be a “prospective payment,” it was to be retroactively adjusted six months after the end of the year based on claims data. In addition to the population adjustments described above, the NOFO said there “may” be an option for the hospital to receive an “outlier adjustment” to address “unexpected, catastrophically expensive utilization.” If CMS concluded that the Capitated Payment Amounts paid to the hospital had been too high, CMS would reduce the CPA to the hospital in the next year or potentially require a lump-sum repayment of the difference.41
The final Capitated Amount could be higher or lower than revenues in previous years depending on the relative magnitudes of the various adjustments.
Figure 9
Methodology for Determining the Initial Capitated Payment Amount in the CMS CHART Model
Payment Amount in Subsequent Years
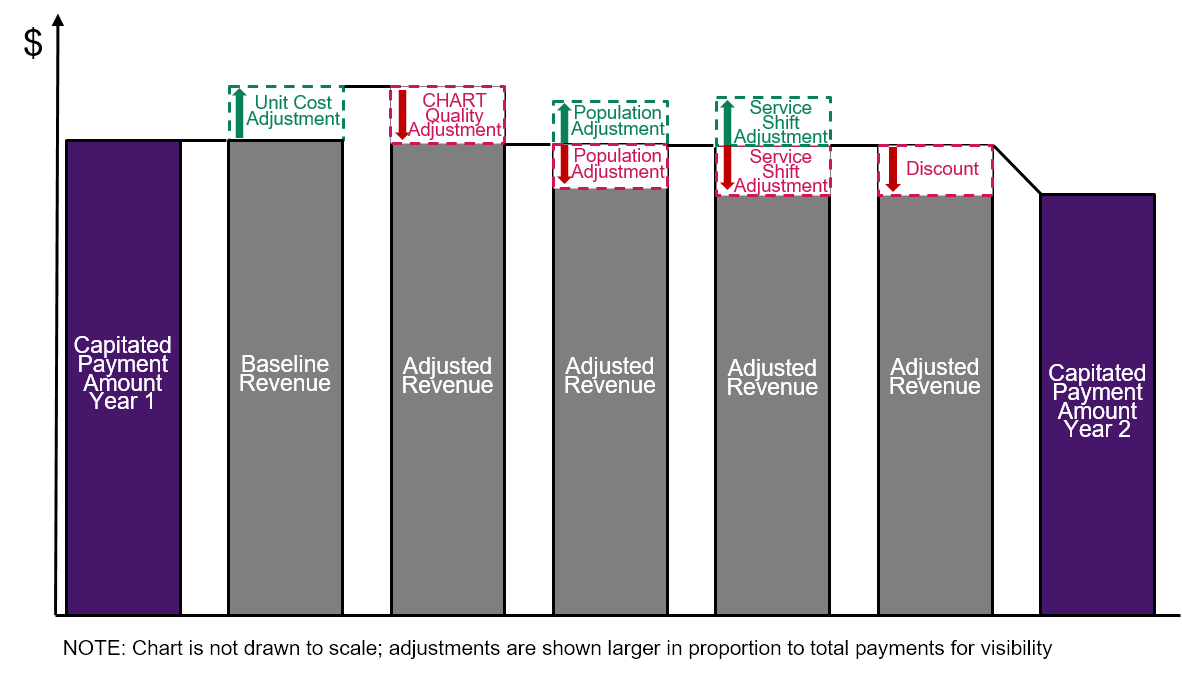
In subsequent years, the methodology for determining the Capitated Payment Amount was to be similar to what is described above, but with three changes:
- The adjustments for changes in unit prices, population size, demographics, and service use would be applied to the Capitated Payment Amount from the previous year. The initial CPA was based on the average of the amount of fee-for-service or cost-based payments the hospital received in prior years. However, in the second and subsequent years, the current CPA would serve as the starting point for determining the next year’s CPA using all of the various adjustments described above.
- Additional reductions in payments would be made based on quality measures. In addition to the adjustments based on current CMS hospital quality programs described above, the CPA was to be reduced by up to 2% based on quality measures specifically defined for the CHART program.42 The quality adjustment would be based on a hospital’s performance on six measures, three of which would be required for all hospitals (per capita hospital admissions for chronic conditions, the all-cause readmission rate, and HCAHPS patient experience ratings), and an additional three that would be selected by the Lead Organization from a menu of seven measures (use of pharmacotherapy for opioid use disorder, use of high dosage opioids for non-cancer patients, the rate of Cesarean sections, the rate of post-partum contraceptive care, the rate of flu vaccination, screening and follow-up plan for depression, and continuity of primary care for children with medical complexity). It is not clear what would have been considered good or bad performance by a small rural hospital on these measures; most of the measures on the second list would have relatively small denominators and would be difficult or impossible to measure reliably in small rural communities.43
- Payments would be reduced by larger amounts each year through higher discounts.
- A 1% discount in Year 2. In the second year of the program, the CPA was to be reduced by 1.0% rather than 0.5%.44
- Discounts as high as 2.5% in Year 3. In the third year, the amount of the discount was to range from 1.0% to as much as 2.5% depending on the total amount Medicare was paying through Capitated Payments for services in the Community. If the total of the CPA payments to all participating hospitals in the Community was less than or equal to $15 million, all of the payments were to be reduced by 2.5%. If the total CPA payments were higher than $15 million, smaller discounts were to be used, with a minimum discount of 1% for communities where $120 million or more of CPA payments were being made. The document stated that the higher discounts were intended to provide “an incentive for Communities to recruit more hospitals to participate” and to increase “the likelihood that the [program] will yield savings that meet or exceed” the amount of the grant funding that is being provided to the Community as part of the CHART model.45
- Maximum discounts between 3% and 4% in Years 4 through 6. In subsequent years, the maximum discount was to increase to as much as 4%, and the threshold for receiving only a 1% discount was to increase to $300 million in total CPA payments.
Figure 10
Methodology for Determining the Second Year Capitated Payment Amount in the CMS CHART Model
Payments from Other Payers
The state Medicaid agency was required to participate and serve as an “Aligned Payer” in order for a Community to be selected. However, Medicaid payments did not need to change until the second year of the program. Moreover, only 50% of the participating hospitals’ Medicaid revenue needed to be paid through a Capitated Payment Arrangement in the second year; that percentage was to increase to 60% in the third year and 75% in the fourth and subsequent years. The document did not say whether these percentages would apply to all Medicaid revenues or only the revenue for services delivered to residents of the Community.46
Participation by commercial payers as Aligned Payers was “recommended but not required,” and there was no requirement for Medicare Advantage plans to participate, so it is possible that payments would have only changed for Original Medicare beneficiaries and a portion of Medicaid beneficiaries.47
The payment methodology used by Medicaid and other Aligned Payers was supposed to be “similar” to the Medicare methodology, but it did not need to be identical. The NOFO stated that an “Aligned Payer may implement their capitated payment arrangement with Participant Hospitals differently based on their plan benefits and member populations.”48 The NOFO specifically stated that other payers did not need to make adjustments for Critical Access Hospitals based on changes in the hospitals’ costs.49
The Impact of the CHART Model on Rural Hospitals
The complexity of the payment methodology made it difficult for a rural hospital to understand what impact participation in the CHART Model would have. However, careful examination shows that:
- Rural hospitals would have been paid less for services under the CHART Model than under current payment systems.
- Payments to rural hospitals under the CHART Model would still have been based on the volume of services delivered.
- Hospital costs and losses would have increased under the CHART Model. Hospitals would have still lost money if they reduced avoidable services such as unplanned hospital readmissions or Emergency Department visits.
Rural Hospitals Would Have Been Paid Less for Services Under the CHART Model
Most rural hospitals are losing money on the services they deliver to patients because the payments they receive from Medicare, Medicaid, and private health insurance plans are less than what it costs for the hospitals to deliver the services. The CHART Model would not only have failed to solve this problem, it would have made it worse, because it was explicitly intended to reduce the amount that payers spend.
Capitated Payments Would Have Been Reduced Below Current Inadequate Levels. The “discount” in the methodology reduced the Capitated Payment Amount below what the hospital would have received under current payment systems. At most rural hospitals, payments from Medicare and other payers are below the cost of services, so if the Capitated Payment was even lower, the hospitals’ losses would have increased.50
Payment Reductions Would Increase Over Time. The discount in the first year was 0.5%, and it would have doubled to 1% in the second year. It would have doubled again to 2.0% or more in the third year for most hospitals,51 and it would have continued to increase by smaller amounts in each subsequent year to as much as 4.0% in the sixth year. In addition, beginning in the second year, a new quality adjustment would have been added that could have reduced payments by as much as 2% below the discounted amount. As a result, the hospital could receive less revenue during the demonstration than it received prior to entering.
Figure 11
Increasing Reductions in Capitated Payment Amounts Over Time
in the CMS CHART Model
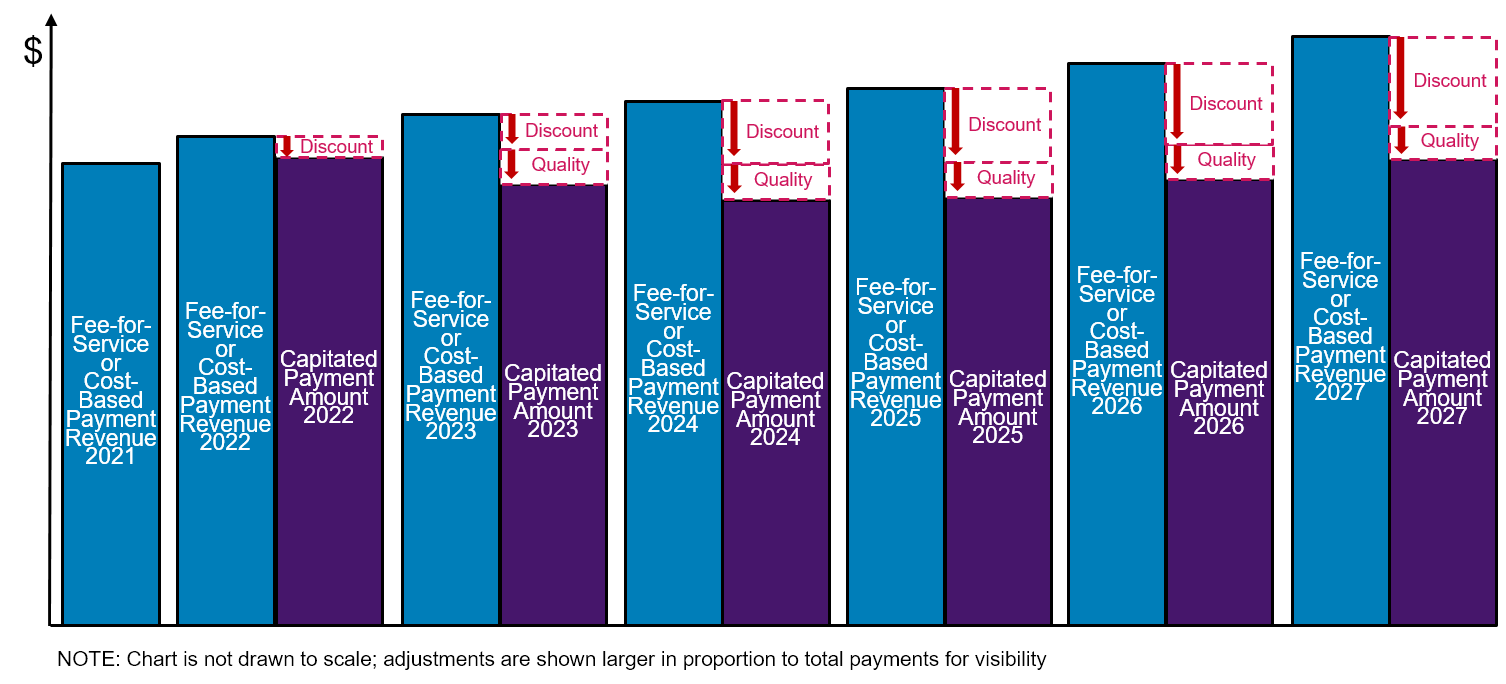
- Payment Reductions Would Have Been Larger for Smaller Rural Hospitals and Smaller Rural Communities. The size of the discount would have been based on the total amount of Medicare revenue included under the Capitated Payment Arrangement in a Community. The percentage reduction in payment to the hospital would be larger if the total amount of Medicare revenue involved was smaller. In the sixth year of the program, the Capitated Payment Amount was to be reduced by 4% if the hospitals in the Community received less than $15 million in Medicare payments for the services covered by the Capitated Payment Amounts, and the discounts would only have been 2% or less if there were more than $160 million in total Capitated Payments in the Community. As noted earlier, CMS stated that the higher discounts were intended to provide “an incentive for Communities to recruit more hospitals to participate” and to increase “the likelihood that the [program] will yield savings that meet or exceed the amount of the cooperative funding.” However, 72% of rural hospitals receive less than $15 million per year in Medicare payments for inpatient and outpatient services, and the majority of rural hospitals have less than $10 million in Medicare revenue, so a large number of hospitals would have had to participate in a Community in order to qualify for smaller discounts.
Figure 12
Total Medicare Inpatient and Outpatient Revenue
at Rural Hospitals
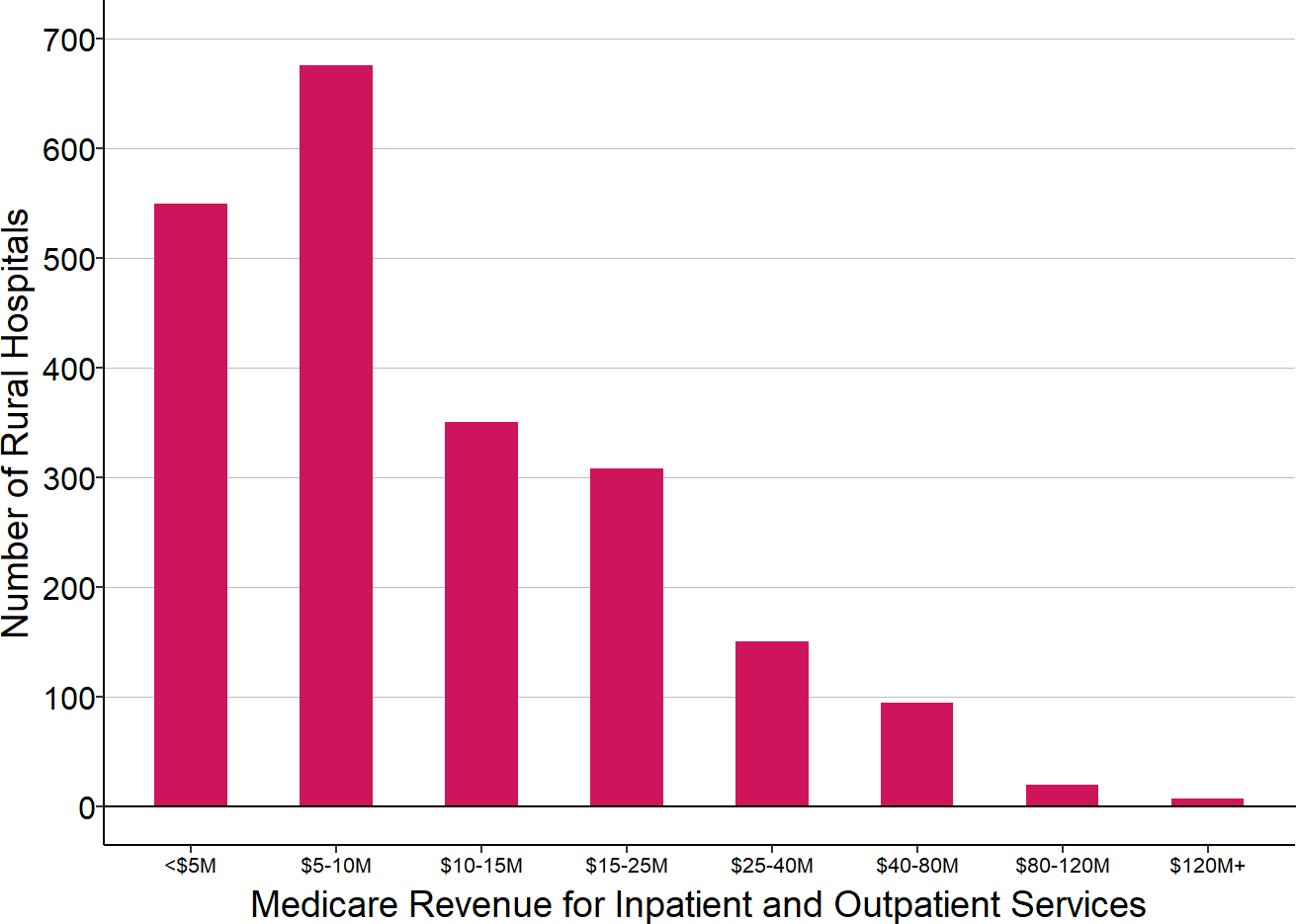
Amount in most recent year at U.S. rural hospitals.
- Payments for Critical Access Hospitals Would Have No Longer Increased When Costs Increased During the Year. Most small rural hospitals are classified as Critical Access Hospitals; currently, if their costs increase unexpectedly during the year, their cost-based payments from Medicare increase proportionately. For example, if one of the hospital’s emergency physicians or nurses resigns or becomes ill and the hospital has to pay more for a temporary employee to fill the gap, the increase in the hospital’s personnel cost that year will result in a higher Medicare payment for that year. Under CHART, however, the Capitated Payment Amount for the year would not have increased if the hospital’s costs increased unexpectedly during the year, resulting in lower revenues and higher losses under CHART than under the current payment system.
Hospital Payments Would Still Have Been Based on the Volume of Services
CMS said that the CHART Model payments would have provided “a predictable and stable revenue stream” and that hospitals’ revenues would no longer be “predicated on realized volumes.” However, most of the hospital’s revenue would still have come from fee-for-service payments, and even the Capitated Payments would still have been tied to the number of services delivered.
- Payments Would Not Have Changed at All for Most of the Hospital’s Services.
- Medicare: Although Medicare is a large payer at most rural hospitals, it does not represent the majority of revenues at most hospitals. Moreover, the Capitated Payment Amount would have applied only to inpatient hospital services and outpatient hospital services. Medicare would have continued to pay for physician services and other professional services, Rural Health Clinic services, swing bed services at non-Critical Access Hospitals, home health services, hospice services, ambulance services, and inpatient rehabilitation services outside of swing beds using fee-for-service payments. Medicare payments for inpatient and outpatient services only represent about one-third of total revenues at small rural hospitals and less than one-fourth of revenues at larger rural hospitals.
- Medicaid: Although the state Medicaid program was required to participate in the CHART Model in order for a Community to be selected, Medicaid payments were not required to change until the second year, and even then, only 50% of Medicaid payments had to be provided through a capitated payment arrangement. Medicaid revenues only represent about 9-10% of total revenues at small rural hospitals, so if only 50% of Medicaid payments changed, that would affect less than 5% of the hospital’s revenue.
- Private Insurance: There was no requirement that private health plans participate in the program, so under the CHART Model, a hospital would likely have continued to receive fee-for-service payments for most patients with private insurance.
- Total: In combination, it is likely that less than half of a hospital’s revenues would have been provided through Capitated Payments. For Critical Access Hospitals, that would primarily represent a change from cost-based payment, not a shift from fee-for-service payments.
- The CHART Model’s Capitated Payment Would Have Been Reduced if the Population of the Community Decreases. Many rural hospitals have had financial difficulties because population losses in the rural communities they serve have caused a reduction in the number of services they deliver and the associated fee-for-service revenues. The CHART Model would not have prevented these losses of revenue; if the number of Medicare beneficiaries living in the Community decreased, the “population adjustment” in the payment methodology would have reduced the hospital’s Capitated Payment Amount, which would have had the same negative impact on the hospital’s revenues as the loss of fee-for-service revenues. In some cases, the hospital could have been even worse off under the CHART Model, because the Capitated Payment would be reduced when the population decreased even if the number of services delivered did not decrease.
Figure 13
Sources of Revenue at Rural Hospitals
Median amounts in three most recent years (excluding 2020) at U.S. rural hospitals. Private/Other includes Medicare revenues for services other than inpatient and outpatient hospital services.
- The CHART Model’s Capitated Payment Would Have Been Reduced if the Hospital Discontinued a Service Line. Under the CHART Model, if a hospital stopped delivering a particular type of service, the Capitated Payment Amount would have been reduced in the following year. As stated in the Notice of Funding Opportunity, “When Participant Hospitals shut down a service line, they will lose revenue from that service line…”52 The same would have been true if the hospital delivered fewer services and patients obtained those services at another hospital instead; the Notice of Funding Opportunity stated that the Capitated Payment Amount would be reduced “if Eligible Hospital Services shifted between health care providers.” As a result, the hospital would have less revenue to cover the fixed costs of essential services. The only cases in which the hospital could continue to receive the same revenues when it delivered fewer services would be when it reduced avoidable utilization in an existing service line and patients did not go to other hospitals to receive those services.53
Rural Hospital Costs and Losses Would Have Increased Under the CHART Model
The CHART Model presumed that the “financial flexibility” of the Capitated Payment and “operational flexibilities” through regulatory waivers would allow a hospital to “achieve savings … through reductions in potentially avoidable utilization” and would “incent community-based, preventive care.” However, CMS provided no information to support this assertion. In fact, it is unlikely that hospital costs would decrease and more likely that they would increase under CHART. As a result, it is likely that rural hospitals participating in CHART would have experienced greater financial losses than they would otherwise.
- Reductions in Avoidable Utilization Would Cause Financial Losses. In the NOFO, CMS said “it is expected that Participant Hospitals can achieve savings, despite the presence of a discount, through reductions in potentially avoidable utilization.”54 However, at the smallest rural hospitals, staffing is typically at or near the bare minimum needed to deliver essential services, and even if some of those services could be avoided, the hospital could not eliminate any staff or equipment as a result. For example, a small rural hospital with one physician on duty in the ED will still need that physician on duty even if there are fewer visits to the ED. If a hospital reduces the frequency with which patients are readmitted to the hospital, it will not be able to reduce nursing staff on the inpatient unit.55 Although the Capitated Payment would not decrease if there was a reduction in avoidable utilization, the hospital would only be receiving the Capitated Payment for a subset of patients, so fee-for-service revenues would decrease for the remaining patients, causing losses.
- Unavoidable Increases in the Need for Services Would Cause Financial Losses. If the community experienced a natural disaster or an outbreak of a communicable disease that resulted in a significant increase in ED visits, hospital admissions, and delivery of other outpatient services, the hospital might need to bring in additional staff on a temporary basis to provide the care, purchase additional medications and supplies, and even purchase or rent additional equipment. If the community lost primary care providers and more patients came to the Emergency Department to receive care for minor conditions, the hospital might need to increase the number of physicians or nurses in the ED to handle the higher volume of visits. Under the current fee-for-service payment and cost-based payment systems, the hospital would receive additional revenues to help cover these additional costs, but there was no provision in the CHART Model for making adjustments in the Capitated Payment for unavoidable increases in services.
- Elimination of Services Would Cause Financial Losses. The NOFO stated that a hospital receiving Capitated Payments “will be able to focus on more transformational and collaborative strategies, such as converting to a rural emergency medical center or reconfiguring service lines.” Although elimination of a service line could result in a significant reduction in costs at a hospital, the CHART Model would not have allowed the hospital to retain the revenue that it received for services that were no longer offered. Moreover, the hospital would also lose fee-for-service revenue that it had received from other payers for those services. Although it is often assumed that small rural hospitals would be financially better off if they did not have to provide inpatient care, analysis shows that at most rural hospitals, elimination of inpatient services would result in significant financial losses for the hospital as well as loss of access to inpatient care, rehabilitative care, and long-term care for the residents of the community.
- Rural Hospitals Would Have Experienced Higher Costs and Financial Losses in Order to Satisfy CHART Model Requirements. A hospital could only participate in the CHART Model if it agreed to change its services in accordance with a “Transformation Plan” developed by the Lead Organization. The Transformation Plan, which had to be approved in advance by CMMI, had to include expanded use of telehealth and methods of addressing population health disparities, and it also had to address either behavioral health treatment, substance use disorder treatment, chronic disease management and prevention, or maternal and infant health. There was no increase or other adjustment in the Capitated Payment Amount to provide additional resources for delivering these services. In addition, the Capitated Payments would have been reduced by up to 2% based on the hospital’s performance on six quality measures, and a hospital would have had to incur additional costs to track and analyze these measures and to change services in an effort to minimize penalties based on the quality measures. Under the CHART Model, the Lead Organization would be able to receive grants of up to $500,000 per year, and it was permitted to “pass some of the funding directly to Participant Hospitals for investing in and successfully implementing care delivery redesign efforts.”56 However, there was no requirement that the Lead Organization provide any of these funds to the hospitals and it was not clear whether the Lead Organization would have been able to afford to do so or whether the funds it provided would have been sufficient to cover the additional costs at the multiple hospitals that would have been participating; moreover, the grants would only last until the end of the CHART Model demonstration period.
Will a Global Budget Help a Small Rural Hospital?
The Maryland and Pennsylvania programs provide little, if any, useful information about whether global budgets would help or hurt small rural hospitals in other states:
The only small rural hospital in Maryland closed while it was participating in the global budget program, but that may or may not be indicative of what would happen to other small rural hospitals if a similar program were created in their states.
There are only four small rural hospitals participating in the Pennsylvania program, and as discussed in the previous section, these hospitals differ in significant ways from small rural hospitals in other states. Not only is the Pennsylvania program very different from the Maryland model, it has not been operating long enough to draw any conclusions about its impacts, and the impacts that occur during 2020 will not be indicative of what would happen in non-pandemic years.
Factors Affecting the Impact of a Global Budget on a Rural Hospital
The impact of a global budget on a rural hospital will depend on at least six factors:
whether the hospital has been profitable, and which payers and services have contributed profits and losses;
the extent to which the hospital can and should reduce, expand, or modify the types of services it is delivering;
the year-to-year variability in the community’s need for services;
the year-to-year variability in the hospital’s ability to attract and retain staff and the amounts it has to pay for staff, equipment, and supplies;
whether the hospital’s global budget for the year will be adequate to cover the minimum costs the hospital will have to incur to deliver services, and whether and how the budget can be modified to respond to changes in community needs, the amounts the hospital has to pay for personnel, equipment, drugs, etc.; and
how the hospital will be paid for the services it delivers, and how the budget affects those payments.
Since hospitals differ significantly on the first two factors, a global budget program could benefit some hospitals while harming others. Because the third and fourth factors change from year to year, a hospital could benefit from the global budget in some years, but be harmed in other years. And because there is no one standard approach for determining the amounts of global budgets and for ensuring hospitals receive the amount specified in the budget, a hospital that benefits under one approach to global budgets could be harmed under another.
Impacts of a Global Budget Under Different Scenarios
The only way to fully understand whether and when a small rural hospital would do better or worse under a global budget than fee-for-service or cost-based payment is to compare what its profits or losses would be under different scenarios about the volume of services and the cost of delivering those services.
The Impact of a Global Budget on Emergency Department Services
The table below shows a hypothetical Emergency Department at a Critical Access Hospital under four different scenarios. In the Status Quo scenario, the ED has 12,500 visits, and the staffing and other costs for the ED are the same as those used in . It will be assumed that payers other than Medicare (i.e., Medicaid, Medicare Advantage, commercial insurance plans, and self-insured patients) pay an average of $185 per ED visit ($120 for the hospital and $65 for the physician), which is enough to generate a small (3%) profit for the ED. (It is assumed that current payments are high enough to cover the costs of the ED in order for the relative impacts of the global budget in different scenarios to be seen more easily.)
Three scenarios are used to show the impact on the hospital when the number of visits changes:
In Scenario A, the number of visits decreases by 10%, so fee-based revenues decrease. The cost-based payment from Medicare increases slightly because, with fewer visits, the physicians spend a smaller proportion of their time seeing patients, which means that a larger share of the physicians’ compensation will be treated as a hospital cost (which is eligible for cost-based payment) rather than a professional service (which is supposed to be paid for using Medicare physician fees). However, this increase in the cost-based payment does not offset the reduction in fee-based revenues, and the hospital now has a loss in the service line.
In Scenario B, the number of visits increases by 10%, the cost-based payment decreases slightly, fee-based revenues increase, and the net result is an 8% profit for the hospital.
In Scenario C, the number of visits increases significantly, and it is assumed that the volume of visits during certain times is sufficiently high that the hospital needs to hire 2 additional FTE physicians in order to have two physicians on the high-volume shifts instead of one. Since the cost of operating the ED increases (the amount shown is less than the cost shown in for an ED with 15,000 visits because only direct costs are assumed to change with the higher number of visits, not indirect costs), the cost-based payment from Medicare increases to covers Medicare’s share of this. Since the number of visits increases, the hospital receives more fee-based revenue. The net result is that the hospital ED remains profitable. (The profitability will vary depending on exactly how much the total number of visits increases.)
Figure 14
ED Margins Under Cost-Based Payment
When the Number of Visits Changes
STATUS QUO |
SCENARIO A Fewer Visits |
SCENARIO B More Visits |
SCENARIO C More Vists + Cost |
||||
|---|---|---|---|---|---|---|---|
| Amount | Amount | Change | Amount | Change | Amount | Change | |
| ED Visits | |||||||
| ED Visits | 12,500 | 11,250 | −10% | 13,750 | 10% | 15,000 | 20% |
| Revenue | |||||||
| Medicare Facility Cost | $1,154,000 | $1,198,000 | 4% | $1,111,000 | −4% | $1,369,000 | 19% |
| Medicare Physician Fee | $1,113,000 | $1,002,000 | −10% | $1,224,000 | 10% | $1,336,000 | 20% |
| Subtotal Medicare Payments | $2,268,000 | $2,200,000 | −3% | $2,335,000 | 3% | $2,705,000 | 19% |
| Other Payers Facility Fee | $675,000 | $608,000 | −10% | $742,000 | 10% | $810,000 | 20% |
| Other Payers Physician Fee | $366,000 | $329,000 | −10% | $402,000 | 10% | $439,000 | 20% |
| Subtotal Other Payers Payments | $1,041,000 | $937,000 | −10% | $1,145,000 | 10% | $1,249,000 | 20% |
| Uninsured Facility Fee | $0 | $0 | $0 | $0 | |||
| Uninsured Physician Fee | $0 | $0 | $0 | $0 | |||
| Subtotal Uninsured Payments | $0 | $0 | $0 | $0 | |||
| Total Revenue | $3,308,000 | $3,136,000 | −5% | $3,480,000 | 5% | $3,954,000 | 20% |
| Cost | |||||||
| Facility Cost | $2,313,000 | $2,403,000 | 4% | $2,223,000 | −4% | $2,742,000 | 19% |
| Cost of Clinician Patient Time | $900,000 | $810,000 | −10% | $990,000 | 10% | $1,080,000 | 20% |
| Total Cost | $3,213,000 | $3,213,000 | 0% | $3,213,000 | 0% | $3,822,000 | 19% |
| Margin | |||||||
| Margin | $96,000 | ($76,000) | −179% | $268,000 | 179% | $131,000 | 36% |
| Pct Margin | 3.0% | −2.4% | 8.3% | 3.4% | |||
The next table shows the same ED if the hospital receives a global budget for hospital services from Medicare and also from one-half of the non-Medicare payers. It is assumed here that the global budget amount allocated to the ED for each payer is the same as what the hospital would have received from that payer under the cost-based and fee-based payments shown above. (If the global budget were reduced by a “discount,” as proposed in the CMS CHART Model, the revenues and margins would be lower than what are shown in the table.) Although the global budget is “global” and the hospital does not need to allocate the same proportion of revenue to the ED as it did before, allocating more (or less) of the global budget to the ED would simply increase (or reduce) losses elsewhere.
It is assumed that participation by payers in the global budget program is voluntary, and that half of the non-Medicare payers continue to pay fees for each visit. Moreover, since hospital global budgets only constrain or replace revenues for hospital services, not physician services, the hospital continues to receive fees from all payers for the time the physicians spend with patients.57
Figure 15
ED Margins Under a Global Budget
When the Number of Visits Changes
STATUS QUO |
SCENARIO A Fewer Visits |
SCENARIO B More Visits |
SCENARIO C More Visits + Cost |
||||
|---|---|---|---|---|---|---|---|
| Amount | Amount | Change | Amount | Change | Amount | Change | |
| ED Visits | |||||||
| ED Visits | 12,500 | 11,250 | −10% | 13,750 | 10% | 15,000 | 20% |
| Revenue | |||||||
| Medicare Facility Global Pmt | $1,154,000 | $1,154,000 | $1,154,000 | ||||
| Medicare Facility Cost | $1,154,000 | $0 | −100% | $0 | −100% | $0 | −100% |
| Medicare Physician Fee | $1,113,000 | $1,002,000 | −10% | $1,224,000 | 10% | $1,336,000 | 20% |
| Subtotal Medicare Payments | $2,268,000 | $2,156,000 | −5% | $2,379,000 | 5% | $2,490,000 | 10% |
| Other Global Facility Payment | $338,000 | $338,000 | $338,000 | ||||
| Other Global Facility Fee | $338,000 | $0 | −100% | $0 | −100% | $0 | −100% |
| Other Global Physician Fee | $183,000 | $165,000 | −10% | $201,000 | 10% | $219,000 | 20% |
| Subtotal Other Global Payments | $520,000 | $502,000 | −3% | $539,000 | 4% | $557,000 | 7% |
| Other Payers Facility Fee | $338,000 | $304,000 | −10% | $371,000 | 10% | $405,000 | 20% |
| Other Payers Physician Fee | $183,000 | $165,000 | −10% | $201,000 | 10% | $219,000 | 20% |
| Subtotal Other Payers Payments | $520,000 | $468,000 | −10% | $572,000 | 10% | $624,000 | 20% |
| Uninsured Facility Fee | $0 | $0 | $0 | $0 | |||
| Uninsured Physician Fee | $0 | $0 | $0 | $0 | |||
| Subtotal Uninsured Payments | $0 | $0 | $0 | $0 | |||
| Total Revenue | $3,308,000 | $3,127,000 | −5% | $3,490,000 | 6% | $3,672,000 | 11% |
| Cost | |||||||
| Facility Cost | $2,313,000 | $2,403,000 | 4% | $2,223,000 | −4% | $2,742,000 | 19% |
| Cost of Clinician Patient Time | $900,000 | $810,000 | −10% | $990,000 | 10% | $1,080,000 | 20% |
| Total Cost | $3,213,000 | $3,213,000 | 0% | $3,213,000 | 0% | $3,822,000 | 19% |
| Margin | |||||||
| Margin | $96,000 | ($86,000) | −190% | $277,000 | 189% | ($151,000) | −257% |
| Pct Margin | 3.0% | −2.7% | 8.6% | −3.9% | |||
Under this payment arrangement:
In the status quo scenario, the hospital makes a small profit on the ED that is identical to what it received under current payment systems because the costs and revenues are the same.
In Scenario A, fewer visits are made to the hospital ED. The revenue for hospital services from Medicare does not change because it is coming from the global budget. In contrast, the hospital would have received more revenue under cost-based payment (because a larger share of the physician compensation would be eligible for cost-based payment). The revenue for hospital services from the subset of other payers that are participating in the global budget also stays the same, whereas that revenue would have decreased under fee-based payment. The global budget does nothing to stop the loss of fee-based revenues from the payers that are not participating in the global budget program, and it does nothing to stop the loss of fee-based revenues from Medicare and other payers for physician services since those services are not part of the global budget. The net effect is that the hospital experiences a larger reduction in revenue under the global budget than under the current payment system. Since the total cost of the ED is the same, this creates a financial loss for the hospital.
In Scenario B, where visits increase, the opposite effect occurs. The hospital receives more revenue from Medicare for the hospital component of services than it would have received under cost-based payment, but less revenue from other global payers than under fee-for-service payment.
In Scenario C, the hospital incurs higher costs because it is employing additional physicians, but whereas the Medicare payment for hospital services would have increased under cost-based payment to cover a portion of the higher cost, the Medicare payment stays unchanged under the global budget. The hospital has significantly more visits, but since half of the non-Medicare payers are paying based on a fixed global budget, revenues increase less than they would under the current payment system. The net result is that the hospital experiences a financial loss.
Although it is possible that the hospital would receive a higher global budget if the increase in ED visits was due to growth in the local population, it is also possible that the hospital would receive a lower global budget if the population decreased but the number of ED visits increased due to more health problems among the remaining residents or reduced access to primary care services in the community.
A comparison of margins under the two payment systems shows when visits change by small amounts, there is no benefit to being in the global budget model compared to the current payment system. The impacts would only be slightly different if the hospital were receiving all of its revenue for hospital services through a global budget, since less than 20% of the hospital component of revenues is coming from fees.
Figure 16
ED Margins Under Cost-Based Payment vs. Global Budget
STATUS QUO |
SCENARIO A Fewer Visits |
SCENARIO B More Visits |
SCENARIO C More Visits + Cost |
|
|---|---|---|---|---|
| ED Visits | ||||
| ED Visits | 12,500 | 11,250 | 13,750 | 15,000 |
| Margin | ||||
| Cost-Based + FFS | 3.0% | −2.4% | 8.3% | 3.4% |
| Global Budget | 3.0% | −2.7% | 8.6% | −3.9% |
Obviously, the impacts depend on the scenario, and it is certainly possible to construct scenarios in which the hospital would be better off under global payment than under current payment systems. However, it is equally possible to construct scenarios in which there would even more negative impacts than what is shown above.
As noted above, the status quo scenario was constructed assuming that the hospital’s current payments would be high enough to cover the cost of operating the ED, so that if the hospital received the same amount of revenue under a global budget, it would also be able to cover the cost. Most small rural hospitals do not receive payments that are higher than their costs, so their actual margins under all of these scenarios would be much lower than those shown above. However, the relative differences between the scenarios and the differences between a global budget and cost-based payment in each scenario would still be similar to those shown in the table. For example, if the hospital had a loss of 5% under the current payment system, then it would also have a 5% loss under the global budget, it would lose more than 3% under Scenario A, its profit would be less than 9% under Scenario B, and it would lose even more than 4% under Scenario C.
The Impact of a Global Budget on Inpatient Care
The table below shows a hypothetical inpatient unit at a Critical Access Hospital under four different scenarios. For simplicity, it is assumed that the hospital only has acute inpatients (i.e. no swing beds), that half of the patients are Medicare beneficiaries, and all of the others have health insurance. In the Status Quo scenario, the unit has an average daily census of 3.0, and the staffing and other costs are the same as for an inpatient unit with an ADC of 3.
Under current payment systems, the hospital would receive a cost-based payment for the Medicare beneficiaries, and it would be paid fees for each admission or inpatient day by other payers. For purposes of this example, it is assumed that payers other than Medicare pay an average of $2,400 per day for inpatient care, which is enough to generate a small (3.5%) profit for the inpatient unit. (The payment amounts here are assumed to be high enough to cover the hospital’s costs in order to better show the relative impact of using a global budget to pay for services.)
Three scenarios are used to show the impact of changes in acute admissions:
In Scenario A, the average daily acute census decreases to 2.5, with the reduction equally split between patients on Medicare and other types of insurance. The Medicare cost-based payment does not change because the cost of the unit does not change and Medicare beneficiaries still represent 50% of patients. However, revenues from the other payers decrease because there are fewer patients, so the hospital now experiences a loss.
In Scenario B, the average daily census doubles, and it is assumed the hospital needs to double the number of nurses on the unit.58 Because the costs have increased, Medicare pays a higher amount, and because there are more non-Medicare patients, fee-for-service revenues increase, and the hospital’s profit on the unit increases significantly. The hospital could even reduce the amount it charges for inpatient care significantly and still make a profit on the unit.
In Scenario C, the average daily census stays the same as in Scenario A, but the cost of operating the unit increases, perhaps because one of the nurses became ill and the hospital had to hire a temporary nurse to fill the position at a higher cost. Although the Medicare payment increases because of the higher cost, that only covers 50% of the increase (since only half of the patients are Medicare beneficiaries), and the hospital now has a smaller profit margin on the unit.
Figure 17
Inpatient Margins Under Cost-Based Payment
When the Number of Admissions Changes
STATUS QUO |
SCENARIO A Fewer Admissions |
SCENARIO B More Admissions |
SCENARIO C Higher Cost |
||||
|---|---|---|---|---|---|---|---|
| Amount | Amount | Change | Amount | Change | Amount | Change | |
| Daily Inpatient Census | |||||||
| Acute Census | 3.0 | 2.5 | −17% | 6.0 | 100% | 3.0 | 0% |
| Total Inpatients | 3.0 | 2.5 | −17% | 6.0 | 100% | 3.0 | 0% |
| Revenue | |||||||
| Medicare Cost-Based Pmt | $1,203,000 | $1,203,000 | 0% | $1,441,000 | 20% | $1,247,000 | 4% |
| Other Payers Per Diem | $1,314,000 | $1,095,000 | −17% | $2,628,000 | 100% | $1,314,000 | 0% |
| Total Revenue | $2,517,000 | $2,298,000 | −9% | $4,069,000 | 62% | $2,561,000 | 2% |
| Cost | |||||||
| Total Cost | $2,432,000 | $2,432,000 | 0% | $2,911,000 | 20% | $2,519,000 | 4% |
| Margin | |||||||
| Margin | $86,000 | ($133,000) | −255% | $1,158,000 | 1,247% | $42,000 | −51% |
| Pct Margin | 3.5% | −5.5% | 39.8% | 1.7% | |||
The next table shows what would happen under the same scenarios if the hospital was receiving a global payment instead of cost-based payment from Medicare and a global payment instead of per diem payments from half of the other payers.
The global payments are assumed to be identical to what the hospital would have received under current payment systems, so the cost, revenue, and margin in the Status Quo scenario is the same.
In Scenario A, the global payments stay the same when the inpatient census decreases, and the hospital’s revenues only decrease for the payers who are not using a global budget. As a result, the hospital loses money, but the loss is smaller than under the current payment system.
In Scenario B, the cost of operating the inpatient unit increases but the Medicare payment stays the same because it is no longer tied to the actual cost of the unit. The number of patients on the unit increases, but revenues only increase for the subset of payers that are not using a global budget. However, because the average cost per day decreases but payment per admission remains the same, the increase in revenues for the remaining fee-for-service patients exceeds the increase in the cost of services. As a result, the hospital makes a higher profit on the unit, but much less than it would have made under the current payment system, and it would not be able to reduce the fees it charges for patient care.
In Scenario C, the cost of caring for the same number of patients increases, but none of the hospitals’ revenues are based on actual cost, so the hospital now loses money.
Figure 18
Inpatient Margins Under a Global Budget
When the Number of Admissions Changes
STATUS QUO |
SCENARIO A Fewer Admissions |
SCENARIO B More Admissions |
SCENARIO C Higher Cost |
||||
|---|---|---|---|---|---|---|---|
| Amount | Amount | Change | Amount | Change | Amount | Change | |
| Daily Inpatient Census | |||||||
| Acute Census | 3.0 | 2.5 | −17% | 6.0 | 100% | 3.0 | 0% |
| Total Inpatients | 3.0 | 2.5 | −17% | 6.0 | 100% | 3.0 | 0% |
| Revenue | |||||||
| Medicare Inpatient Global Pmt | $1,203,000 | $1,203,000 | $1,203,000 | ||||
| Medicare Cost-Based Pmt | $1,203,000 | $0 | −100% | $0 | −100% | $0 | −100% |
| Other Payers Global Pmt | $657,000 | $657,000 | $657,000 | ||||
| Other Payers (Global) Per Diem | $657,000 | $0 | −100% | $0 | −100% | $0 | −100% |
| Other Payers Per Diem | $657,000 | $548,000 | −17% | $1,314,000 | 100% | $657,000 | 0% |
| Total Revenue | $2,517,000 | $2,408,000 | −4% | $3,174,000 | 26% | $2,517,000 | 0% |
| Cost | |||||||
| Total Cost | $2,432,000 | $2,432,000 | 0% | $2,911,000 | 20% | $2,519,000 | 4% |
| Margin | |||||||
| Margin | $86,000 | ($24,000) | −128% | $263,000 | 206% | ($2,000) | −102% |
| Pct Margin | 3.5% | −1.0% | 9.0% | −0.1% | |||
Comparison of the two simulations shows that under two of the three scenarios, the hospital is worse off financially under the global budget model than under the current payment system. Under Scenario A, although the hospital is better off than it would have been under the current payment system, it still experiences a loss from reducing hospital admissions or readmissions. Scenario C shows that the stable, predictable revenue provided by the global budget is not an advantage for a hospital that experiences unexpectedly higher costs.
If the hospital were receiving all of its revenue for hospital services through a global budget, there would be no loss under Scenario A, but the loss would be greater under Scenario B since there would be no increase in revenue at all to offset the higher costs required to care for additional patients.
Here again, the impacts depend on the scenario. Under different scenarios, the hospital would be better off under a global budget in some scenarios and worse off in others. The impacts also depend on the hospital, since changes in patient volume affect costs differently at different hospitals, and different hospitals face differing degrees of variability in their costs from year to year.
Figure 19
Inpatient Margins Under Cost-Based Payment vs. Global Budget
STATUS QUO |
SCENARIO A Fewer Admissions |
SCENARIO B More Admissions |
SCENARIO C Higher Cost |
|
|---|---|---|---|---|
| Daily Inpatient Census | ||||
| Acute Census | 3.0 | 2.5 | 6.0 | 3.0 |
| Total Inpatients | 3.0 | 2.5 | 6.0 | 3.0 |
| Margin | ||||
| Cost-Based + FFS | 3.5% | −5.5% | 39.8% | 1.7% |
| Global Budget | 3.5% | −1.0% | 9.0% | −0.1% |
The Impact of a Global Budget on Ancillary Services
The impact of a global budget on a hospital’s ability to deliver ancillary services such as laboratory tests, radiology studies, drugs, and medical supplies depends heavily on the proportion of fixed, semi-variable, and variable costs in each service line. In the ED and inpatient examples above, almost all of the costs are fixed costs or semi-variable costs, so the cost of the service line does not change with small changes in volume. In those cases, the biggest problem with the global budget arises when the volume of services increases by a large enough amount that the hospital has to increase its staffing, because the hospital’s cost increases but revenue under the global budget stays the same. (Even if there is an increase in the global budget the next year based on inflation, that would only cover higher costs due to inflation-based increases in wages, not the higher cost due to a higher staffing level.)
In many other service lines, however, the hospital’s cost can change by large amounts even with small changes in volume because a higher proportion of the costs are variable costs. For example, if the number of patients admitted to the hospital increases or decreases during the year, the hospital’s spending on medical supplies will generally increase or decrease proportionately, even if the staffing on the inpatient unit remains the same. Since the global budget does not change, the hospital will profit when the number of patients decreases and it will experience losses when the number of patients increases.
The biggest problems arise where (1) the cost of the service depends not only on how many patients receive a service, but on the specific type of service they need, and (2) where the cost to the hospital of the materials used to deliver the service can change significantly during the course of the year. For example, the amount that a hospital spends on drugs depends on how many patients it treats, what types of drugs are used for the treatments, and the price the hospital has to pay to acquire the drugs. Under both cost-based payment and fee-for-service payment, the hospital will receive more revenue when it uses more drugs or more expensive drugs, and under cost-based payment, it will also receive more revenue if the price of drugs increases suddenly during the year. Conversely, the hospital will receive less revenue if it uses fewer drugs or less expensive drugs. However, under a global budget, the hospital receives the same revenue during the year regardless of how much it ends up having to spend on drugs, so it could experience large losses if the prices of drugs increase or if patients need particularly expensive drugs.
The Impact of a Global Budget on Patients’ Access to Quality Care
Because the hospital’s total expenses will increase by some amount when more patients receive services, but its revenue would remain the same under a global budget, the hospital is financially penalized when more patients need services, and it is financially rewarded if it helps fewer patients. Similarly, it is penalized when patients receive tests or treatments that involve more expensive supplies or drugs, and rewarded when it avoids using new and more expensive treatments.
Although this creates a desirable incentive for the hospital to avoid delivering unnecessary services and unnecessarily expensive services, it creates a very undesirable financial incentive to limit or withhold access to necessary services and to avoid using more expensive treatments that achieve better outcomes for patients. While some services are “high value” because they achieve better outcomes at a lower cost, others deliver high value because the better outcomes justify the higher cost. The incentives created by the global budget reward the hospital for delivering more of the first group but penalize it for delivering more of the second.
The Impact of a Global Budget on Affordability of Care for Patients
A global budget does not guarantee that the cost of individual services or the total spending on patients’ care will be lower. The Maryland global budget model has been touted as having “reduced” the cost of hospital care, but this only means that the growth in spending in Maryland was lower than the growth in other states. Spending on hospital services did not actually decrease, and spending per patient (both on hospital services and all healthcare services) remained higher in Maryland than in other states.59 It is much easier to have below-average increases in spending when baseline levels of spending are already above average.
Moreover, Medicare pays far more for individual services in Maryland than it does in other states. The evaluation conducted by CMS found that the payments for outpatient services were 58-66% higher in Maryland than they would have been under standard Medicare payments and 33-44% higher for inpatient admissions.60 Since Medicare beneficiaries are responsible for 20% of the amount Medicare pays for outpatient services, the higher prices for outpatient services means Medicare beneficiaries in Maryland pay more for those services than Medicare beneficiaries in other states.
Private insurance plans and uninsured patients pay less for hospital services in Maryland than in other states, but this is not because either prices or revenues are constrained; it is due to the fact that Medicare, Medicaid, and Medicare Advantage plans are required to pay 94% of the amounts that commercial insurance plans pay (i.e., a difference of 6%). The evaluation of the Maryland model conducted by CMS found that payments for commercial insurance payments for inpatient admissions were 11-15% lower in Maryland than in a comparison group. However, the evaluators reported that these lower payments did not fully offset the 33-44% higher payments from Medicare for inpatient admissions; i.e., overall prices for inpatient care were higher in Maryland. (The study did not examine private insurance payments for outpatient services.)
In addition, the Maryland global budget model assures that a hospital receives no less than the full budget amount by allowing the hospital to increase the fees it charges for individual services. This means that if the hospital delivers fewer services, patients will pay more for any services they receive until their deductible is met and they will pay more for any services where cost-sharing is proportional to the fee or charge for the service. Medicare and health insurance plans will collectively pay no more than they would have otherwise because their total payments are constrained by the global budget, but individual patients could pay significantly more than they would have otherwise because of the higher prices for individual services.
The amounts paid by patients could increase even more under the version of global budgets used in the Pennsylvania Rural Health Model, because the global budgets in Pennsylvania constrain the portion of revenue that comes from the insurance plan but not the amount that comes from the patient, and because there is no constraint on the amount that comes from self-insured patients. As a result, a hospital could still increase its revenue by increasing charges for services, and all of that increase would come from patients.
Ability of Global Budget Revenues to Sustain Rural Hospital Operations
The scenarios discussed above examine the impacts of changes in service volumes and costs that occur during the course of a year under a global budget that has already been established for that year. However, all of the scenarios assumed that (1) the amount of payment the hospital would receive under current payment systems was adequate to cover the cost of the services in the “status quo scenario,” and (2) the hospital would receive the same amount under the global budget as it would have received under current payment systems in the status quo scenario.
The first assumption was used in an effort to clearly show the impacts of the global budget payment method on the hospital’s finances under different scenarios, but the amount of the budget is also critical. The payments most small rural hospitals are receiving from most payers are not adequate to cover their costs, so a global budget based on the amount of revenue they receive under current payment systems would not prevent them from closing.
In the Maryland and Pennsylvania systems and in global budgets used in other countries, the hospital’s global budget for the year is not determined based on what the hospital would have received under fee-for-service or cost-based payment systems for a particular volume and mix of services. The global budget for the year is based primarily on what the global budget was for the prior year. Although formulas are used to make adjustments for inflation, changes in the population of the community, and other factors, there is no assurance that these formulas will result in a budget that is adequate to cover the hospital’s costs of delivering high-quality services to patients. In the CMS CHART Model, the increase in the discount factor every year would make it less likely that payments would be adequate to cover costs.
There is also the potential that the global budget formulas will result in some hospitals receiving more revenues than they would have received under current payment systems, and potentially even more revenues than they need to cover the cost of services. The possibility of this has been one of the attractions of the global budget concept for some hospitals. Hospitals that have experienced declining revenues because there are fewer people living in their community, because the residents are healthier, or because the residents are more reluctant to receive elective services would have more stable revenues under the global budget than under fee-for-service or cost-based payment. Under a global budget, hospitals that have the ability to eliminate services could reduce their costs without experiencing a loss in revenues, thereby reducing or eliminating financial losses.
The extent to which an individual hospital will benefit or suffer over time will vary, depending on the adequacy of the hospital’s revenues when it first began receiving a global budget, the way that its services and costs change over time, and the formula used to adjust the global budgets over time.
The graph below shows the change in the patient service margin that all of the small rural hospitals in the U.S. would have experienced in 2015-2018 if they had begun receiving all of their patient service revenues based on a global budget beginning in 2015. The initial budget in 2015 is based on the formula used in the Pennsylvania Rural Health Model, i.e., the hospital receives the same amount in 2015 as the hospital’s revenue in 2014 or the average of its 2012-2014 revenues, whichever is greater. The budget in each subsequent year is then increased by the rate of growth in the GDP that year (which ranged between 3% and 5% in the 2016-18 period).
Figure 20
Impact of Global Budgets
on Small Rural Hospitals
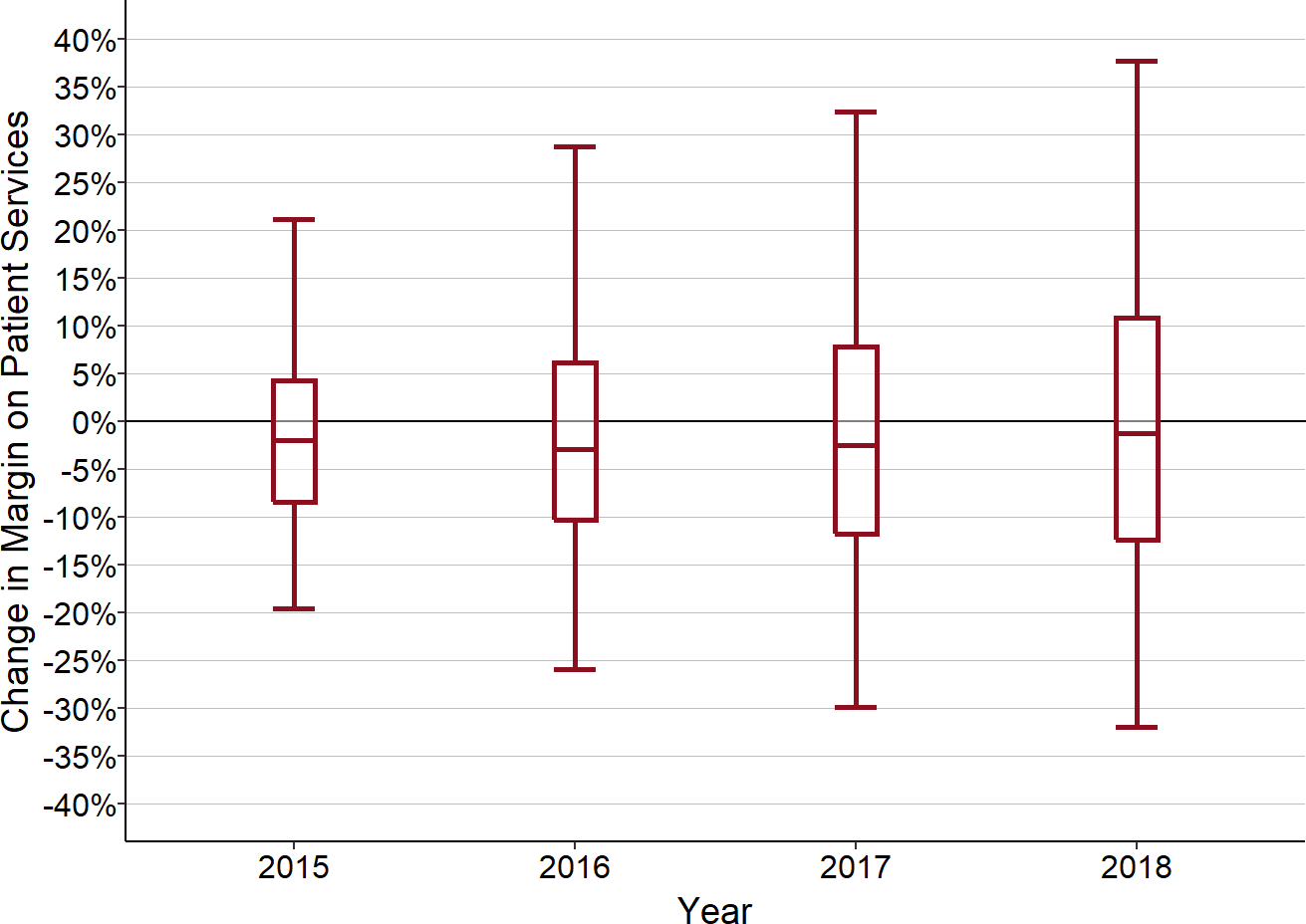
Values are the change from actual patient service margins to estimated margins if a global budget based on 2012-14 revenues had been in effect starting in 2015 for rural hospitals with less than $30 million in total expenses in 2015.
Some hospitals would experience very large increases in their margins each year, while others would experience very large reductions. Overall, the majority of hospitals would have lower margins in each year than they would have had under their existing payment systems. Although some individual hospitals would do worse in some years and better in other years, the negative impacts would outweigh the positive changes, and the cumulative change would be negative for the majority of hospitals. If the budgets were to increase by amounts smaller than the GDP growth, more hospitals would experience even greater losses.
This projection is based on a very simplistic methodology – increasing the prior year’s budget by an inflation factor. As noted earlier, the budgets in Maryland are also adjusted each year using a complex methodology intended to capture changes in the size, demographic characteristics, and healthcare utilization of the community, and to create incentives for reducing avoidable utilization. The Pennsylvania system is supposed to make similar types of adjustments. These adjustments could reduce some of the projected losses shown above, but they could also increase them.
It is important to emphasize that is a retrospective analysis, based on how the hospitals’ costs and revenues actually changed. For many hospitals, it is unlikely that they could have predicted their costs and revenues multiple years into the future with sufficient accuracy to determine, prior to participation in a global budget model, whether they would be better off or worse off financially. Moreover, because small hospitals can experience significant year-to-year variations in revenues, the amount of revenues they receive under these global budget models could vary significantly depending on which base year is used to calculate the initial budget amount.
The Difficulty of Expanding Services Under a Global Budget
Although the stability of revenues under the global budget can be an advantage if a hospital wants to scale back or eliminate a service line, it is a disadvantage if the hospital wants to expand the services it delivers to the residents and businesses in its community. The initial revenue under the global budget is based on the set of services that the hospital was delivering when the global budget program began, and the global budget in each subsequent year is based primarily on the revenue the hospital received the prior year.
As a result, under a global budget, if a rural hospital wants to deliver a new type of service, it would have to seek and receive permission for an increase in its global budget. While this could discourage delivering unnecessary or duplicative services, it could also delay or prevent delivering necessary services. Many small rural hospitals would like to deliver behavioral health services, care management services, and other types of beneficial services to the residents of their communities, but they have been unable to do so because of losses they are experiencing on other services. They may still be unable to deliver these services under a global budget.
In contrast, under a cost-based payment system, a hospital would automatically receive higher payments for the new hospital service based on the cost of delivering that service. Under a fee-for-service system, the hospital would also automatically receive additional revenues from the fees paid for the new services, although the feasibility of delivering the service would depend on the amount that the hospital could charge and the volume of services it would deliver.
Under the Maryland global budget system, if a hospital wants to add a service line, it needs approval from the state Health Services Cost Review Commission to increase its global budget; if the Commission approves the increase, it can also authorize the hospital to charge fees for its services that will generate the higher level of revenue. In contrast, under the Pennsylvania system, each individual payer would need to agree to increase the global budget amount that it pays, and there is no assurance that any increases they did agree to would collectively provide sufficient revenue to cover the cost of delivering the new service. Although the Pennsylvania Rural Health Redesign Center Authority could recommend changes in all of the payers’ global budget amounts that would be sufficient, it cannot require them to make those changes.
A frequently-cited advantage of global budgets is the flexibility they give a hospital to pay for the costs of a new service by reducing avoidable services in existing service lines. However, the hospital’s ability to do this depends on whether it can, in fact, reduce the cost of a service line when the volume of services decreases. At small rural hospitals, the level of staffing in each service line is often already at or near the bare minimum needed to deliver any services at all, and so there is no way to reduce the cost even if fewer services are delivered.
Moreover, the hospital’s ability to reduce readmissions and other avoidable services usually depends on whether the hospital can deliver alternative types of services to the patients. For example, providing care management services to patients with chronic diseases can reduce avoidable hospital admissions and readmissions. However, a hospital would have to deliver the improved care management services first in order to reduce admissions. If the hospital is currently losing money and the global budget provides no additional funds beyond the revenues received in the past, the hospital would not have any additional resources to invest in expanded care management services until after hospital admissions had been reduced.
For example, as shown below:
Even if a small hospital had a 20% readmission rate, cutting the readmission rate in half would only reduce the total number of patients by 8%, and that would not be enough to justify staffing changes in a small hospital. If the hospital had started with an average daily census of 6 patients, a 50% reduction in readmissions would only have reduced the census to 5.5 patients, and the same number of nurses and other staff would be needed on the inpatient unit. Even if the hospital were able to eliminate readmissions entirely, it would likely still need the same level of staffing.
However, if the hospital had hired a nurse care manager to improve discharge planning and follow-up after discharge in order to reduce readmissions, that would increase the hospital’s costs, with no increase in revenue to pay for it.
Moreover, to the extent that the hospital was receiving fee-for-service payments for any of the readmitted patients from payers not participating in the global budget system, reducing readmissions for these patients would reduce the hospital’s revenues.
The net result is that improving care for patients makes the hospital worse off financially, even under a global budget.61
Figure 21
Impact on Inpatient Margins of Reducing Readmissions
Under a Global Budget
Baseline
|
Reduced Readmissions
|
No Readmissions
|
|||
|---|---|---|---|---|---|
| Amount | Amount | Change | Amount | Change | |
| Quality | |||||
| Readmission Rate | 20% | 10% | 0% | ||
| Inpatients | |||||
| Initial Admissions | 5.0 | 5.0 | 0% | 5.0 | 0% |
| Readmissions | 1.0 | 0.5 | −50% | 0.0 | −100% |
| Total Inpatients | 6.0 | 5.5 | −8% | 5.0 | −17% |
| Revenue | |||||
| Medicare Inpatient Global Pmt | $1,678,000 | $1,678,000 | 0% | $1,678,000 | 0% |
| Other Payers Global Pmt | $903,000 | $903,000 | 0% | $903,000 | 0% |
| Other Payers Per Diem | $903,000 | $828,000 | −8% | $753,000 | −17% |
| Total Revenue | $3,484,000 | $3,409,000 | −2% | $3,334,000 | −4% |
| Cost | |||||
| Baseline Cost | $3,390,000 | $3,390,000 | 0% | $3,390,000 | 0% |
| Care Management | $0 | $87,000 | $87,000 | ||
| Total Cost | $3,390,000 | $3,477,000 | 3% | $3,477,000 | 3% |
| Margin | |||||
| Margin | $94,000 | ($68,000) | −172% | ($143,000) | −252% |
| Pct Margin | 2.8% | −2.0% | −4.1% | ||
Winners and Losers Under a Global Budget
What is clear from the above analysis is that a global budget system will be better than the current payment system for some hospitals but worse for others. Although the exact impacts will depend on both the specific characteristics of the hospital and the structure of the global payment system, a few general observations can be made about which hospitals will be “winners” and which will be “losers” under a global budget system.
Winners:
Hospitals that are currently profitable and have no difficulties attracting and retaining staff at competitive wages. Under a global budget, these hospitals could receive a predictable revenue stream that increases with inflation and it could maintain its margin by holding wage increases for its personnel to similar or lower amounts.
Hospitals in communities that are experiencing significant population losses. Under a global budget, these hospitals would no longer experience reductions in revenue due to the declining number of residents in the community.
Short-Term Winners:
- Hospitals with formerly profitable service lines that are no longer financially viable and that are not viewed as essential for the community. Under a global budget, these hospitals could eliminate the service line and its associated cost while retaining the revenues it had been receiving for the services for at least some period of time. However, Medicare and other payers will likely want to reduce payments to a hospital if it is delivering fewer services, so this benefit may only last for a short time.
Losers:
Communities with hospitals where current revenues are lower than the cost of delivering patient services. Under a global budget, revenues would be similar to previous years, so these hospitals would likely continue to receive inadequate revenues.
Communities whose populations have increasing health needs that will result in the need for more services. Under a global budget, the hospitals in these communities would have no additional revenues to support hiring additional staff to provide additional services unless the global budget formula identifies the changes in the community’s health needs and adjusts for them adequately.
Communities that have difficulties recruiting physicians, nurse practitioners, physician assistants, nurses, and/or other staff. Although the global budget could protect the hospital from loss of revenue during periods when it does not have staff available to deliver services, most hospitals will hire temporary employees until vacancies are filled, and there will be no additional revenue under the global budget to cover the higher cost of the temporary workers. Similarly, if the hospital has to pay more to attract employees, this may increase its expenses more than any annual adjustment in the global budget.
Communities that want to establish new service lines to reduce the need for residents to travel long distances for care. As discussed earlier, under a global budget, the hospital would have to get approval from a regulatory agency and/or multiple payers in order to do this.
Since it is impossible to predict exactly what will happen in a small rural community in the future, it is also impossible to say whether and for how long an individual hospital would be a “winner” or “loser.” A global budget model that would help a hospital next year may harm it the following year. In Maryland, the HSCRC receives many requests from hospitals each year to adjust the global budgets determined by the agency’s formulas because of circumstances that are not captured by those formulas.
Figure 22
How Changes in Volume Affect Margins Under a Global Budget
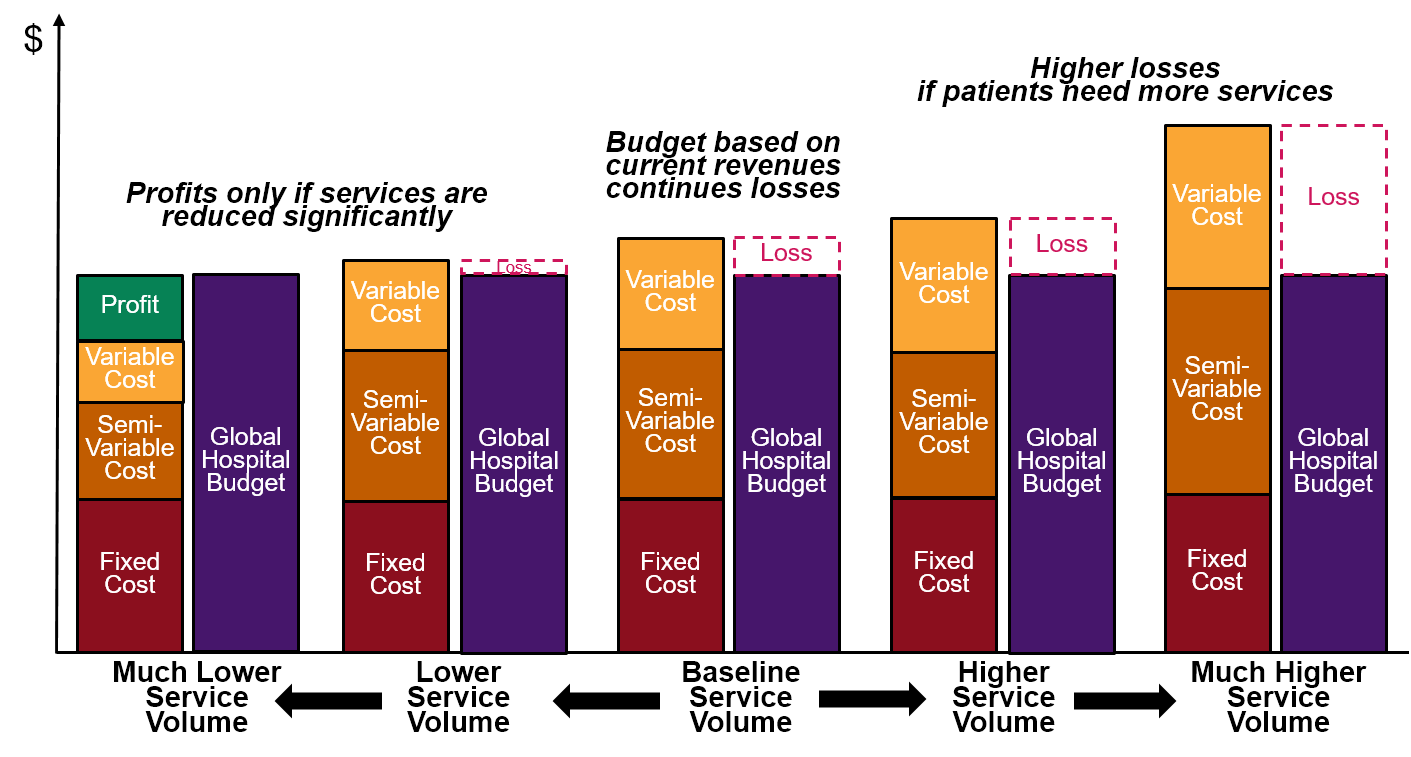
The Shift Away from Hospital Global Budgets in Other Countries
Global hospital budgets have been used for far longer periods of time in other countries than anywhere in the U.S.62 This is partly because hospitals in other countries were traditionally more likely to be government-run than in the United States, and partly because it was easier for countries with single-payer health insurance systems to create and enforce a truly “global” budget for a private hospital since all of the payments for the hospital’s services were coming from a single government agency.
However, other countries’ greater experience with global budgets has also given them a better understanding of their limitations. Although global budgets have generally been viewed as effective in controlling hospital costs, many hospitals have placed limits on admissions or services in order to stay within their budgets, and this has resulted in waiting lists for patients to receive services. Moreover, there is an incentive for hospitals to use the lengths of their waiting lists as justification for receiving higher budgets.63
In order to encourage greater efficiency and reduce wait times for services at hospitals, a number of countries that had used global budget systems have modified or replaced them with “activity-based” systems that tie all or part of the hospital’s revenues to the volume and complexity of services delivered.64 An “activity-based” payment is really just a different name for “fee for service” payment; in fact, many of the systems in the other countries use case rate payments for hospitals similar to the DRG-based payments in the Inpatient Prospective Payment System created by Medicare in 1983.
Evaluations of these changes have found both positive and negative impacts.65 Long waiting times for services continue to be a priority concern for most countries even under the modified versions of global budget systems.66 Many countries have had to provide higher funding levels to increase capacity in order to reduce or avoid increases in waiting times, but a recent study found that waiting times for elective services had begun increasing again in 2019 before the coronavirus pandemic began.67
Clearly, simply using a global budget to pay hospitals does not achieve better results than using a fee-for-service or cost-based payment system if the payments are not adequate to support the cost of delivering high-quality care to patients.
Example: Hospital Payments in Canada
For several decades, the large provinces in Canada funded hospitals using global budgets.68 This was viewed as a major improvement over the previous system in which hospital budgets were reviewed and approved on a line item-by-line item basis.69 The total amount of funding for hospital services and the allocations of that funding among hospitals was determined at the beginning of each year, and the proportions allocated to each hospital typically changed little from year to year.70
However, serious concerns developed about overcrowding of hospitals and long wait times under this system.71 In 2010, the same year that the state of Maryland began implementing its global budget system in the U.S., Canadian provinces began developing ways to reduce the reliance on global budgets and to make greater use of “activity-based funding” for hospitals.72
For example, in 2011, the Ontario Ministry of Health and Long Term Care began a multi-year implementation of a new “patient-based” payment system for hospitals. Under this system, two new funding components partially replaced global budgets: the “Health Based Allocation Method” (HBAM) and “Quality-Based Procedures” (QBP).73 Under the Quality-Based Procedures component, hospitals began receiving a portion of their funding based on the number of patients they treat for select procedures, using standard prices for each procedure that are established by the government. The initial procedures were hip replacement, knee replacement, dialysis, and cataract surgery.
Hospital revenues in Ontario and other provinces are still based primarily on a global budget methodology, and the changes that have been made have not been sufficient to address concerns about inadequate hospital capacity and waiting times. A 2017 survey of 11 countries found that Canada had the highest percentages of patients waiting two months or more for specialist appointments and elective surgery, 4-5 times as many as in the United States.74 A 2019 study of what is described as “hallway healthcare” in Ontario found that on any given day, at least 1,000 people are being treated in Ontario hospital hallways rather than in hospital rooms because of inadequate hospital capacity.75 At the beginning of 2020, the hospitals in Ontario requested an increase of nearly $1 billion in funding in order to address capacity issues.76
Footnotes
If the hospital’s budget is exceeded in one year, it is reduced the following year, and the hospital then has to reduce its fees for services in order to stay within the lower budget. The budget would then presumably return to something closer to the previous level in the next year, and fees would be increased correspondingly.↩︎
In Maryland, Medicare, Medicaid, and Medicare Advantage plans pay 6% less than the regulated fee amounts, and commercial health plans pay the full amount of the fees. The levels of the fees are set high enough to avoid losses due to the 6% discounts.↩︎
Maryland Health Services Cost Review Commission. Global Budget Revenue Agreements and Addendums.↩︎
“Savings” is defined in the program as having occurred when actual spending is less than the amount CMS projects it would have spent if hospital spending in Maryland had increased at the same rate that hospital spending increased in the rest of the country. Spending did not have to decrease in Maryland, nor did spending have to be lower than in the rest of the country, it simply had to increase at a slower rate.↩︎
Maryland Health Services Cost Review Commission. Global Budget Revenue Adjustments.↩︎
The factors that are used in Maryland to make these adjustments are changed over time.↩︎
Rural Policy Research Institute and Stratis Health. Rural Innovation Profile: Global Budget Process as an Alternative Payment Model (2017).↩︎
The Maryland global budget only applies to the “regulated revenue” at a hospital. Hospitals that provide outpatient services at sites away from the hospital campus can obtain additional revenue for some of those services.↩︎
Mortensen K, Perman C, Chen J. “Innovative Payment Mechanisms in Maryland Hospitals: An Empirical Analysis of Readmissions Under Total Patient Revenue,” Healthcare 2(3): 177-183 (September 2014).
Roberts ET et al. “Changes in Hospital Utilization Three Years Into Maryland’s Global Budget Program for Rural Hospitals.” Health Affairs 37(4): 644-653 (April 2018).
Pine JM et al. “Maryland’s Experiment With Capitated Payments for Rural Hospitals: Large Reductions in Hospital-Based Care.” Health Affairs 38(4): 594-603 (April 2019).
Done N, Herring B, Xu T. “The Effects of Global Budget Payments on Hospital Utilization in Rural Maryland.” Health Services Research 54(3): 526-536 (May 2019).↩︎Some of the hospitals’ services may be provided to residents of rural communities, but the hospitals themselves are not located in a community designated as rural.↩︎
Mortensen K, Perman C, Chen J. op cit.; Roberts ET et al. op. cit.; and Done N, Herring B, Xu T op. cit.↩︎
Pine JM et al. op. cit.↩︎
Roberts ET et al. op. cit.; Pine JM et al op. cit.; and Done N, Herring B, Xu T op. cit.↩︎
RTI International. Evaluation of the Maryland All-Payer Model (November 2019).↩︎
Centers for Medicare and Medicaid Services. Hospital Compare datasets.↩︎
RTI International. Evaluation of the Maryland All-Payer Model (November 2019).↩︎
Center for Medicare and Medicaid Innovation. Pennsylvania Rural Health Model.↩︎
There were no restrictions on where Medicare beneficiaries could receive services. A private insurance plan would have to change its benefit design in order to require its members to use the global budget hospital or to create financial disincentives for seeking care elsewhere.↩︎
In Maryland, where all hospitals are regulated, the state makes a determination as to whether an increase in services at one hospital represents the delivery of unnecessary services or a shift in market share from other hospitals, and the state makes different adjustments in the hospitals’ budgets in each case. In the Pennsylvania model, there was no method of changing how much non-participating hospitals were paid for services, so the only way to meet the overall spending target was to reduce the budget at the rural hospital.↩︎
Centers for Medicare and Medicaid Services. Community Health Access and Rural Transformation (CHART) Model Fact Sheet. August 11, 2020.↩︎
The second track in the CHART Model is the “ACO Transformation Track” which will provide additional payments to 20 ACOs in rural areas that participate in the Medicare Shared Savings Program.↩︎
U.S. Department of Health and Human Services, Centers for Medicare and Medicaid Services. Community Health Access and Transformation Model Community Transformation Track Notice of Funding Opportunity. September 15, 2020.↩︎
Center for Medicare and Medicaid Innovation. Chart Model.↩︎
It appeared that CMS did not expect or want rural hospitals to serve as Lead Organizations. A Lead Organization would need to have “received and successfully managed …health-related grant(s) or cooperative agreement(s) totaling at least $500,000 over the last three years” and have experience “engaging and maintaining provider participation in APMs or CMMI demonstration projects/models.” The Notice of Funding Opportunity listed Independent Practice Associations and Academic Medical Centers as examples of entities eligible to serve as Lead Organizations, but not rural hospitals. Notice of Funding Opportunity, op. cit., p. 18.↩︎
The counties and census tracts in a Community did not need to be contiguous; moreover, there was no prohibition on the counties being in completely different parts of the country. Notice of Funding Opportunity, op. cit., p. 19.↩︎
Original Medicare beneficiaries typically represent about 16% of the total population in small rural counties, so in order to have 10,000 Medicare beneficiaries, the community would likely need to have 60,000 or more total residents.↩︎
The Notice of Funding Opportunity (NOFO) stated that a Participant Hospital must agree to “assume accountability for hospital expenditures (as specified in Appendix XI: CPA Financial Methodology) for the Medicare beneficiaries they serve that reside in the Community” (p. 24, emphasis added). Appendix XI stated that the hospital’s Capitated Payment Amount would be determined “based on the portion of services that it provides to the Community” (p. 111) and it defined the population adjustment factor based on beneficiaries who “reside in the Community.” On the other hand, there was nothing in the definition of “Eligible Hospital Services” in the main body of the Notice of Funding Opportunity that indicated that the community where the recipient resides was an eligibility criterion (p. 28). Moreover, the NOFO also stated “For Participant Hospitals that are not located inside the Community, CMMI may modify this CPA financial methodology to account for the Medicare FFS expenditures of beneficiaries located inside the Community only, rather than the total Medicare FFS revenue of the Participant Hospital” (p. 28). The latter statement seemed to imply that hospitals would receive the CPA instead of standard Medicare payments for services delivered to any Medicare beneficiary, not just those who live in the Community. However, since the population adjustments would be based only on the residents of the Community, it would have been problematic to use those to adjust the payments the hospital received for services delivered to beneficiaries who live outside the community, particularly since a hospital located in the Community was only required to have 20% of its services delivered to Community residents.↩︎
Notice of Funding Opportunity, op. cit., pp 27 and 110.↩︎
The methodology states that the average would be calculated “after each historical year has been adjusted according to the prospective adjustments defined…below, to ensure that the years are comparable.” Presumably this meant that the first of the two years would be adjusted for unit price changes and quality so it was more comparable to the second year before the average was taken, since all of the adjustments defined in the methodology would then be applied to the average in order to reflect the differences in payments and quality measures between the baseline period and the year in which the payment would be made. There were no adjustments defined in the original methodology for dealing with unique circumstances such as the impact of the coronavirus pandemic or a natural disaster; the decision to use 2018 and 2019 as the base years was announced later.↩︎
Notice of Funding Opportunity, op. cit., p. 113.↩︎
In subsequent years, the hospital would no longer be receiving separate payments for inpatient and outpatient services, but the hospital would still be required to file claims for individual services, so presumably these adjustments would be based on the proportion of services delivered on an inpatient basis.↩︎
Notice of Funding Opportunity, op. cit., p. 111.↩︎
The methodology said that beneficiaries are “aligned” if they “reside in the Community for the majority of the alignment period,” but then stated that a beneficiary “must not move out of the Community before or during the respective baseline or Performance Period.” Notice of Funding Opportunity, op. cit., p. 112. This may have been intended to distinguish people who had a residence in the community but who did not live there full time; however, there was no detail on how it would have been determined when an individual was “residing” in the community and when someone “moves out.”↩︎
If the Capitated Payments had begun in January 2022, this presumably meant that the Medicare population in the Community in the 12 months from July 2020 to June 2021 would be compared to the Medicare population in the Community from July 2017 to June 2018.↩︎
Notice of Funding Opportunity, op. cit., p. 113.↩︎
The Hierarchical Condition Category (HCC) system was developed to adjust payments to Medicare Advantage Plans based on the projected health needs of their enrolled beneficiaries, and the system is now used to adjust payments under a number of CMS Alternative Payment Models. Although the overall system is designed to adjust for the types of chronic conditions a beneficiary has, the initial component of the HCC score for each beneficiary is a demographic factor based on the individual’s age and gender as well as their living status and reason for Medicare eligibility. For example, a 65-year-old female has an HCC demographic factor of .321, whereas a 95-year-old male has an HCC demographic factor of 1.033. The HCC score for a population is determined by adding all of the individual scores and dividing by the number of individuals.↩︎
Notice of Funding Opportunity, op. cit., p. 113.↩︎
Notice of Funding Opportunity, op. cit., p. 113.↩︎
Notice of Funding Opportunity, op. cit., p. 115.↩︎
The document stated that this adjustment “will impact no more than 2% of the CPA.” Notice of Funding Opportunity, op. cit., p. 112. Existing CMS quality programs and alternative payment models for hospitals only reduce payments based on quality performance, they do not increase them, and there is no indication in the NOFO that good performance on quality measures could have resulted in an increase in the CPA, so it seems likely that CMS intended to reduce the CPA by some amount between 0% and 2%.↩︎
The document stated that additional information on how the quality adjustments are made will be provided after hospitals are selected to participate. Notice of Funding Opportunity, op. cit., p. 112.↩︎
The Lead Organization that applied to participate in the CHART Model would have received a grant of up to $2 million during the “pre-implementation” year, and then up to $500,000 per year during each of the six years in which the hospitals were receiving the Capitated Payment Amounts. The Lead Organization was permitted to request smaller discount factors for hospitals in return for a reduction in the grant amount, and it was also permitted to negotiate different discount factors among the participant hospitals as long as the aggregate discount amount stayed the same. Notice of Funding Opportunity, op. cit., p. 31.↩︎
Notice of Funding Opportunity, op. cit., pp. 113-114.↩︎
Notice of Funding Opportunity, op. cit., p. 30.↩︎
Notice of Funding Opportunity, op. cit., p. 29.↩︎
Notice of Funding Opportunity, op. cit., p. 29.↩︎
The Notice of Funding Opportunity said “Aligned Payers may not need to align with the adjustments that rely on CAH cost report data, since those are not relevant for other payers besides Medicare FFS.” (Notice of Funding Opportunity, op. cit., p. 29)↩︎
Although Critical Access Hospitals receive “cost-based payment” from Medicare, federal sequestration requirements result in payments equal to at most 99% of their costs. As a result, no matter how much a Critical Access Hospital reduces its costs, it will still be paid less than its costs by Medicare, and under the CHART Model, the hospital would have received even less because of the discount and quality adjustment.↩︎
The discount would only have been less than 2% if the total Capitated Revenues in the Community were more than $40 million. Since the majority of rural hospitals receive less than $10 million in Medicare payments for inpatient and outpatient services, four or more hospitals would likely have had to participate in order to meet this threshold.↩︎
Notice of Funding Opportunity, op. cit., p. 31. If a hospital eliminates a service line, the patients would presumably need to obtain those services at another hospital, and the adjustment for a shift in eligible services in the CPA methodology would have reduced the payment to the hospital that eliminated the services in order to avoid Medicare “paying twice” for that service.↩︎
On page 27, the Notice of Funding Opportunity stated “…this APM creates an incentive to reduce potentially avoidable utilization, prevent admissions, and reduce hospital lengths of stay as appropriate. Participant Hospitals will be able to keep the savings that are generated through these reductions.” However, this would only have applied to services that the patient would not receive at all if the hospital did not deliver them; if the hospital stopped delivering specific tests or procedures to patients because the hospital viewed them as unnecessary, but the patients went to other hospitals to receive those services, then the CPA would have been reduced to reflect the fact that the services shifted to another hospital.↩︎
Notice of Funding Opportunity, op. cit., p. 113.↩︎
The average readmission rate nationally is about 18%. Even if a hospital had a 20% readmission rate and reduced the readmission rate to 16% (a 25% reduction), the average daily inpatient census would only decrease by 3%. Most rural hospitals have an average daily inpatient census of less than 10 patients, so the reduction in the readmission rate would mean the inpatient census would decrease by less than 0.3 patients, which is not enough to allow a reduction in staffing.↩︎
Notice of Funding Opportunity, op. cit., p. 31.↩︎
The Maryland global budgets only apply to hospitals, not physician practices. Similarly, the Pennsylvania Rural Health Model only changes payments for hospital services, not for physician services.↩︎
The hospital may also need to increase the number of nursing assistants and incur other higher costs, and it might use a different mix of RNs and LPNs, but for simplicity, the example assumes only a change in registered nurses, who are the most expensive staff on the unit. assumes that the indirect costs allocated to the inpatient unit would not change in the short run if there were an increase in the number of patients on the unit, which is why the cost is different than the amount shown in for the same number of patients.↩︎
RTI International. Evaluation of the Maryland All-Payer Model (November 2019).↩︎
RTI International. Evaluation of the Maryland All-Payer Model (November 2019).↩︎
The loss would be smaller if every payer participated in the global budget program, but there would still be a loss because of the higher cost associated with hiring the nurse care manager with no increase in the global budget to pay for that.↩︎
Wolfe PR, Moran DW. “Global Budgeting in the OECD Countries.” Health Care Financing Review 14(3):55–76 (1993).↩︎
Street A, Duckett S. “Are Waiting Lists Inevitable?” Health Policy 36:1-15 (1996).↩︎
O’Reilly J et al. “Paying for Hospital Care: The Experience With Implementing Activity-Based Funding in Five European Countries.” Health Economics, Policy and Law 7(1): 73-101 (2012).↩︎
Palmer KS et al. “Activity-Based Funding of Hospitals and Its Impact on Mortality, Readmission, Discharge Destination, Severity of Illness, and Volume of Care: A Systematic Review and Meta-Analysis.” PLOS ONE 9(10). (October 2014).↩︎
Waiting Times for Health Services: Next in Line. OECD Health Policy Studies (2020).↩︎
Ibid.↩︎
McKillop I, Pink GH, Johnson LM. The Financial Management of Acute Care in Canada: A Review of Funding, Performance Monitoring and Reporting Practices. Canadian Institute for Health Information (2001).↩︎
Lave JR, Jacobs P, and Markel F. “Transitional Funding: Changing Ontario’s Global Budgeting System.” Health Care Financing Review 13(3): 77-84 (1992).↩︎
Sutherland JM. Hospital Payment Mechanisms: An Overview and Options for Canada. Canadian Health Services Research Foundation. (2011)↩︎
In 2005, the Supreme Court of Canada struck down a law that banned the sale of private insurance for medically necessary services in Quebec in response to a lawsuit filed by a physician in Quebec on behalf of a 73-year old patient who had waited one year for a hip replacement. Health Care in Canada 2009: A Decade in Review. Canadian Institute for Health Information (2009). In 2011, a survey of specialty physicians reported a wait time of 19 weeks between referral from a general practitioner and elective treatment. Barua B, Rovere M, and Skinner BJ. Waiting Your Turn: Wait Times for Health Care in Canada, 2011 Report. Fraser Institute (2011).↩︎
Ibid.↩︎
Ontario’s Action Plan for Health Care. Ontario Government (2012).↩︎
Mossialos E, Djordjevic A, Osborn R, and Sarnak D. International Profiles of Health Care Systems. The Commonwealth Fund (May 2017).↩︎
Hallway Health Care: A System Under Strain. Ontario Government (January 2019).↩︎
Ferguson R. “Ontario Hospitals Ask for Nearly $1 Billion to Ease Hallway Health-Care Problem.” The Star (January 17, 2020).↩︎