The Importance of Rural Hospitals
There are two very different types of hospitals in the U.S: (1) small rural hospitals, and (2) urban and large rural hospitals. There are over 1,000 small rural hospitals, representing nearly one-fourth of all the short-term general hospitals in the country, but they receive less than 3% of total national hospital spending.
Small rural hospitals provide most or all of the healthcare services in the small communities they serve. Small rural hospitals deliver not only traditional hospital services such as emergency care, inpatient care, and laboratory testing, but most of them also deliver rehabilitation, long-term care, and primary care. The majority of the communities they serve are at least a half-hour drive from the nearest alternative hospital, and many communities have no alternate sources of healthcare.
Small rural hospitals are struggling to survive and rural communities are being harmed. The majority of small rural hospitals are losing money delivering patient services. More than 100 rural hospitals have closed in the past decade, and most of these were small rural hospitals. In most cases, the closure of the hospital resulted in the loss of both the emergency department and other outpatient services, and residents of the community must now travel much farther when they have an emergency or need other healthcare services. This increases the risk of death or disability when accidents or serious medical conditions occur, but it also increases the risk of health problems going undiagnosed or inadequately treated due to lack of access to care.
Residents of urban areas can also be harmed by rural hospital closures. Most of the nation’s food supply and energy production comes from rural communities. Farms, ranches, mines, drilling sites, wind farms, and solar energy facilities cannot function without an adequate, healthy workforce, and people are less likely to live or work in rural communities that do not have an emergency department and other healthcare services. Many popular recreation, historical, and tourist sites are located in rural areas, and visitors to those sites need access to emergency services if they have an accident or medical emergency.
The Need to Control Hospital Spending Without Harming Patients
Hospitals are an essential part of the healthcare system. Although far more care is being delivered in patients’ homes, physicians’ offices, and ambulatory surgery centers today than in the past, there are many types of services that cannot be safely delivered in any setting other than a hospital.
Moreover, it is important for every community to have adequate hospital capacity available when it is needed. During the coronavirus pandemic, hospitals unexpectedly needed to provide care for tens of thousands of patients with COVID-19. Some communities were forced to erect temporary hospitals or inpatient units in order to ensure there would be adequate capacity to treat all patients who needed care.
However, hospitals are also very expensive. The United States spends more than $1.5 trillion per year on hospital services. More than one-third (37%) of total healthcare spending goes to hospitals, a far larger share than any other healthcare sector.1
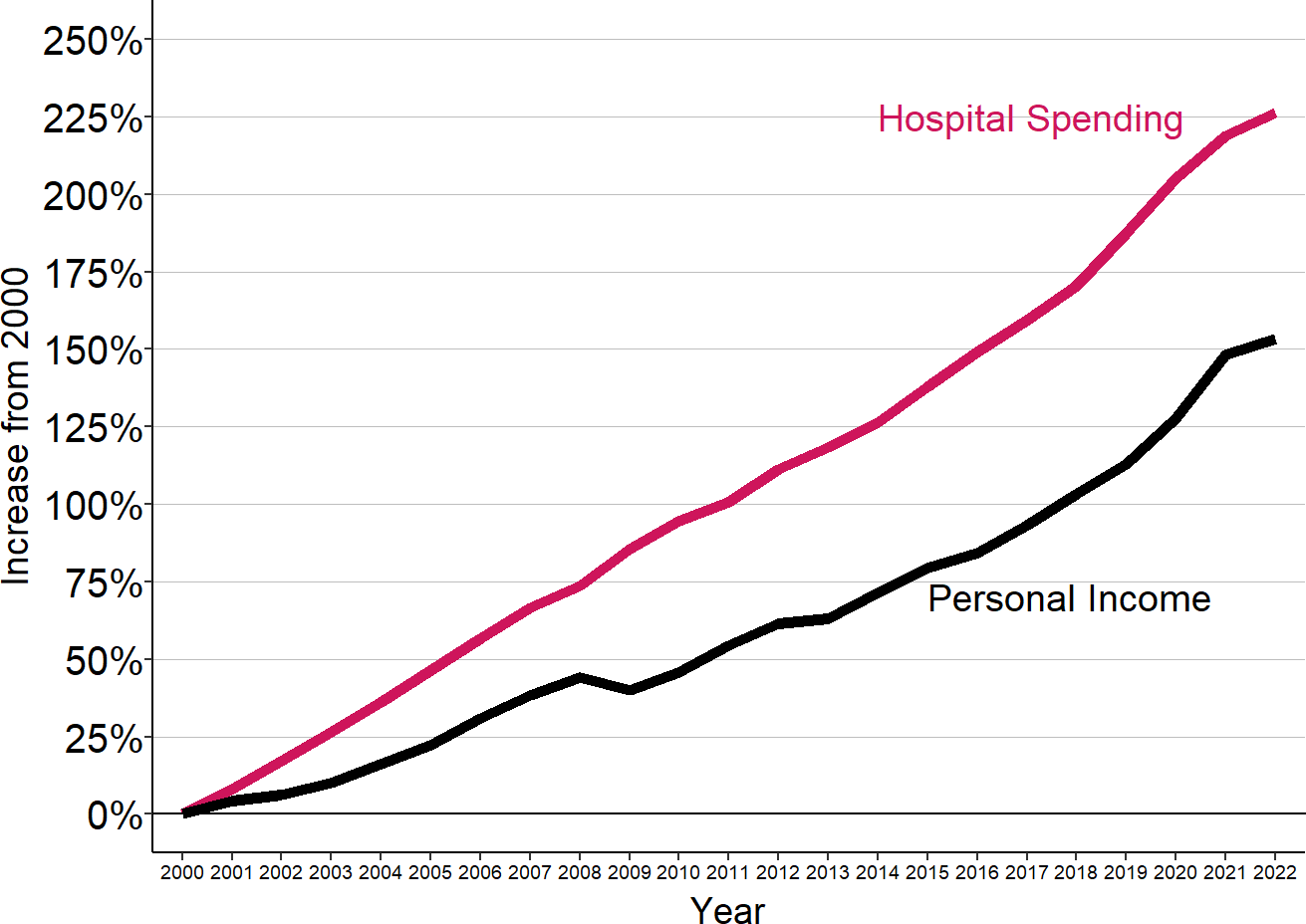
Over the past two decades, national spending on hospital services tripled, more than the increase in total healthcare spending2, and far more than the growth in personal income.3
Figure 1
Cumulative Change in National Hospital Spending and Personal Income
Sources: CMS National Healthcare Expenditure Accounts, BEA Personal Income Data
Because hospitals represent such a large portion of total healthcare spending, it will be almost impossible to make health care or health insurance more affordable unless methods are found to control the growth in spending on hospital care. However, this must also be done in a way that preserves the ability of all citizens to obtain high-quality hospital care in a timely fashion.
As the country searches for policies that will control or reduce hospital spending while maintaining access to quality care, it is essential to recognize that the nation’s hospitals fall into two very different categories: (1) small rural hospitals, and (2) urban and larger rural hospitals. These two groups of hospitals differ dramatically in terms of both the amount they contribute to healthcare spending growth and the size of the financial challenges they face in delivering healthcare to the communities they serve.
Figure 2
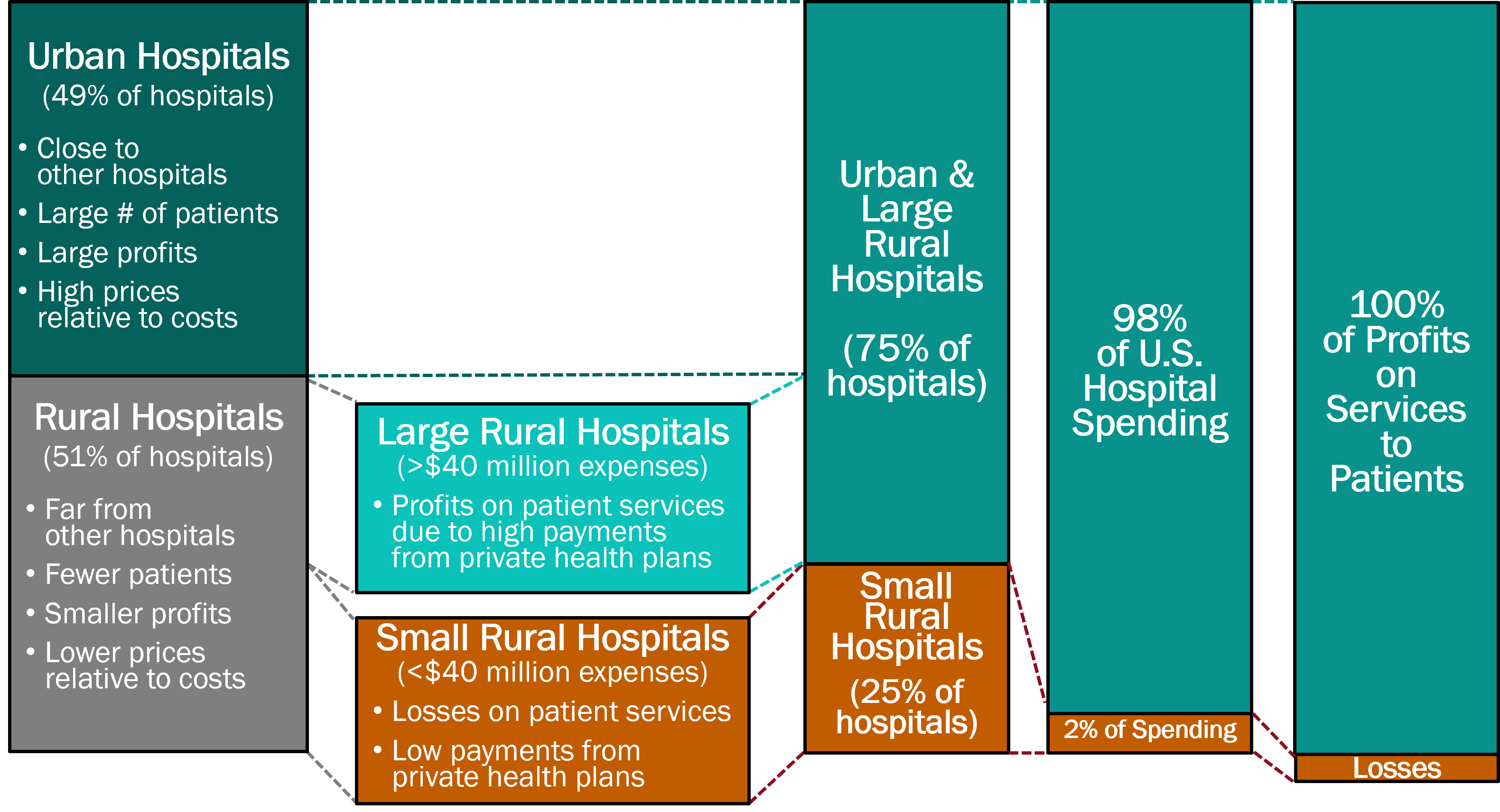
How Rural Hospitals Differ from Urban Hospitals
Over half of the nation’s short-term general hospitals4 are located in rural areas.5 Rural hospitals differ from urban hospitals both in terms of their size and their distance from other hospitals:
- Most rural hospitals are the only source of hospital care in their community. Most cities and urban areas have multiple hospitals that patients can use, but most rural communities have only one hospital that is easily accessible, if they have a hospital at all.
- The majority of urban hospitals are less than 5 miles away from another hospital, and over 80% are within a 15 mile drive from another hospital.
- In contrast, almost two-thirds of rural hospitals are more than 20 miles away from the next closest hospital, and one-fourth are 30 miles or more away.6
Figure 3
Driving Distance to Closest Alternative Hospital
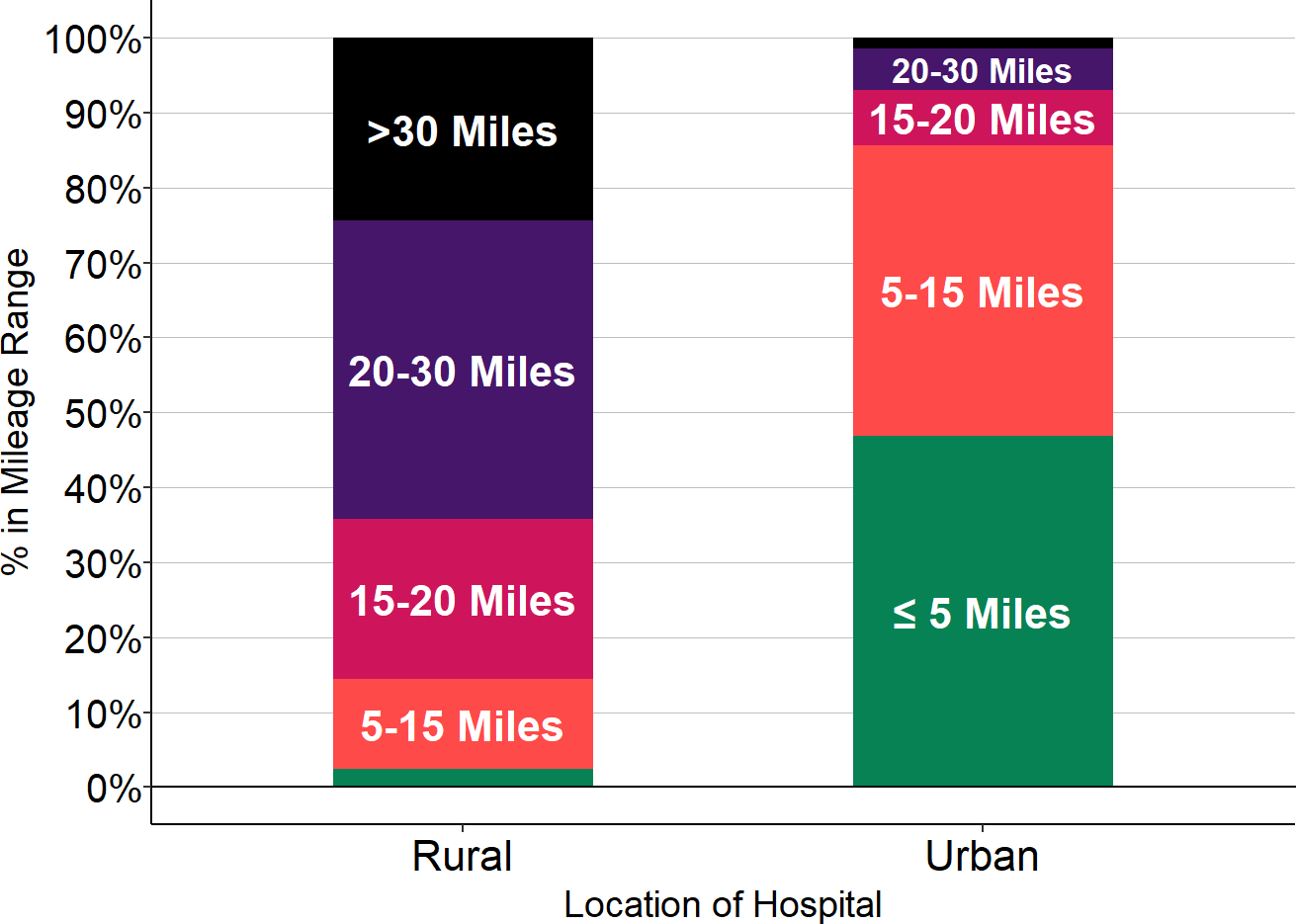
Sources: CMS Provider of Services data, Google Maps
- Most rural hospitals are much smaller than urban hospitals. Although there are some large hospitals located in communities that are classified as rural, most rural hospitals are much smaller than most urban hospitals. The size of a hospital has traditionally been defined in terms of the number of inpatient beds it is licensed to operate, but most of the services that hospitals deliver today are ambulatory care services, not inpatient care. Consequently, a hospital’s total annual expenses is a better measure of a hospital’s relative size than the number of inpatient beds:
- Most urban hospitals have over 200 inpatient beds, whereas most rural hospitals have 25 or fewer beds.7
- More than half of urban hospitals have annual expenses of more than $300 million, but less than 3% of rural hospitals are that large.8
- One-half of rural hospitals have total expenses of less than $45 million, compared to only 2% of urban hospitals.
Figure 4
Total Hospital Expenses
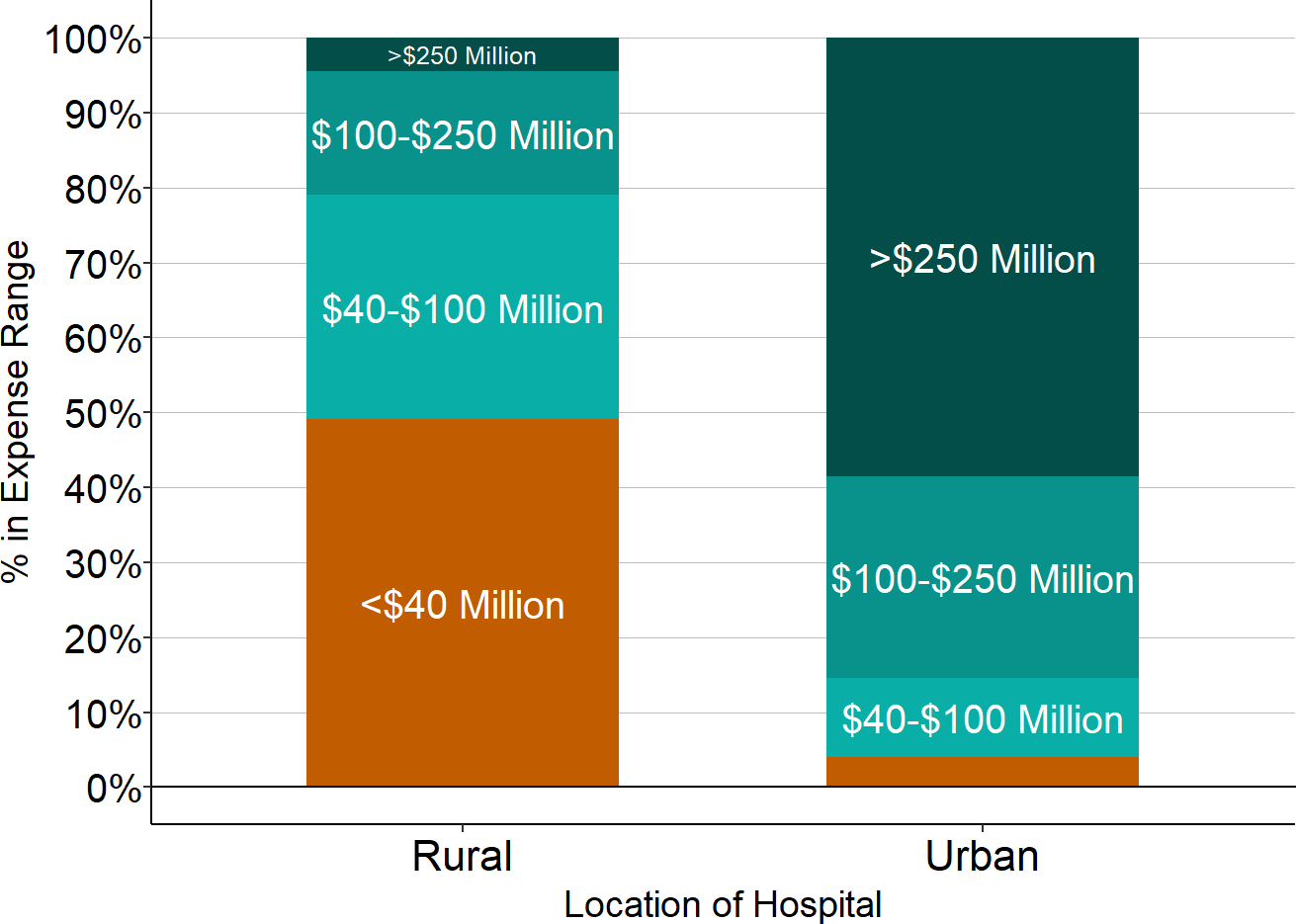
Source: CMS Healthcare Cost Report Information System, 2024 Data
How Small Rural Hospitals Differ From Larger Hospitals
Small rural hospitals – those with annual expenses below the median for rural hospitals ($45 million in 2024) – deliver many of the same kinds of essential services as larger hospitals do. They have emergency services available around the clock, they perform basic laboratory tests and imaging studies, and they provide inpatient care and outpatient care for a wide range of health problems. However, many small rural hospitals also provide services that most urban hospitals and large rural hospitals do not provide:9
- Rehabilitation. In addition to outpatient physical therapy services, 88% of small rural hospitals offer inpatient Skilled Nursing Facility (SNF) services so that community residents can receive rehabilitation in their own communities. In contrast, only 11% of urban hospitals operate a Skilled Nursing Facility.
- Long-Term Care. In addition to skilled nursing care, over 70% of small rural hospitals offer long-term nursing care or assisted living services, whereas less than 3% of urban hospitals provide long-term care services.
- Primary Care. Over 70% of small rural hospitals operate one or more Rural Health Clinics that provide primary care for community residents, and almost half of the others operate some other type of medical clinic for patients. Most small rural hospitals with Rural Health Clinics have more than 12,000 clinic visits per year.
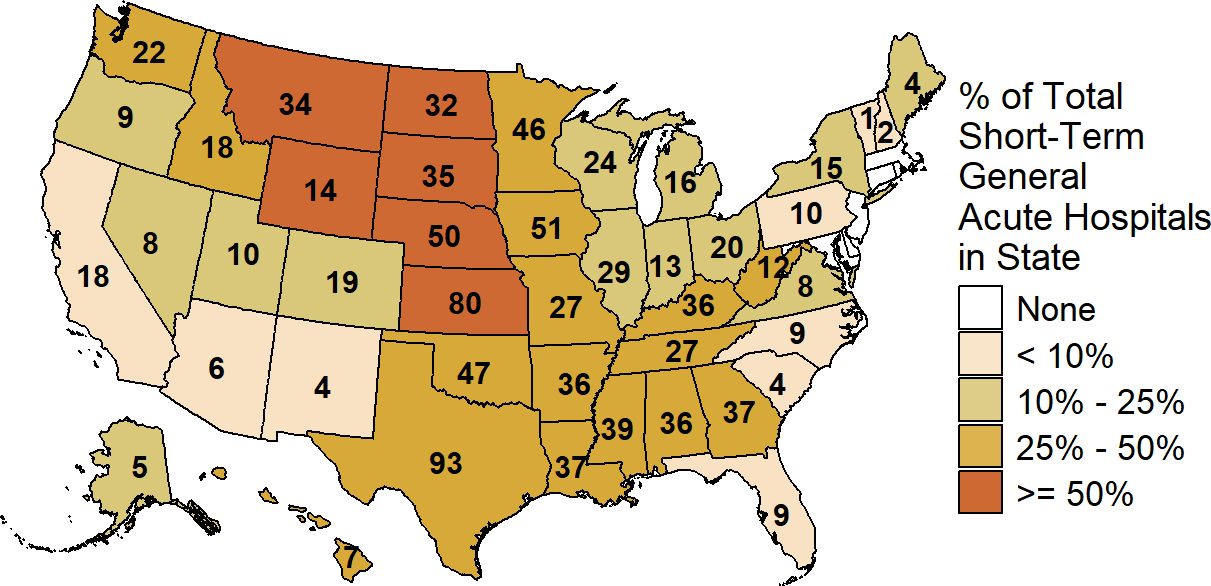
There are over 1,000 small rural hospitals in the country, representing one-fourth of the nation’s total short-term general acute hospitals. Most states (45) have at least one small rural hospital; in 22 states, at least one-fourth of all the hospitals in the state are small rural hospitals, and in 7 of those states, 50% or more of the hospitals are small rural hospitals.
Figure 5
Number of Small Rural Hospitals by State
| State | Total Hospitals |
Rural Hospitals and Rural Emergency Hospitals |
Small Rural Hospitals |
Small Rural Hospitals as Percentage of Total Hospitals |
|---|---|---|---|---|
| Alabama | 83 | 51 | 34 | 41% |
| Alaska | 21 | 16 | 5 | 24% |
| Arizona | 78 | 27 | 6 | 8% |
| Arkansas | 74 | 52 | 41 | 55% |
| California | 305 | 59 | 17 | 6% |
| Colorado | 81 | 43 | 19 | 23% |
| Connecticut | 25 | 4 | 0 | 0% |
| Delaware | 6 | 3 | 0 | 0% |
| District of Columbia | 5 | 0 | 0 | 0% |
| Florida | 180 | 22 | 12 | 7% |
| Georgia | 126 | 74 | 40 | 32% |
| Hawaii | 20 | 13 | 6 | 30% |
| Idaho | 41 | 28 | 18 | 44% |
| Illinois | 170 | 79 | 30 | 18% |
| Indiana | 111 | 55 | 20 | 18% |
| Iowa | 113 | 94 | 49 | 43% |
| Kansas | 120 | 103 | 81 | 68% |
| Kentucky | 90 | 71 | 36 | 40% |
| Louisiana | 99 | 57 | 41 | 41% |
| Maine | 31 | 24 | 5 | 16% |
| Maryland | 41 | 9 | 0 | 0% |
| Massachusetts | 54 | 7 | 1 | 2% |
| Michigan | 121 | 67 | 18 | 15% |
| Minnesota | 122 | 98 | 47 | 39% |
| Mississippi | 91 | 74 | 46 | 51% |
| Missouri | 98 | 59 | 27 | 28% |
| Montana | 61 | 53 | 32 | 52% |
| Nebraska | 84 | 72 | 52 | 62% |
| Nevada | 34 | 14 | 10 | 29% |
| New Hampshire | 26 | 18 | 3 | 12% |
| New Jersey | 60 | 2 | 0 | 0% |
| New Mexico | 40 | 28 | 7 | 18% |
| New York | 146 | 54 | 14 | 10% |
| North Carolina | 98 | 56 | 11 | 11% |
| North Dakota | 44 | 38 | 33 | 75% |
| Ohio | 145 | 74 | 21 | 14% |
| Oklahoma | 110 | 79 | 52 | 47% |
| Oregon | 57 | 34 | 7 | 12% |
| Pennsylvania | 139 | 52 | 12 | 9% |
| Rhode Island | 10 | 1 | 0 | 0% |
| South Carolina | 53 | 22 | 5 | 9% |
| South Dakota | 53 | 49 | 36 | 68% |
| Tennessee | 92 | 54 | 28 | 30% |
| Texas | 349 | 158 | 107 | 31% |
| Utah | 45 | 22 | 11 | 24% |
| Vermont | 14 | 13 | 1 | 7% |
| Virginia | 80 | 31 | 8 | 10% |
| Washington | 85 | 45 | 21 | 25% |
| West Virginia | 46 | 34 | 14 | 30% |
| Wisconsin | 120 | 81 | 28 | 23% |
| Wyoming | 29 | 27 | 13 | 45% |
Sources: CMS Provider of Services data, CMS Healthcare Cost Report Information System
These hospitals are small because the communities they serve have a small number of residents. There are hundreds of small rural hospitals because most of the country consists of small communities. The majority of the 3,200 counties in the U.S. have fewer than 26,000 residents, and these are the counties where the majority of small rural hospitals are located.10 This includes many of the nation’s agricultural areas and ranchlands, which require large amounts of land for crops and animals but have relatively few residents per square mile. One-third of small rural hospitals are located in counties with fewer than 10,000 residents.
In many cases, the small rural hospital is not just the sole provider of hospital services in its community, it is the sole or primary source of all healthcare services in the community. Most small rural communities do not have an urgent care center that residents can use as an alternative to the hospital ED, there is no separate clinical laboratory where residents can obtain diagnostic tests, and there may be few, if any, alternative sources of primary care. One-third of the counties in which small rural hospitals are located are designated by the Health Resources and Services Administration (HRSA) as Primary Care Shortage Areas in the entire county, and for almost all of the rest, a portion of the county is designated as a Primary Care Shortage Area.
The significance of this is even greater when one realizes how remote many rural communities are and how far the residents would have to travel to find alternative sources of care. Almost all small rural hospitals are at least a 20-minute drive from the nearest alternative hospital, and half of them are located 30 minutes or more from another hospital.11 Moreover, the distance between hospitals does not necessarily reflect the distance or time for individuals who live outside of the town where the hospital is located. If an individual lives 15 minutes away from the rural hospital, an alternative hospital that is 30-45 minutes away from the current rural hospital might then be as much as 45-60 minutes away for that individual.12
Example: Forks Community Hospital
Forks is a small town in the Pacific Northwest that is located on the western side of the Olympic National Park. Many people have heard of Forks because it was the setting for the popular Twilight Saga novels written by Stephenie Meyer that were also made into a series of movies. Thousands of tourists visit the area every year for fishing, hiking, or other recreation, and the timber industry also still has a significant presence in the community.
Forks Community Hospital is the only hospital in Forks and the surrounding area. It is a small Critical Access Hospital with 15 licensed beds. Although the estimated population of the City of Forks was only 3,380 in 2022, it is the closest hospital for a group of communities with a total of over 9,000 residents. As a result, its Emergency Department has more than 4,000 visits per year, and its Rural Health Clinics have over 13,000 patient visits each year. Forks Community Hospital also provides nursing care in addition to acute care so that elderly residents of the community can receive long-term care close to their families and friends.
The next-closest hospital to Forks is the Olympic Medical Center in Port Angeles, which is a 70-minute drive. The travel time is even longer for patients who don’t live directly in Forks. For example, for people who live or work in LaPush on the Pacific Coast, Forks Hospital is more than 20 minutes away, and travel to the Olympic Medical Center would require a nearly 90-minute drive.
Despite the key role it plays in the community, Forks Community Hospital loses a significant amount of money on its patient services. Every year between 2012 and 2024, patient service revenues fell short of costs by 8%-25%. The hospital has only been able to continue operating because it is supported by a local property tax levy. This means that, in addition to paying premiums on their health insurance and paying deductibles and copayments for healthcare services, the residents of the community have to tax themselves in order to keep the hospital open and enable the continuation of healthcare services in their community.
Figure 6
Hospitals Closest to Forks
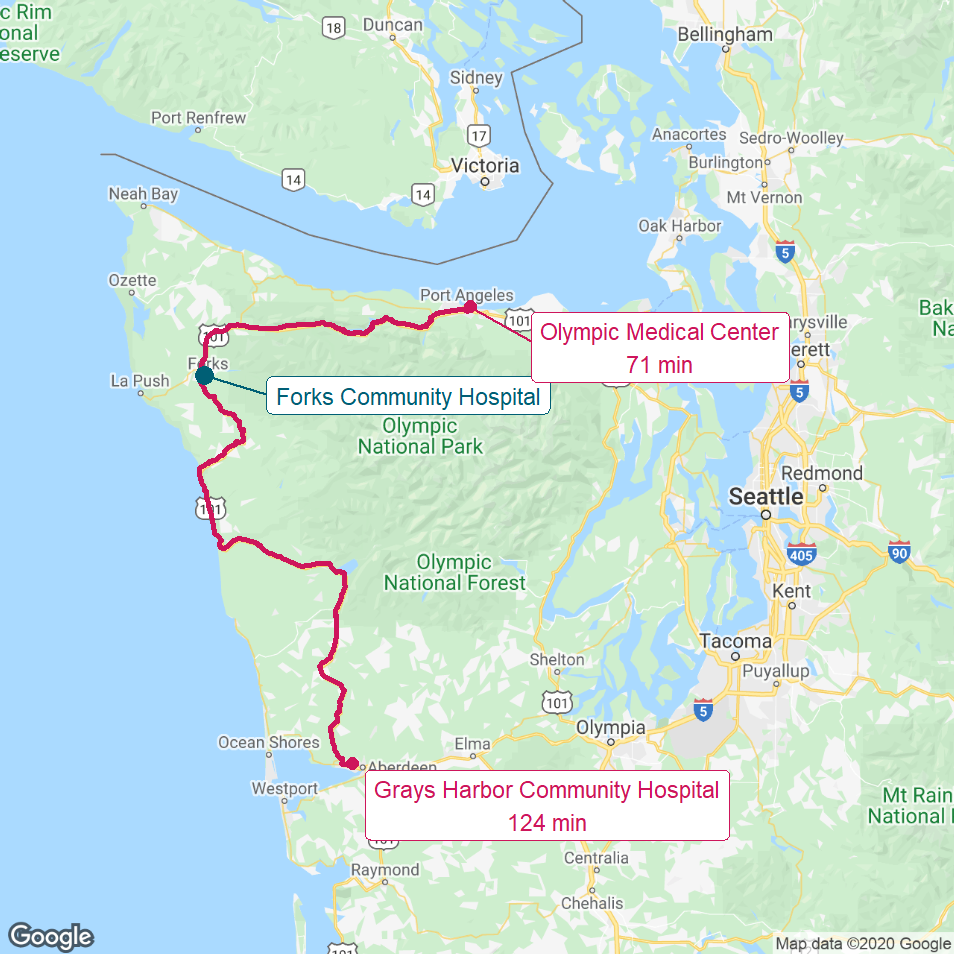
The red lines show the most direct driving routes from Forks Community Hospital to the next-closest hospitals and the estimated driving times.
Figure 7
Communities Closest to Forks
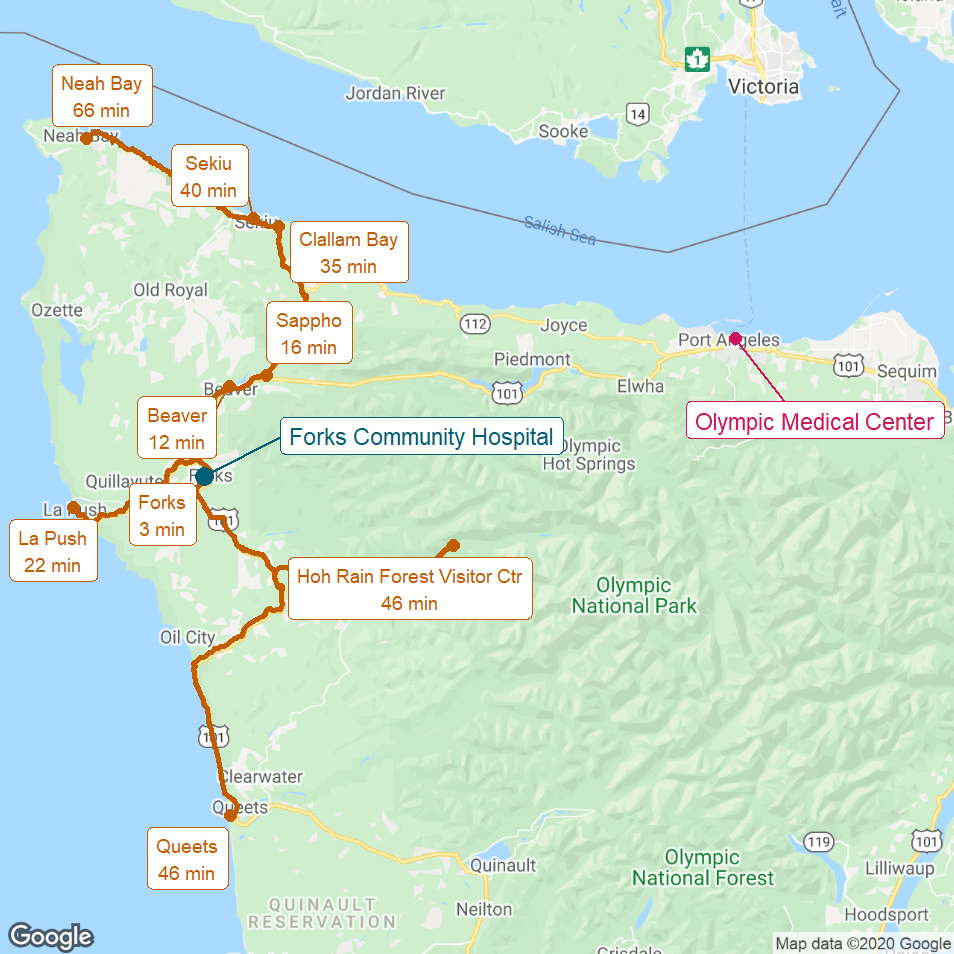
The gold lines show the most direct driving routes to Forks Community Hospital from the closest communities and the estimated driving times.
Small Rural Hospitals Face Greater Financial Challenges Than Other Hospitals
While small rural hospitals deliver many of the same services as other hospitals, they face far greater financial challenges in delivering essential healthcare services than both urban hospitals and larger rural hospitals:
- Most small rural hospitals lose money delivering services to patients, while most urban hospitals and larger rural hospitals make profits on patient services. The primary source of revenues for most hospitals is the payments for services they receive from health insurance plans. Most small rural hospitals are paid less for services by insurance plans than the cost of delivering those services. In contrast, most larger rural hospitals and urban hospitals have been paid more – often significantly more – than it costs them to deliver services to patients.
- Two-thirds of small rural hospitals lose money delivering patient services. In 2024, the median margin on patient services for small rural hospitals was -4.2%, i.e., at the majority of the hospitals, payments were 4% or more below what it cost them to deliver the services.
- In 2024, the median margin on patient services for larger rural hospitals was +7.5% and the median margin on patient services at urban hospitals was +9.4%, i.e., the larger hospitals were paid more than it cost them to deliver their services.
- Two-thirds of small rural hospitals lose money delivering patient services. In 2024, the median margin on patient services for small rural hospitals was -4.2%, i.e., at the majority of the hospitals, payments were 4% or more below what it cost them to deliver the services.
Figure 8
Median Margin on Patient Services
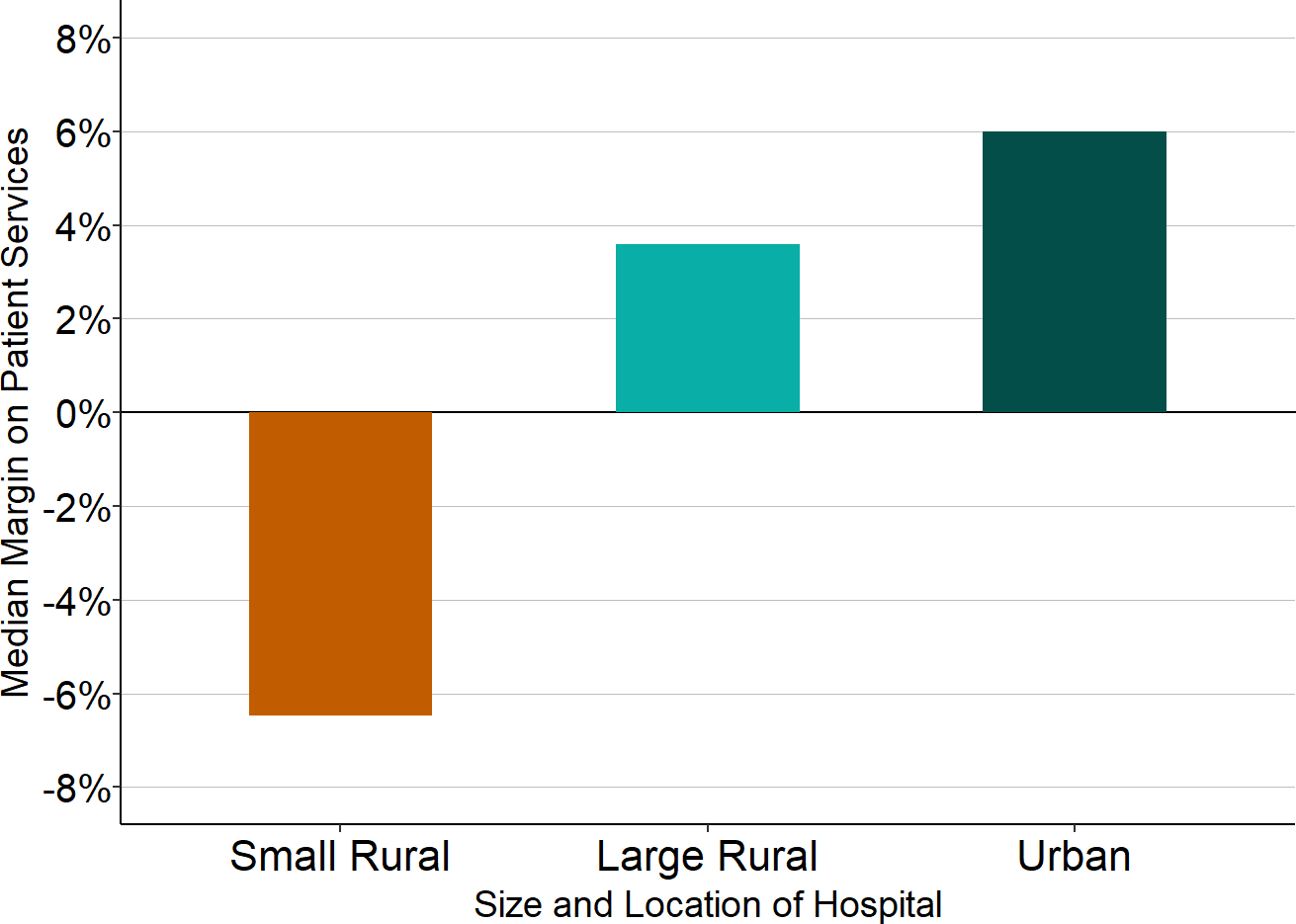
Sources: CMS Healthcare Cost Report Information System, 2023-24 Data
- Small rural hospitals lose money on patient services because of inadequate payments from private insurance plans, whereas urban hospitals and larger rural hospitals make large profits on services to patients with private insurance. Most hospitals lose money on Medicaid and uninsured patients. However, while large hospitals can offset these losses with the profits they make on patients who have private insurance, small rural hospitals cannot.
- In 2024, the median margin at small rural hospitals on services delivered to patients with private insurance (including Medicare Advantage plans) was 0%, i.e., half of the hospitals lost money on patients with private insurance. Over one-third of small rural hospitals lost more than 10% on services delivered to patients with private insurance.
- In contrast, the median profit on services to patients with private insurance was +20% at large rural hospitals and +24% at urban hospitals. One-fifth of urban hospitals made profits of over 50% on services to patients with private insurance.
- A common myth about rural hospitals is that almost all of their patients are on Medicare or Medicaid or are uninsured. In fact, on average, half of the services at small rural hospitals are delivered to patients with private insurance, only slightly lower than the percentage in urban hospitals. As a result, low margins or losses on patients with private insurance, combined with losses on Medicaid and uninsured patients, cause small rural hospitals to have large overall losses on patient services.
Figure 9
Margins on Services to Patients with Medicare, Medicaid, and Private Insurance, 2023-24
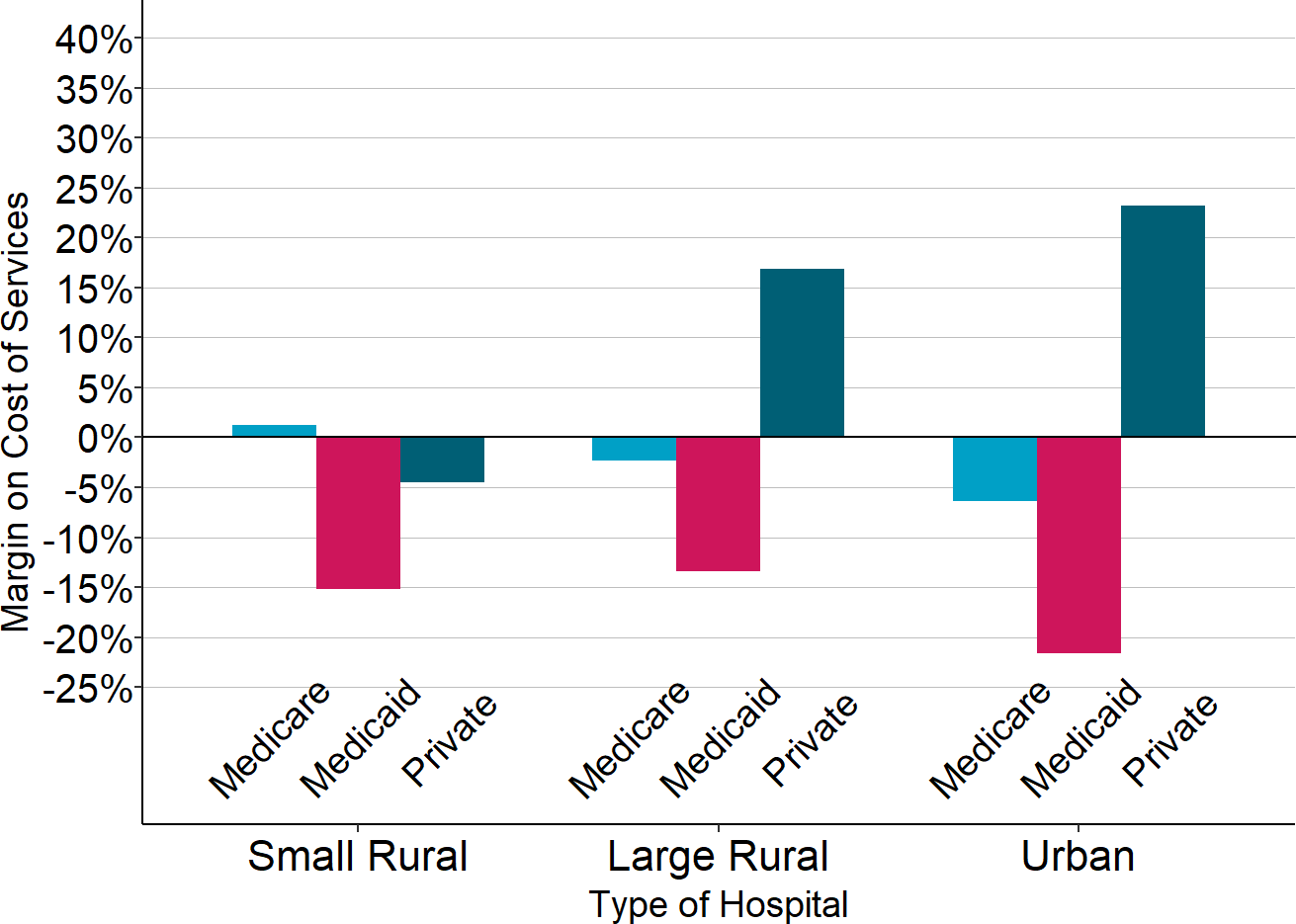
Source: CMS Healthcare Cost Report Information System
Figure 10
Percentage of Total Hospital Services Delivered to Patients With Different Types of Insurance
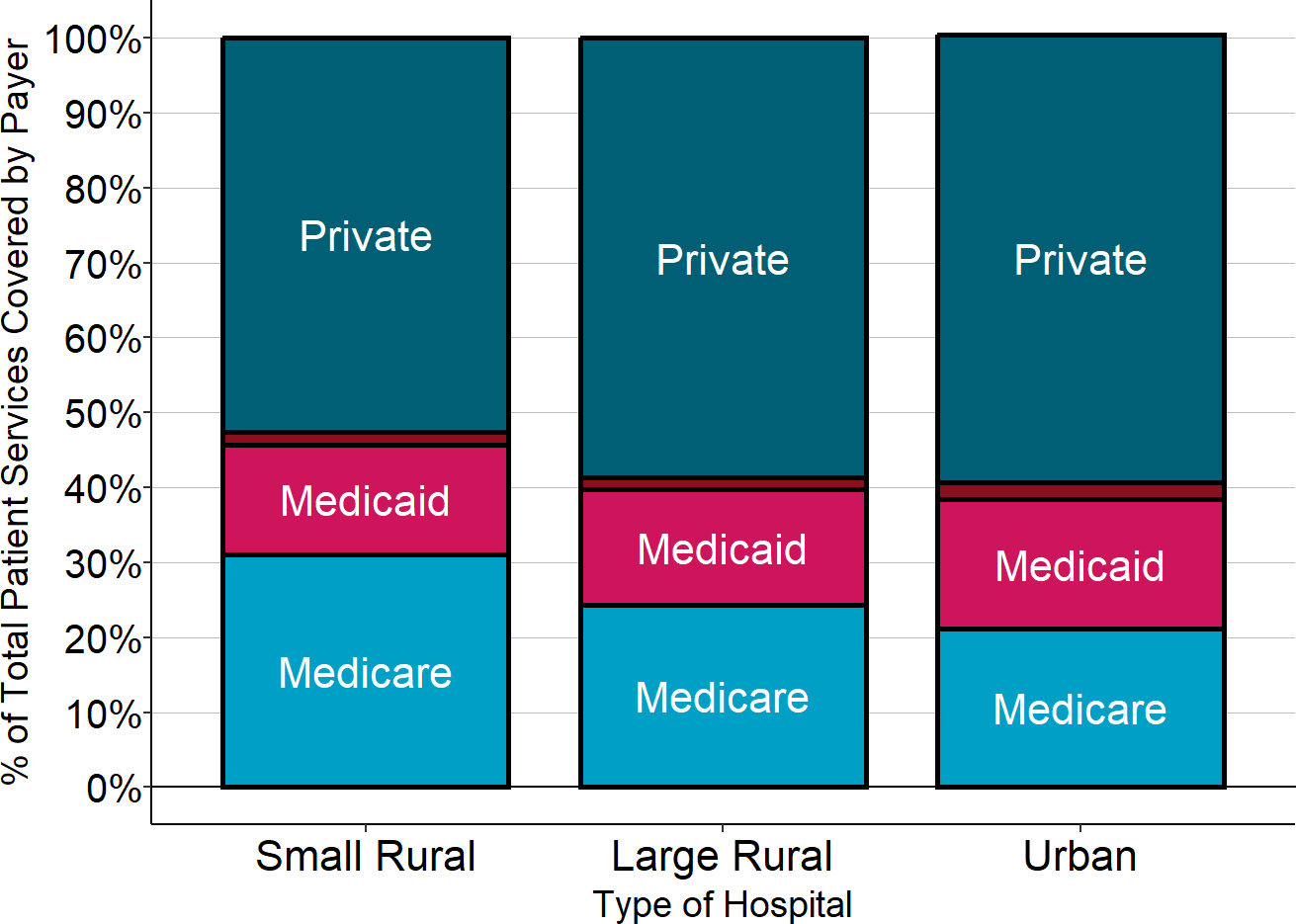
Source: CMS Healthcare Cost Report Information System
- Small rural hospitals need higher payments for essential services than larger hospitals because it costs more to deliver those services in communities with smaller populations. The average cost of an emergency room visit, inpatient day, laboratory test, or imaging study is inherently higher in a small rural hospital than at a larger hospital because there is a minimum level of staffing and equipment required to make sure these “standby” services are available on a 24/7 basis regardless of how many patients actually need to use them on any given day. For example, a hospital Emergency Department (ED) has to have at least one physician available around the clock in order to respond to injuries and medical emergencies quickly and effectively, regardless of how many patients actually have an emergency. The communities served by small rural hospitals have fewer ED visits because they have fewer residents, but the minimum cost of staffing the ED will be the same (or even higher if it costs more to recruit physicians and nurses to the rural community), so the average cost per visit will be higher. Consequently, payments that are high enough to cover the average cost per service at larger hospitals will fail to cover the costs of the same services at small rural hospitals.
- In 2017, the median small rural hospital had fewer than 4,000 ED visits per year (about 10 visits per day). In contrast, the median was over 16,000 visits per year at larger rural hospitals and over 42,000 visits at urban hospitals (10 times as many as the median small rural hospital).
- Because of the smaller number of visits, the median small rural hospital had an average cost per ED visit of $476 in 2017, 60-70% higher than the $276 cost per ED visit at the median large rural hospital and the $304 cost per ED visit at the median urban hospital.
Figure 11
Median Cost Per Emergency Dept. Visit in 2017
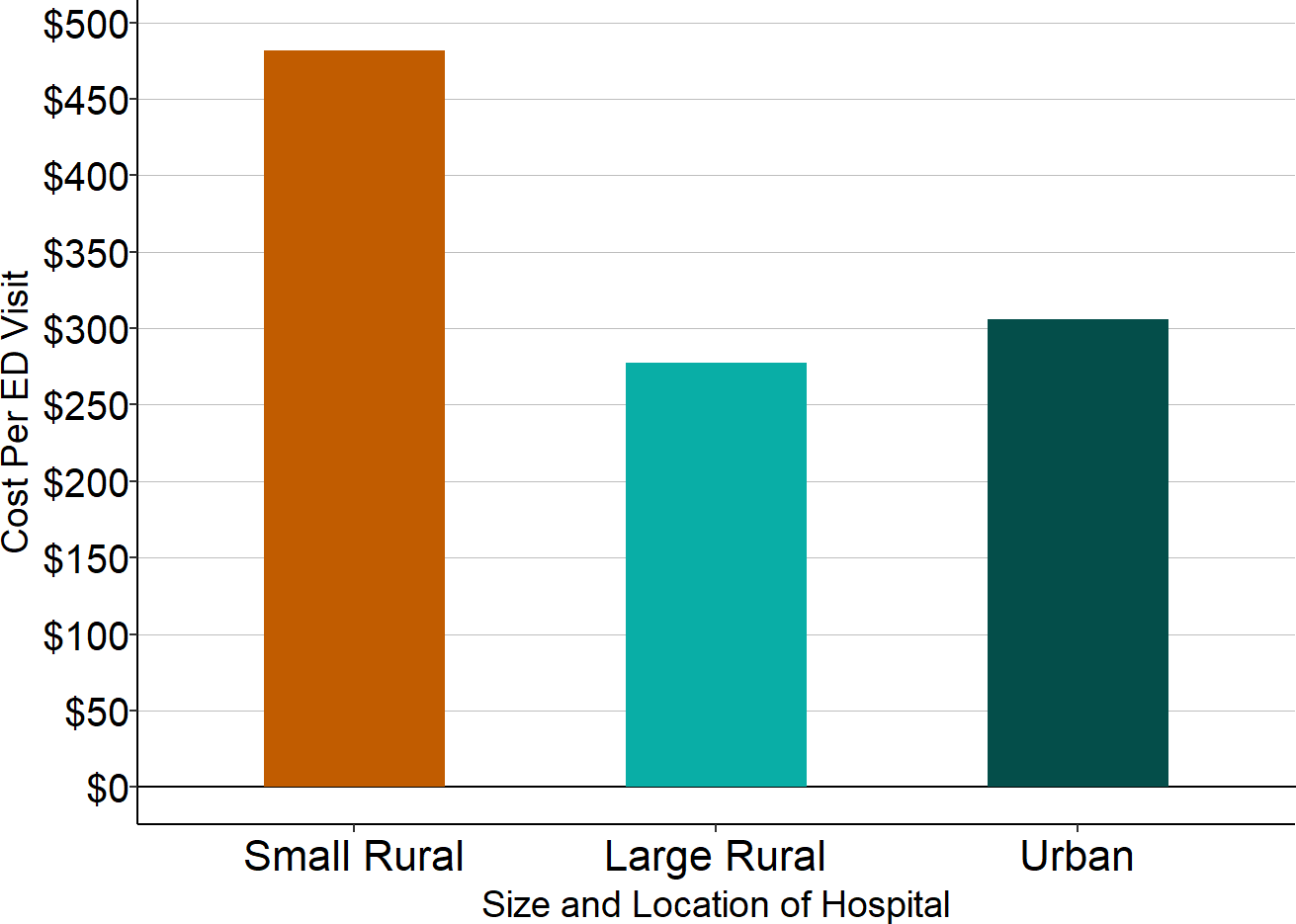
Sources: American Hospital Association Annual Survey of Hospitals, CMS Healthcare Cost Report Information System
Small rural hospitals charge less relative to their costs than urban and larger rural hospitals, which contributes to losses from private insurance plans. The prices that any hospital charges for its services have to be high enough to cover the costs of delivering the services and also high enough to offset the losses on services delivered to those patients who do not have insurance, who cannot pay the cost-sharing amounts required by their insurance, or who have an insurance plan that pays less than the cost of services. However, many hospitals charge far more than is necessary to cover their costs.
- Most urban hospitals charge more than four times as much as it costs them to deliver services. As a result, they can provide large discounts to private insurance plans and still make significant profits on their services. In 2024, the median urban hospital charged 5 times what it cost to deliver services, more than double the markup at small rural hospitals, and the median large rural hospital charged amounts that were over 3 times its costs. Nearly one-third of urban hospitals charged prices more than 6 times what it cost them to deliver services.13
- In contrast, the charges for services at most small rural hospitals are less than twice what it costs the hospital to deliver those services. In 2024, the median small rural hospital charged only 1.8 times what it cost to deliver services. As a result, small rural hospitals suffer financially when they are forced to provide large discounts to private health insurance plans.
Figure 12
Median Ratio of Charges (Prices) to Costs
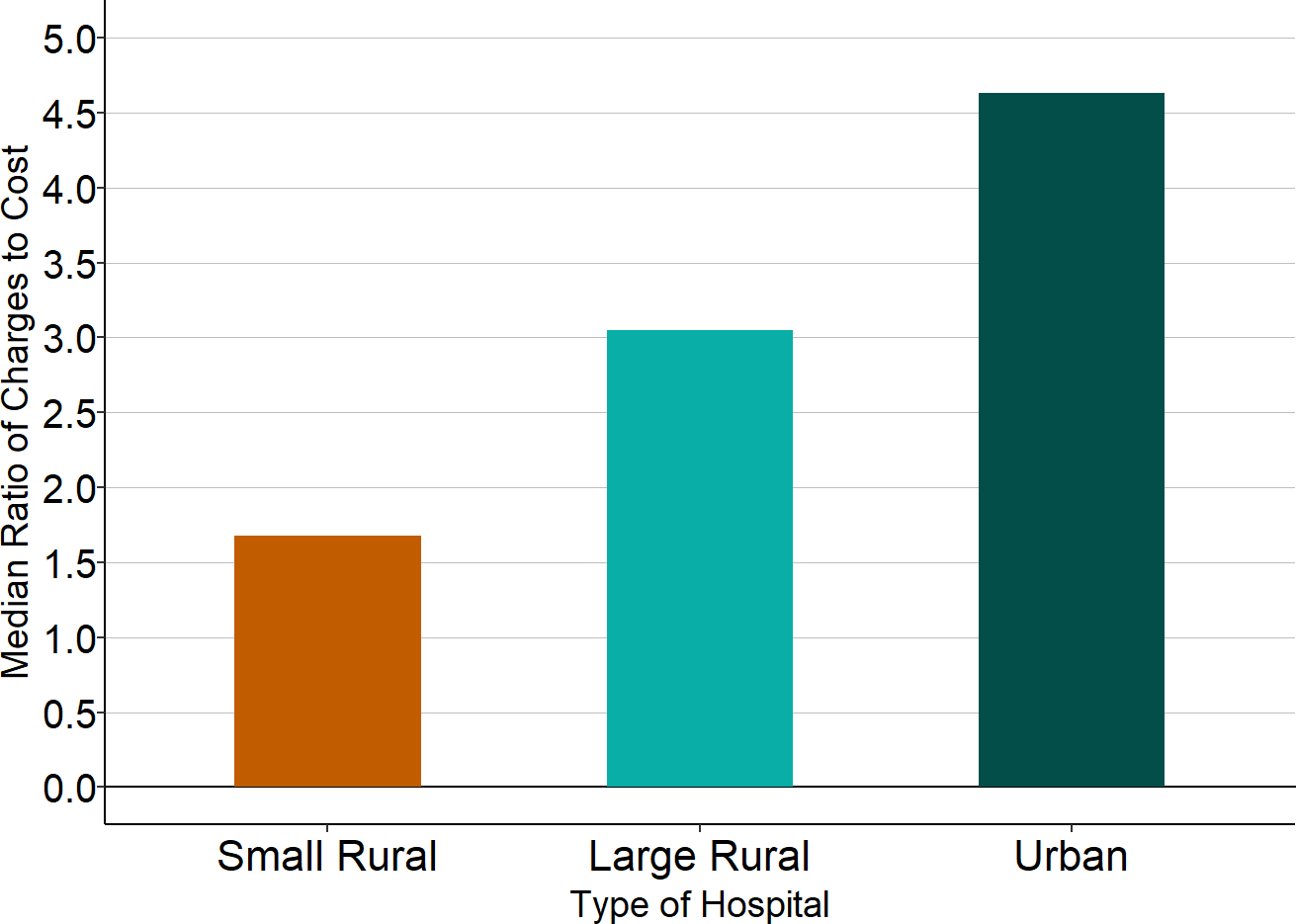
Source: CMS Healthcare Cost Report Information System
- Losses on patient services make small rural hospitals more dependent on local tax levies, government subsidies, and other sources of income than urban hospitals and larger rural hospitals. If a hospital isn’t paid enough by health insurance plans to cover the costs of delivering services to patients, the hospital has to find other sources of revenue in order to continue operating. Many small rural hospitals depend on local tax revenues, state grants, or income from investments or other businesses in order to make up the losses on the services they deliver to patients.
- Most small rural hospitals receive more than 10% of their total revenues from sources other than payments for services to patients, and one-fourth received more than 20% of their revenues that way.
- In contrast, most larger rural hospitals receive less than 7% of their revenues from sources and activities other than patient services, and most urban hospitals received less than 4% of their revenues that way.
- More than 40% of small rural hospitals are able to receive local and state tax revenues because they are government-owned or are operated by public hospital districts, compared to only 26% of larger rural hospitals and 11% of urban hospitals.
Figure 13
Median Percentage of Total Hospital Revenue from Sources Other Than Patient Services
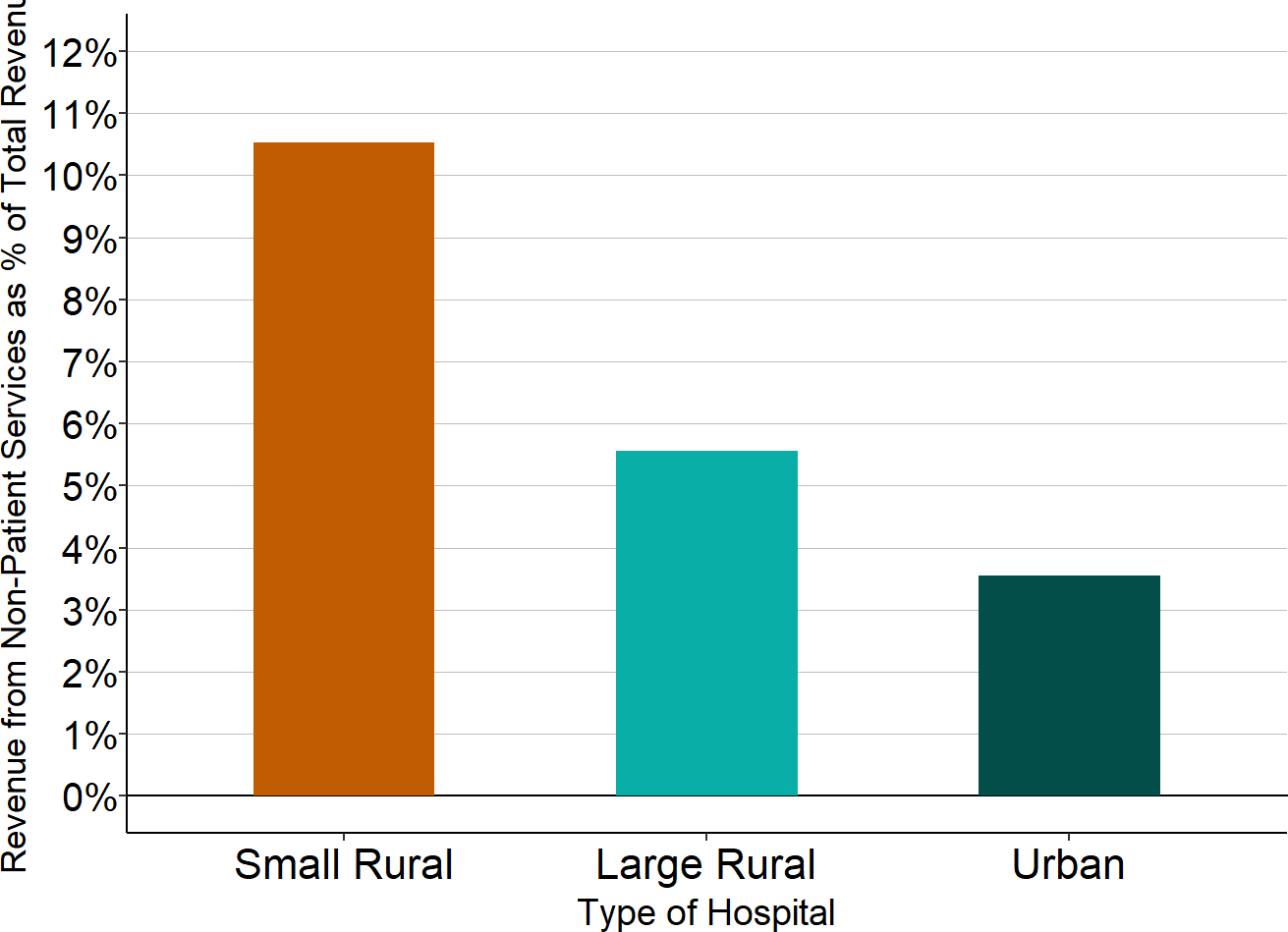
Source: CMS Healthcare Cost Report Information System
The Impacts of Small Rural Hospital Closures
If a hospital does not receive sufficient revenues from insurance payments or government funding to cover its costs over multiple years, it will ultimately be forced to close. Over 100 rural hospitals have closed in the past decade, and 80% of these closures have been small rural hospitals.14 Many more small rural hospitals would likely have been forced to close during the pandemic had it not been for the large federal grants they received.
Figure 14
Rural Hospital Closures 2015-2025
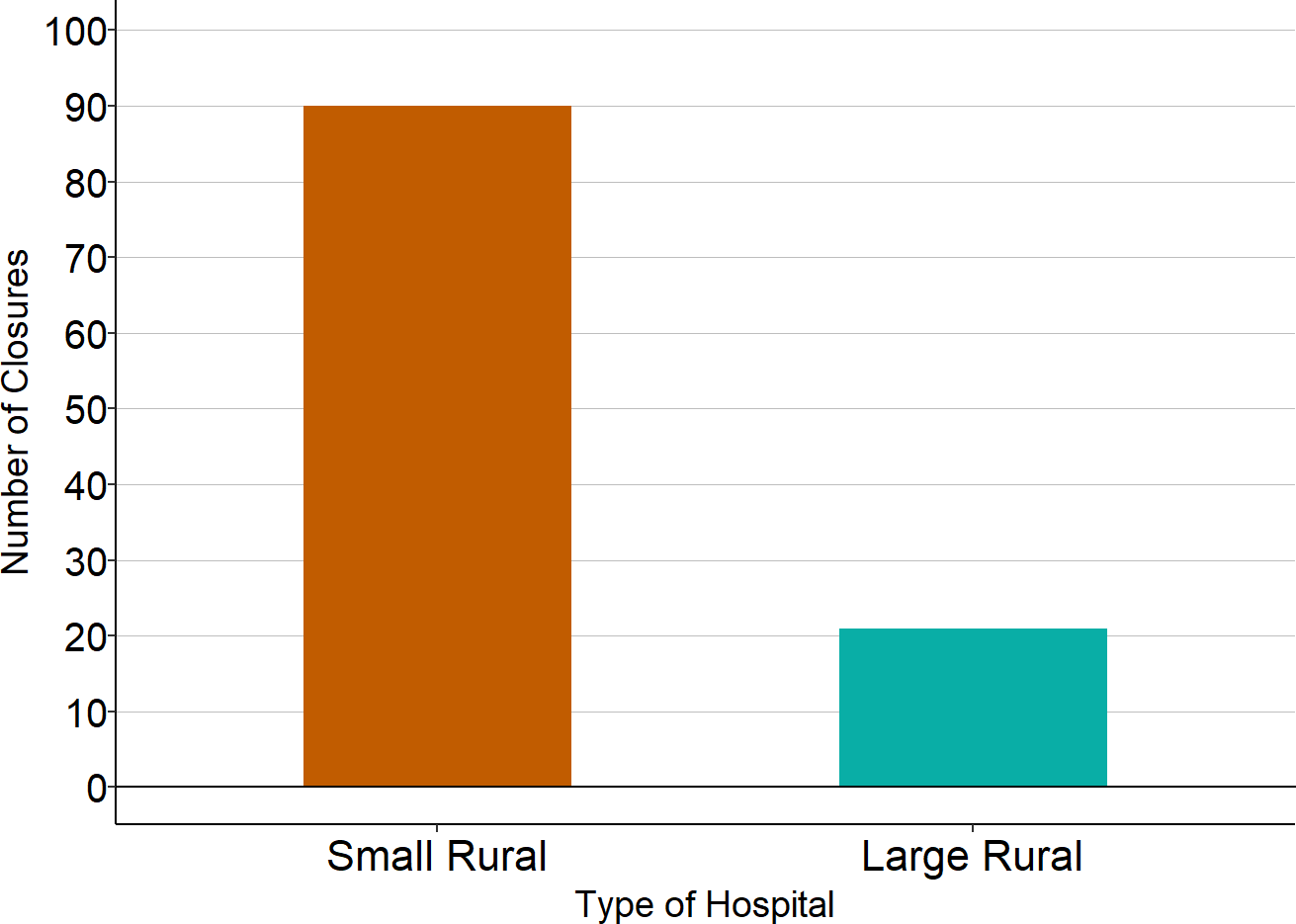
Sources: Data on hospital closures are from the Cecil G. Sheps Center for Health Services Research at the University of North Carolina and were current as of January 2025. Data on hospital size are from the CMS Healthcare Cost Report Information System. A “small” rural hospital is one that had annual expenses less than the median for rural hospitals in the year before closure. The sizes of 7 hospitals could not be determined because cost reports were not available.
In a small percentage of cases, the hospitals that “closed” didn’t completely shut down, and there is still an emergency room and other services operating at the same location.15 In other cases, the hospital did shut down, but there is another hospital located less than a 15-minute drive from the hospital that closed, or even in the same town.16 For example, one rural hospital that closed was a small physician-owned hospital that had been located a block away from a larger facility that still continues to operate.17
However, in most cases where small rural hospitals have closed, there is no longer an ED in the community or nearby.18 In many cases, the nearest ED is 30 minutes or more away, and those people who already had to travel a distance to reach the hospital that closed now have to travel 45 minutes or more to reach a hospital. These types of closures cause two different kinds of problems for the residents of the community:
- Delays in Receiving Emergency Care. The most serious problems occur when an individual experiences a medical emergency, such as a serious injury or symptoms of a heart attack or stroke, and they need to quickly reach an emergency room. Studies have found that mortality rates for heart attack, stroke, respiratory problems, and life-threatening injuries are higher for people who have to travel farther to reach a hospital emergency department.19 Because of the greater travel times in rural areas, closure of a small rural hospital is likely to have a greater negative impact than closure of a small hospital in an urban area; in fact, a study of hospital closures in California found that closures of rural hospitals increased mortality for both heart attacks and strokes, but closures of urban hospitals had no negative impact on mortality.20 Several studies have found that mortality rates for heart attacks were as much as 30% higher following closures of emergency departments that increased travel times by 30 minutes or more, with more limited impacts when travel times increased by 10-30 minutes.21 Although a helicopter ambulance could potentially transport an emergency patient to an alternative hospital more quickly than the time required to drive to a local hospital, this depends on whether a helicopter ambulance is available and whether the weather is safe for flying. A helicopter ambulance trip is extremely expensive, so the cost of this service will be much higher than a visit to a nearby emergency room. Many patients with non-life threatening injuries, chest pain, or other symptoms will not need surgical intervention or other types of treatment that can only be provided at tertiary or quaternary hospitals, and it is much more cost-effective to triage and treat these cases in a local hospital than at a distant hospital that requires air transport to reach.22
- Failure to Receive Important Non-Emergency Care. Patients who are not experiencing an emergency also have to travel farther to receive many types of preventive, diagnostic, and non-emergency treatment services if there is no nearby hospital. The greater the time, distance, and cost of travel, particularly during the winter or bad weather, the less likely it is that patients will obtain those services in a timely fashion. Delays in diagnosis or treatment can result in more serious health problems and more expensive treatment than if the patient had been able to obtain services more easily and quickly. For example,
- Maternity Care. There is growing concern about the high rates of both maternal death and infant mortality in the country, both of which are significantly higher in rural areas.23 Successfully addressing these problems requires that women receive regular prenatal care during pregnancy and that both the mother and infant receive high-quality care after birth, but these services are less likely to be available in a community that lacks primary care and obstetric care. It is also important that women with higher-risk pregnancies receive timely, high-quality care during childbirth, and that is less likely if the woman has to travel a long distance to reach a hospital. One study found that rural counties not adjacent to urban areas that lost hospital-based obstetric services had significant increases in preterm births.24
- Monitoring of Chronic Conditions. The highest-volume service at most hospitals, both urban and rural, is laboratory testing. Many patients with chronic conditions such as diabetes and heart disease need regular testing in order to properly manage their conditions, and failure to do so can lead to serious complications.
- Prompt, Accurate Diagnosis of New Symptoms. Many diseases can only be accurately diagnosed through appropriate testing, and delays in testing can result in delayed or incorrect treatment. For example, one study found that patients with colon cancer who had to travel more than 50 miles for diagnosis were significantly more likely to have advanced disease at the time of diagnosis.25 If the patient has an infectious disease (such as during the coronavirus pandemic in 2020), delayed or inaccurate diagnosis and treatment can harm many others in the community.
EXAMPLE: Nye Regional Medical Center
The most isolated hospital that closed in recent years was the Nye Regional Medical Center in Tonopah, Nevada. Tonopah is the county seat of Nye County, the county that is the third-largest in land area in the country outside of Alaska.26 Originally a gold mining town, Tonopah is located near the midpoint of the more than 400-mile drive between Las Vegas and Reno. Although Tonopah has only about 2,000 residents, Nye County has more than 50,000 residents, spread over 18,000 square miles of land.27
Figure 15
Nye Regional Medical Center
(With Surroundings in Nevada and California)
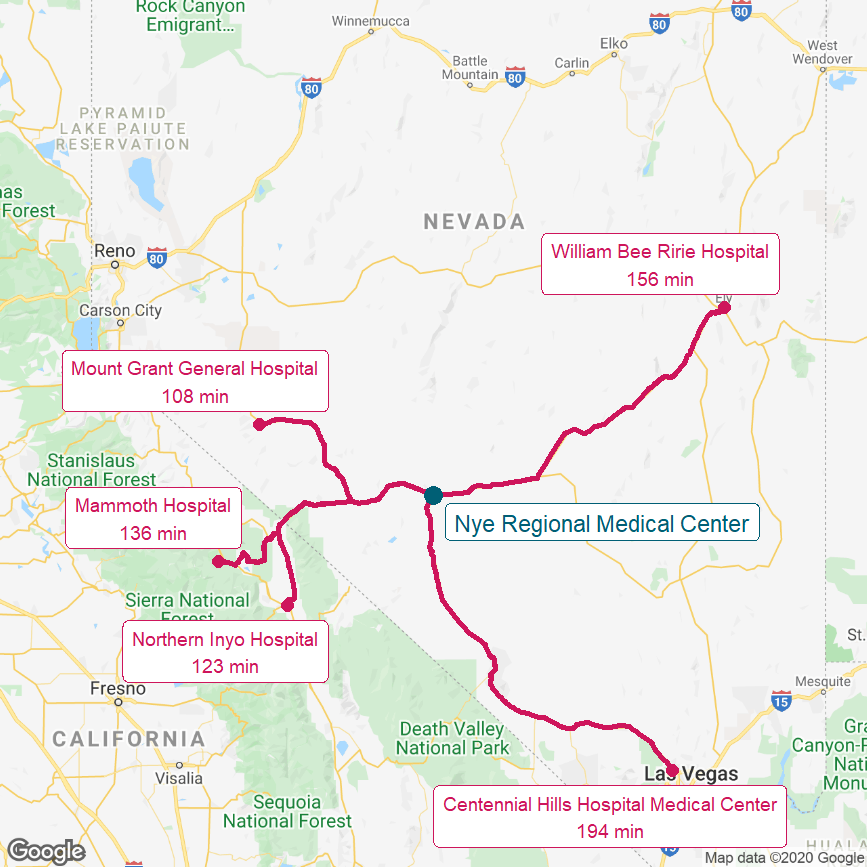
The red lines show the most direct driving routes between the hospitals and the estimated travel times.
The hospital closed in 2015 after years of financial problems and filing for bankruptcy in 2013.28 As shown in the map of the area, the closest hospitals to the community are over two hours away in northern California and Nevada, and more than a three-hour drive is required to reach the hospitals in Las Vegas.
The Emergency Department provided emergency treatment both for residents of the community and for travelers on U.S. 95, the major north-south route through western Nevada that passes through the town. The hospital also served as a principal source of primary care and outpatient services for community residents. Although ambulance services have been enhanced and clinics were established in an effort to fill some of the gaps in healthcare services caused by the closure, the area still has no 24-hour emergency treatment facility and lacks many other healthcare services. Local businesses report that the lack of a hospital has made it more difficult to attract employees, and that workers may have to take off a day or more of work in order to get more than basic medical testing.29 The residents of the community have formed a hospital district supported by local property taxes in the hope of being able to reopen a hospital in the community.30
EXAMPLE: DeQueen Medical Center
The DeQueen Medical Center closed in May 2019, after having financial difficulties for many years.31 The 25-bed Critical Access Hospital was the only hospital in DeQueen, Arkansas and surrounding Sevier County, which are located in the southwestern corner of the state next to Oklahoma.
Figure 16
DeQueen Medical Center
(With Surroundings in Arkansas
and Eastern Oklahoma)
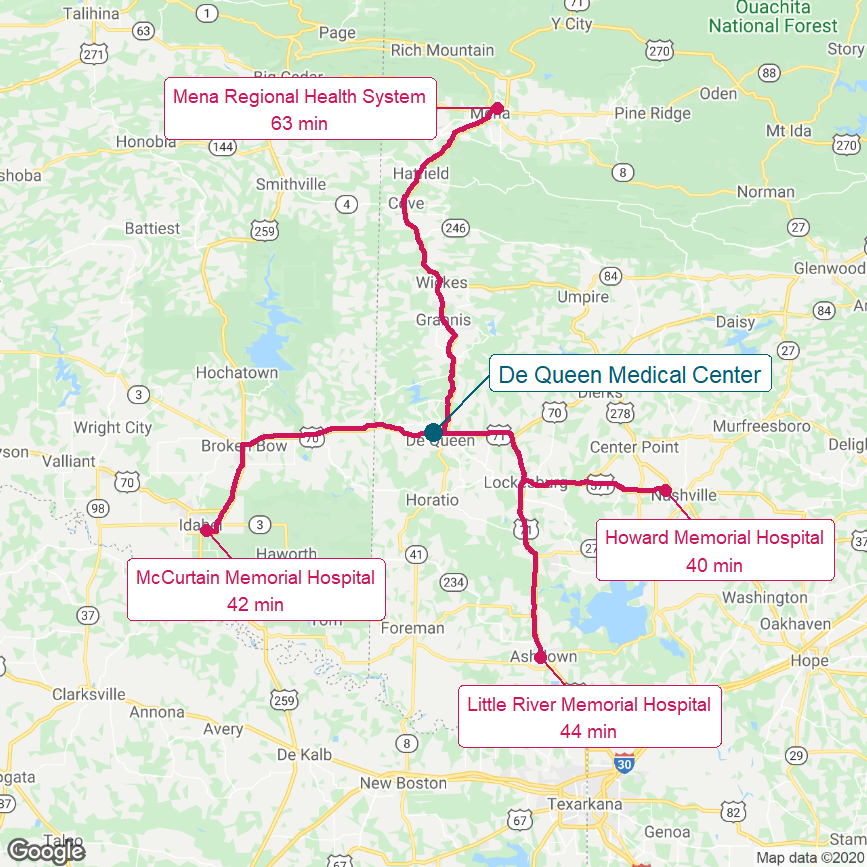
The red lines show the most direct driving routes between the hospitals and the estimated travel times.
As shown in the map of the area, after the closure, the closest emergency rooms and other hospital services were 40 minutes away for the 6,200 residents of DeQueen and the thousands of additional people who live in the immediately surrounding community. The median income in Sevier County is significantly below the national average ($47,900 vs. $70,784) and the poverty level is nearly twice the national average (19.8% vs. 11.6% in 2019), so it is likely that many residents would have difficulty traveling that far in order to receive healthcare services. The three closest hospitals are also small Critical Access Hospitals, each of which has experienced financial losses in recent years.
As the coronavirus spread across the nation in 2020, the lack of a hospital in DeQueen was particularly problematic because Pilgrim’s Pride operates a large poultry processing plant there, and poultry and meatpacking plants were sites of significant outbreaks of COVID-19.32 At the end of June, 2020, Sevier County had had more than 700 COVID-19 cases, representing one of the highest per capita infection rates in the U.S.33
Sevier County issued bonds to finance construction of a new hospital34, and the new hospital, renamed the Sevier County Medical Center, reopened in 2023, but it is unclear whether or how the new hospital will avoid the financial problems that caused the previous hospital to close.
The Importance of Rural Hospitals to the Rest of the Country
In addition to negatively impacting the health of local residents, the closure of a rural hospital can harm the economy of the local community. The community will not only lose the large number of jobs at the hospital, it will also be more difficult for the community to attract and retain businesses and workers in other industries.35
However, the negative impacts of a rural hospital closure are not limited to the community where it was located. Closures can also negatively affect the residents of urban areas located far away because of the important role rural communities play in the nation’s overall economy:
Figure 17
Agricultural and Mining/Oil/Gas Production
in Counties Dependent on Rural Hospitals
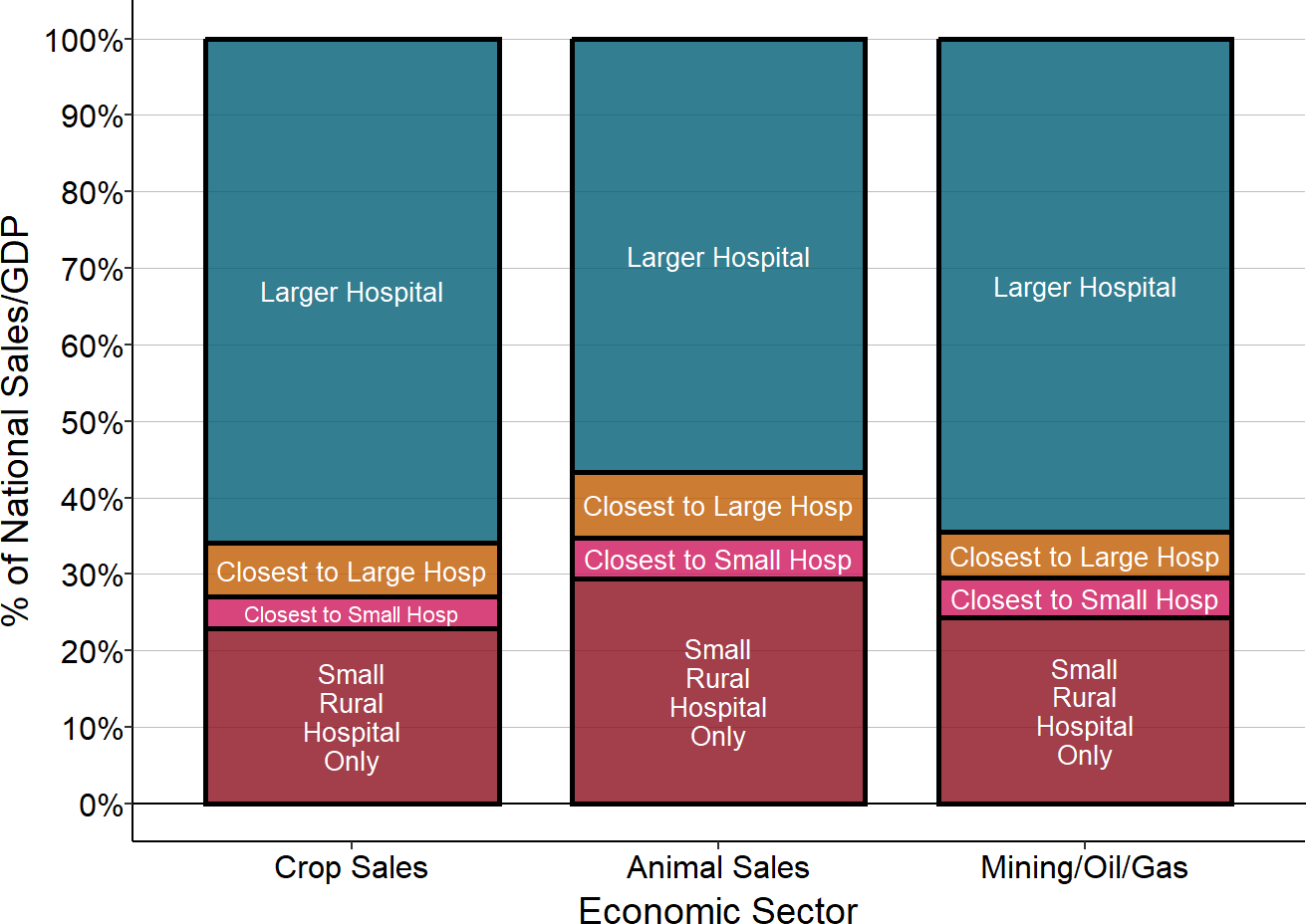
Source: 2017 Census of Agriculture, BEA 2021 Gross Domestic Product by County, CMS Provider of Services Files. “Close to Small” means the county has no hospital and the closest hospital is a small rural hospital.
- Food Supply. Most of the nation’s food supply comes from rural communities because of the large amounts of land needed to grow crops and raise cattle. Rural hospitals provide healthcare services to the owners and workers on the farms and ranches in these areas, to the owners and workers at the businesses that supply the farms and ranches, and also to their family members. Many of these hospitals are small because of the low population densities in agricultural areas.
- 23% of agricultural crops are produced in counties in which the only hospitals are small rural hospitals. An additional 4% of crops come from counties that have no hospital at all and the closest hospital is a small rural hospital in another county.36
- 29% of the country’s production of animals for food occurs in counties in which the only hospitals are small rural hospitals. An additional 8% are in counties that have no hospital at all and the closest hospital is a small rural hospital in another county.
- Energy Production. Rural communities are home to most of the nation’s coal mining and gas and oil production, as well as wind farms and solar energy facilities, and many of those communities rely on small rural hospitals for healthcare services. 24% of the country’s mining and oil and gas production occurs in counties in which the only hospitals are small rural hospitals. An additional 6% of fossil fuel production comes from counties that have no hospital at all and the closest hospital is a small rural hospital.37
- Recreation and Tourism. Many popular recreation, historical, and tourist sites are located in rural areas. If visitors to these sites have accidents or health problems that require medical treatment, their initial care will often be provided by a small rural hospital. For example, the top 10 most-visited National Parks, including the Grand Canyon, Yosemite, and Yellowstone, had almost 50 million visits in 2019, and all are located in rural areas.38 In four of the parks, the closest hospital to at least one of the entrances and visitor centers at the Park was a small, rural hospital. 39
- Shipping and Other Travel. Interstate highways connect the nation’s urban areas to each other, to the nation’s agricultural areas, and to recreation sites, and they pass through rural areas to do so. A trucker, traveler, or tourist who has an accident or medical problem on an interstate highway is likely to depend on a small rural hospital located near a highway interchange for emergency care.
The coronavirus pandemic in 2020 made many city dwellers realize for the first time how dependent they are on rural communities for their food supply and how much that supply could be affected by health problems in rural communities.40 The pandemic has also made healthy individuals all across the country realize how important it is to have hospitals with adequate capacity, not only where they live or work, but where they might be quarantined during travel.
Example: Hospitals in Eastern Washington State
One of the largest agricultural areas in the U.S. is located in Washington State east of the Cascade Mountains. This region produces over $8 billion in agricultural products each year, including almost half (49%) of the nation’s apples, 18% of the potatoes, and 8% of the country’s wheat, as well as other fruits, vegetables, grains, and livestock. The 20-county region includes 2 of the top 10 counties in the country in terms of total agricultural sales, 7 of the top ten apple-producing counties in the country, 4 of the top 10 wheat-producing counties in the country, 3 of the top 10 potato-producing counties in the country, and 2 of the top 10 vegetable-growing counties in the nation.41
This area is also a popular destination for tourists and vacationers because of the Cascade Mountains, the Columbia River, and other natural features.42
Figure 18
Hospitals in Eastern Washington State
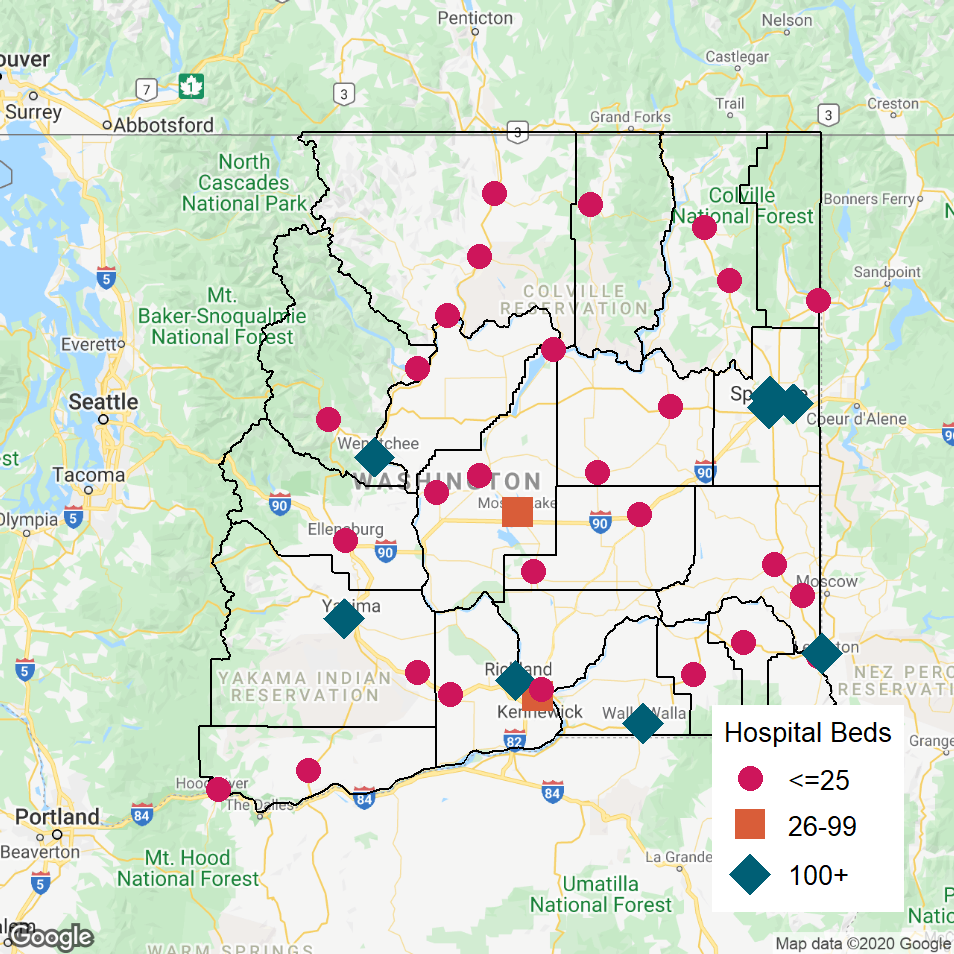
Ready access to quality healthcare in this area is particularly important for the nearly 200,000 farmworkers who support the agricultural industry, including more than 50,000 migrant workers, since injuries are common on farms and ranches because of the manual nature of the work. For example, farm workers must stand on ladders to pick apples by hand. Tourists and visitors also experience injuries while boating, hiking, and skiing.
As shown in the map of the area, 38 hospitals provide services in the region. The largest hospitals are located at the eastern end of the region in Spokane, and in the southern and southwestern portions of the region (in Kennewick, Richland, Walla Walla, Wenatchee, Yakima, and Lewiston, Idaho).
Most (27) of the hospitals are Critical Access Hospitals with 25 or fewer beds. They are primarily located in the northern and central parts of the region and in the southeastern and southwestern corners. The majority (17) of these are small rural hospitals with an average of less than 4 acute inpatients per day, but inpatient care represents only a small proportion of the healthcare services the hospitals provide to their communities. In addition to 24-hour emergency care at all of the hospitals (the majority have over 3,000 ED visits per year), 90% of the hospitals provide skilled rehabilitation and long-term nursing care services, and over 80% operate one or more Rural Health Clinics.
Over two dozen Critical Access Hospitals might seem like a lot for a region with 1.6 million residents until one realizes that those residents are spread out across a 42,000 square mile region, most of which is farmland. Five of the 20 counties have fewer than 10 residents per square mile. Moreover, it would be impossible to have fewer, larger hospitals in the northern and central portions of the region because the topography – mountain passes, deep river gorges, and canyons – would prevent most people from using them.
For example, the first map below shows the communities and hospitals in the Columbia River valley from Wenatchee north to Tonasket and east to the Grand Coulee Dam and Republic. The seven small Critical Access Hospitals in the area are each at least a half hour drive away from the next-closest hospital, which in almost every case is yet another small Critical Access Hospital. The closest large hospital to these communities is in Wenatchee, which requires a one-to-two-hour drive along two-lane roads from most of the communities.
Similarly, in the central and southern portions of the region, the only large hospitals are located at the very edges of the region, so ten 25-bed Critical Access Hospitals and one 50-bed hospital (designated by Medicare as a Sole Community Hospital) provide emergency care, inpatient and outpatient hospital care, and primary care to the farming communities in the interior of the region as well as emergency care for tourists and those traveling along Interstate 90. As shown in the second map, each of these hospitals is a half-hour or more away from the next-closest hospital, which in many cases is another small Critical Access Hospital. Many workers, residents, and visitors in the areas served by each hospital already have to travel a distance to reach that hospital, and an alternative hospital could be an hour away. For example, Dayton General Hospital is a half hour drive from the Bluewood Ski Resort, and it would take over an hour to reach the next closest hospital in Walla Walla.
The majority of the small rural hospitals in Eastern Washington State lose money on patient services. In contrast, most of the larger hospitals make profits on patient services. In most cases, the small hospitals are only able to continue operating because they are structured as Public Hospital Districts and local residents and businesses tax themselves to keep the hospitals open.43
Figure 19
North Central Washington State
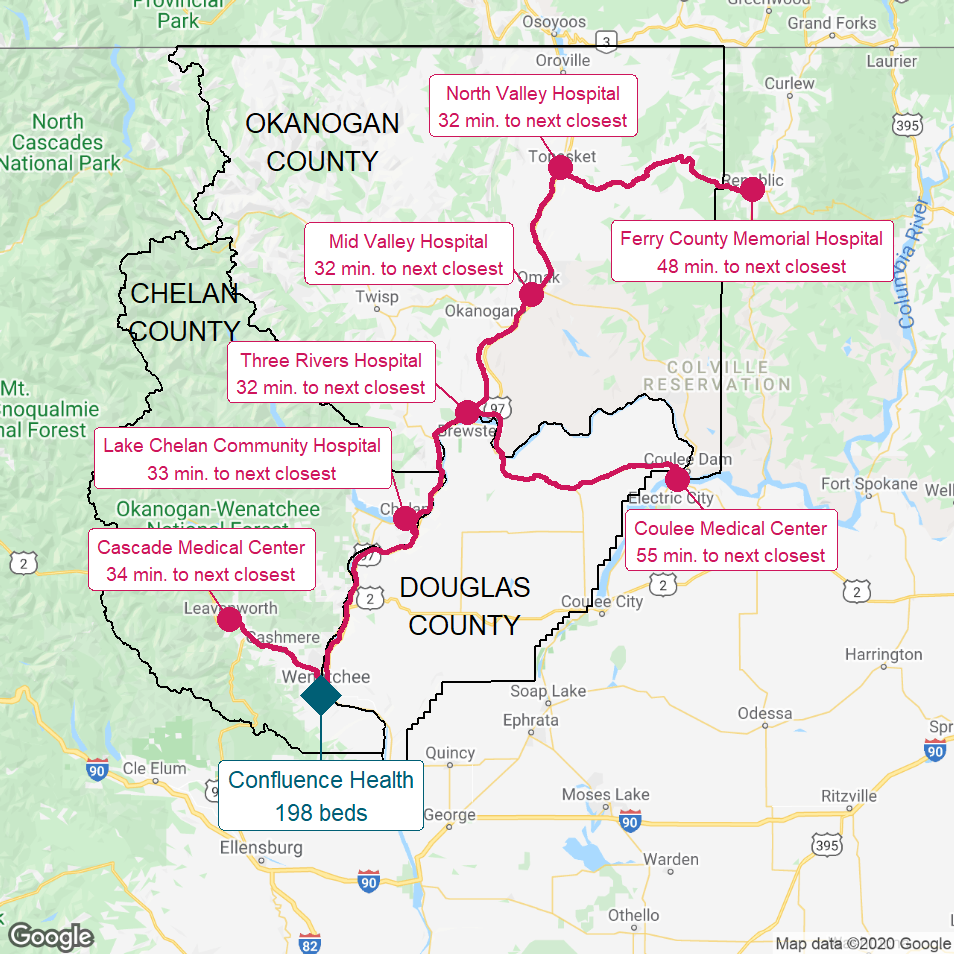
The red lines show the most direct driving routes between the hospitals and the estimated travel times.
Figure 20
Southeastern Washington State
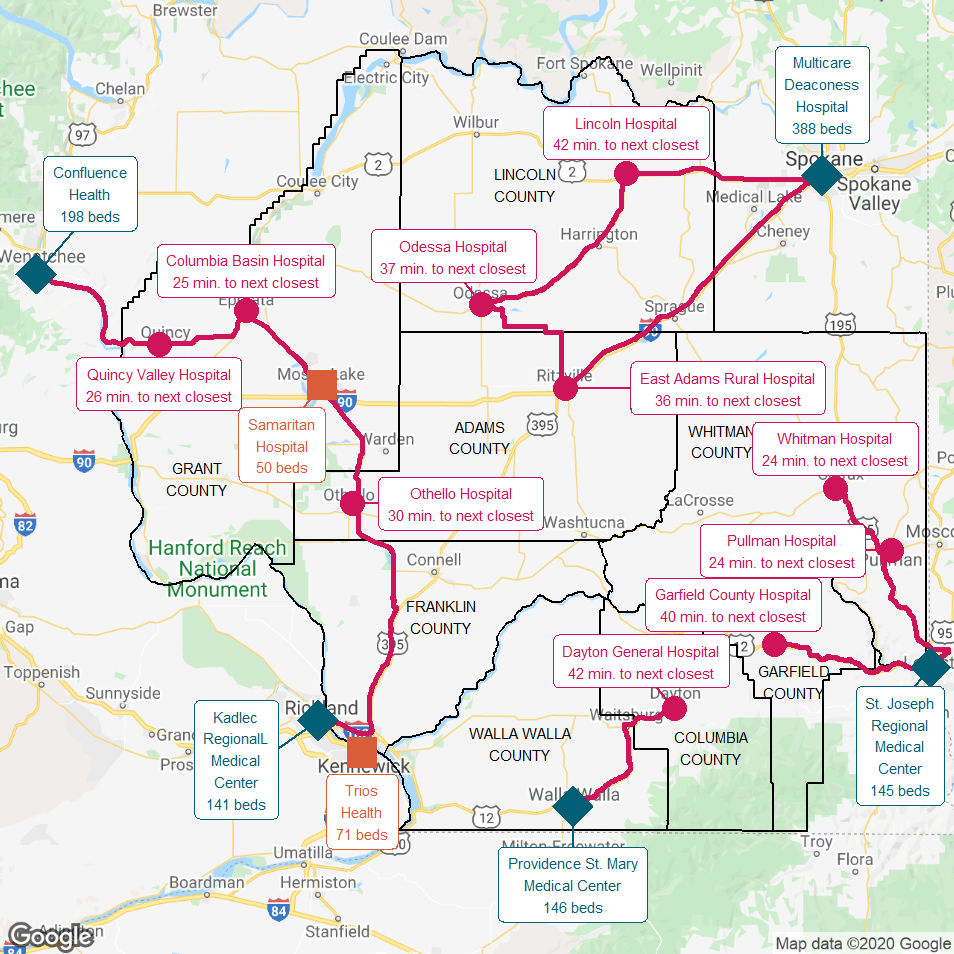
The red lines show the most direct driving routes between the hospitals and the estimated travel times.
Policies to Control Healthcare Spending Need to Differentiate Small Rural Hospitals and Larger Hospitals
Clearly, there are very significant differences between small rural hospitals and larger hospitals, both urban and rural. These differences have important implications for designing policies that control or reduce spending on hospital services while ensuring access to essential health services for citizens in all parts of the country:
- Little in the way of savings can be achieved by reducing payments to small rural hospitals. Although small rural hospitals represent 25% of the short-term general hospitals in the country, they receive less than 3% of national spending on hospital services, and they account for only 2% of the significant increase in national hospital spending that has occurred in recent years. Revenues at small rural hospitals increased by a total of $13 billion nationally from 2014 to 2024, compared to an increase of nearly $600 billion at urban hospitals. Even a large reduction in spending on services at small rural hospitals would have only a minuscule impact on total national healthcare spending.
Figure 21
Total National Spending on Short-Term Acute Hospitals (Billions)
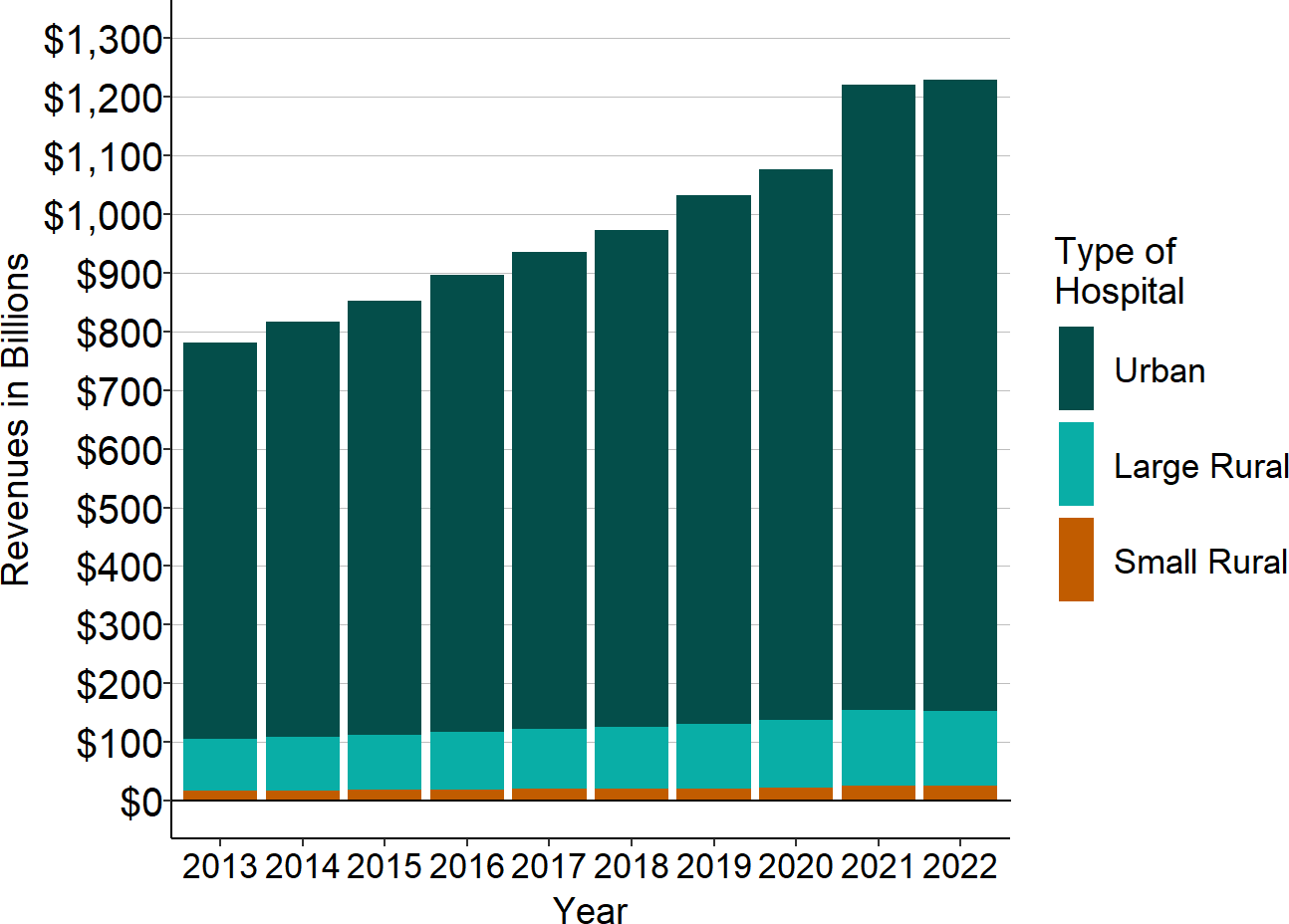
Source: CMS Healthcare Cost Report Information System
- Reducing payments to small rural hospitals will accelerate closures and reduce access to services for rural communities. Policies and programs designed to reduce spending on hospitals by cutting payments for hospital services or reducing utilization of hospital services will have a far more negative impact on small rural hospitals than larger hospitals, because profit margins at most small rural hospitals are already low or negative. Even a small reduction in revenues at small rural hospitals could force more of them to close. Although revenues decreased for most hospitals in 2020 due to the coronavirus pandemic, the majority of urban hospitals and large rural hospitals remained profitable, whereas an even higher proportion of small rural hospitals lost money on patient services. Many small rural hospitals were only able to continue operating because the special federal assistance provided to hospitals during the pandemic enabled them to offset these losses.
Figure 22
Aggregate National Hospital Profits on Patient Services (Billions)
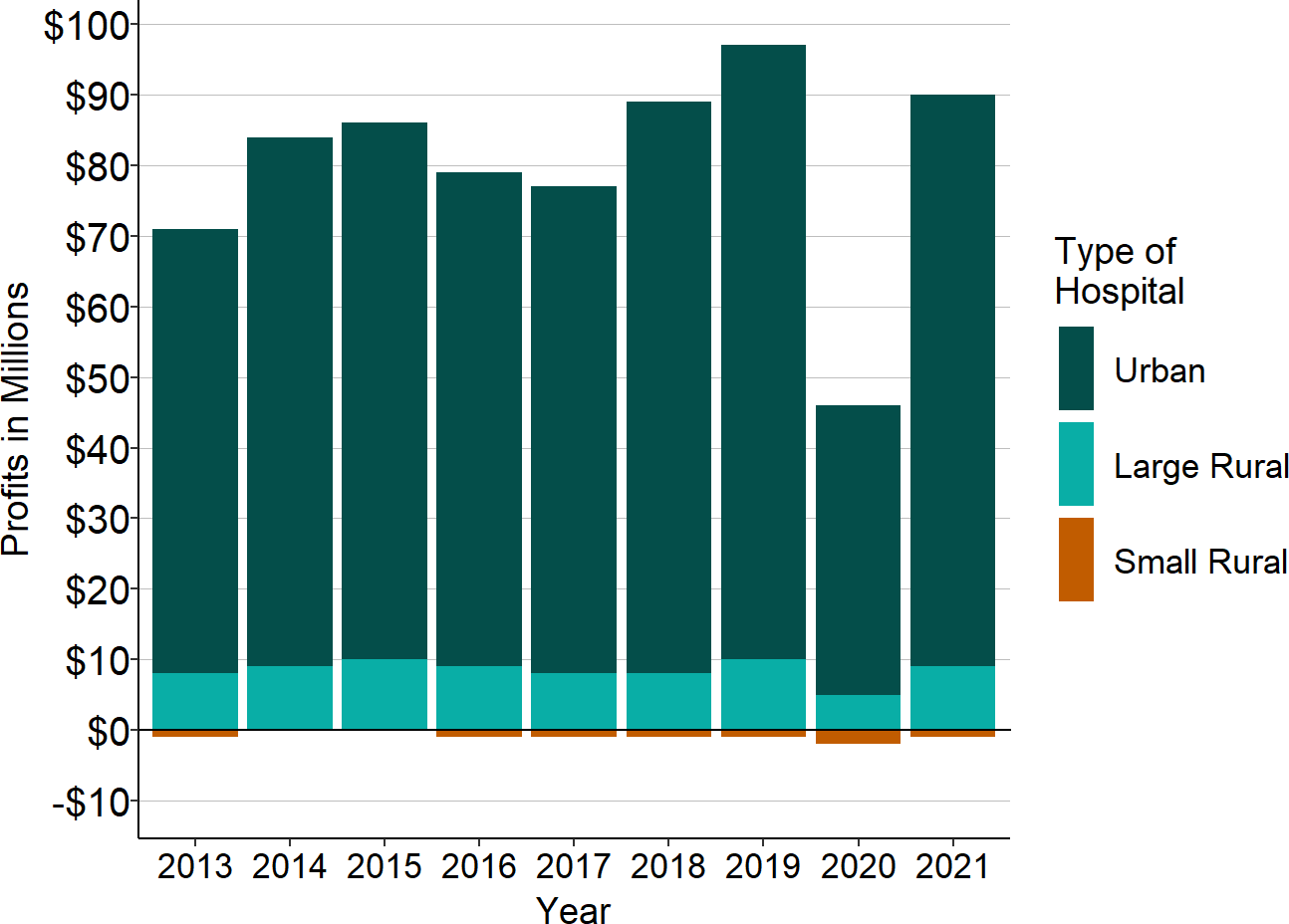
Source: CMS Healthcare Cost Report Information System
Preserving Access to Essential Healthcare Services in Small Rural Communities
There is little to be gained by reducing spending on small rural hospitals and much to be lost by doing so. Conversely, providing adequate payments to small rural hospitals could preserve access to essential healthcare services for rural communities with minimal impact on overall healthcare spending. The losses on patient services at all of the small rural hospitals in the country could be eliminated for only $2 billion per year – an amount that is less than two-tenths of one percent of current national spending on all hospitals.
Unfortunately, many proposals that are ostensibly designed to help rural hospitals would either fail to solve their problems or actually make things worse rather than better. For example, a new federal Rural Emergency Hospital program has been promoted as a way of preventing rural hospital closures. However, it would require a small rural hospital to close its inpatient unit, thereby eliminating a service that proved to be essential in most communities during the pandemic, and there would be no assurance that the payments for the hospital’s outpatient services would be adequate to cover the cost of delivering hospital services in rural areas. Moreover, while most proposals for helping small rural hospitals have focused on changing payments under Traditional Medicare, the primary cause of financial losses at small rural hospitals has been inadequate payments from private health insurance plans (including both employer-sponsored insurance and Medicare Advantage plans).
Creating policies that will successfully prevent additional closures and support high-quality healthcare services for small rural communities requires a clear understanding of what is causing the financial problems at small rural hospitals. Not every small rural hospital is losing money, and there are larger rural hospitals that are also at risk of closing. Rural hospitals do better financially in some states than others, and the biggest differences are not due to whether the state has expanded Medicaid eligibility. Some rural communities are smaller or more isolated than others are and their hospitals need to provide a broader range of services. As a result, one-size-fits-all policies are unlikely to address the needs of every rural community.
Moreover, careful analysis shows that the problems experienced by small rural hospitals are not only due to the inadequate amounts the hospitals receive for the services they deliver, but also the problematic method payers use to pay for services. Sustaining and strengthening rural healthcare services requires paying for those services in a better way.
Footnotes
U.S. Department of Health and Human Services, Center for Medicare and Medicaid Services. National Health Expenditure Accounts.↩︎
U.S. Department of Health and Human Services, Center for Medicare and Medicaid Services. National Health Expenditure Accounts.↩︎
U.S. Department of Commerce, Bureau of Economic Analysis. National Income and Product Accounts: Personal Income.↩︎
As used here, a “short-term general hospital” is a hospital that (1) has an emergency department, (2) provides inpatient care lasting from a few days to a much longer period of time, and (3) treats a wide range of acute conditions. This does not include specialty hospitals that only treat a narrow set of conditions, such as psychiatric hospitals and orthopedic surgery hospitals, long-term acute care hospitals that focus on patients who require a month or more of inpatient care, and rehabilitation hospitals that help patients recover after treatment in an acute care hospital.↩︎
A hospital is described as a “rural hospital” here if it is located in an area that is classified as rural by the Health Resources and Services Administration. Based on the revised definition established in 2021, an area is rural if either (1) it is in a county classified as “non-metropolitan” by the U.S. Office of Management and Budget (OMB); or (2) it is in a county classified as “metropolitan” and is either (a) in a census tract with a Rural-Urban Commuting Area (RUCA) Code of 4.0 or higher, or (b) in a census tract with a RUCA Code of 2 or 3 that is at least 400 square miles in area and has a population density of 35 persons per square mile or less, or (3) it is in a county classified as “metropolitan” that does not contain any urbanized area (which is defined by the U.S. Census Bureau as an incorporated place with 2,500 or more residents). A few hospitals have been reclassified as “rural” here even though they are located in a census tract that is classified as urban because they are in a zip code that is primarily rural. Other federal agencies, including the Centers for Medicare and Medicaid Services, only consider a hospital to be “rural” if it is located in a non-metropolitan county, and exclude hospitals located in rural portions of metropolitan areas. This is why many reports with statistics on hospitals indicate that there only about 1,800 rural hospitals in the country.↩︎
The addresses of hospitals were obtained from the publicly-available Provider of Services (POS) File maintained by the Center for Medicare and Medicaid Services (CMS). Hospital latitude and longitude coordinates were determined from the hospital address using the Google Maps Geocoding API. Driving distances between hospitals were calculated using the Google Maps Distance Matrix API.↩︎
The number of licensed inpatient beds at each hospital was obtained from the Provider of Services (POS) File maintained by the Center for Medicare and Medicaid Services (CMS).↩︎
Hospital expenses were obtained from the publicly-available Hospital Cost Report Information System (HCRIS) that contains data from the Hospital Cost Reports that hospitals are required to submit to the Centers for Medicare and Medicaid Services.↩︎
These statistics are calculated using data from the CMS Healthcare Cost Report Information System (HCRIS), op. cit.↩︎
The count is based on county population estimates for 2020 from the U.S. Department of Commerce, United States Census Bureau.↩︎
Driving distances and driving times between hospitals were calculated using the Google Maps Distance Matrix API.↩︎
Conversely, individuals who live in between the rural hospital and the alternative hospital may not have to travel much farther to reach the alternative hospital than they do to reach their current hospital.↩︎
Data on charges and costs were obtained from HCRIS. The total amount that each hospital charged for all services to all patients (regardless of whether or how much the hospital was actually paid for the services) was divided by the total cost of the services delivered. The median of this ratio was then calculated for all rural hospitals and the median was calculated for all urban hospitals.↩︎
The most up-to-date data on rural hospital closures are maintained by the Cecil G. Sheps Center for Health Service Research at the University of North Carolina. When the Sheps Center identifies a potential closure, it investigates to determine whether the hospital has actually closed, has reduced services, or has merged with or been acquired by a larger system, and it also monitors over time to identify whether a closed hospital later reopened. University of North Carolina, Cecil G. Sheps Center for Health Services Research.↩︎
The hospital is classified as “closed” because it stopped offering inpatient care, and therefore it can no longer be considered a hospital, even though community residents can still receive the same kinds of emergency and outpatient services they received in the past. In some cases, a different hospital or other entity took over operations of the emergency services and outpatient services when the inpatient services were terminated.↩︎
Driving distance and driving times between hospitals were calculated using the Google Maps Distance Matrix API.↩︎
Doctors Hospital at Deer Creek, a 10-bed hospital that was located in Leesville, Louisiana, closed in January 2019. It was located 0.3 miles from Byrd Regional Hospital, a 60-bed hospital which continues to operate. Leesville is a rural community near the Louisiana-Texas border which had an estimated population of 5,713 in 2018.↩︎
In some cases, outpatient services continue to be offered at the site of the closed hospital, although not a 24-hour ED.↩︎
Harmsen AMK et al. “The Influence of Prehospital Time on Trauma Patients Outcome: A Systematic Review.” Injury 46(4):602-609 (2015).
Nicholl J et al. “The Relationship Between Distance to Hospital and Patient Mortality in Emergencies: An Observational Study.” Emergency Medicine Journal 24:665-668 (2007).
Tansley G et al. “Effect of Predicted Travel Time to Trauma Care on Mortality in Major Trauma Patients in Nova Scotia.” Canadian Journal of Surgery 62(2): 123-130 (April 2019).↩︎Gujral K and Basu A. Impact of Rural and Urban Hospital Closures on Inpatient Mortality. National Bureau of Economic Research Working Paper 26182 (August 2019). Nationally, most hospital closures have occurred in urban areas, and some closures in rural communities have occurred where another hospital was nearby or where emergency services continued to be offered even though the hospital was “closed.” As a result, studies that do not differentiate between the circumstances surrounding hospital closures are less likely to show negative impacts on mortality rates or other outcomes. For example, a study that found no significant change in mortality rates following closures of either rural or urban hospitals did not control for differences in the travel time to the next-closest hospital or for whether emergency services continued to be offered at the site of the closed hospital. Moreover, its primary outcome measure was all-cause mortality for Medicare beneficiaries, not mortality for specific conditions that are sensitive to hospital travel time. Although it examined time-sensitive conditions, it only did so for closures overall, not for closures in rural areas. Joynt KE et al. “Hospital Closures Had No Measurable Impact on Local Hospitalization Rates or Mortality Rates,” Health Affairs 34(5): 765-772 (2015).↩︎
Shen Y and Hsia RY. “Association Between Emergency Department Closure and Treatment, Access, and Health Outcomes Among Patients With Acute Myocardial Infarction.” Circulation 134(20): 1595-1597 (2016).
Shen Y and Hsia RY. “Does Decreased Access to Emergency Departments Affect Patient Outcomes? Analysis of Acute Myocardial Infarction Population 1996-2005.” Health Services Research 47(1) Part I:188-210 (2012).
Hsia RY and Shen Y. “Emergency Department Closures and Openings: Spillover Effects on Patient Outcomes in Bystander Hospitals,” Health Affairs 38(9): 1496-1504 (2019).↩︎Carlson, AP et al. “Low Rate of Delayed Deterioration Requiring Surgical Treatment in Patients Transferred to a Tertiary Care Center for Mild Traumatic Brain Injury.” Neurosurgery Focus 29(5) (2010).
Fuentes B et al. “Futile Interhospital Transfer for Endovascular Treatment in Acute Ischemic Stroke.” Stroke 46:2156-2161 (2015).
Newgard, CD et al. “The Cost of Overtriage: More Than One-Third of Low-Risk Injured Patients Were Taken to Major Trauma Centers.” Health Affairs 32(9): 1591-1599 (2013).↩︎Maron DF. “Maternal Health Care is Disappearing in Rural America.” Scientific American, February 15, 2017.↩︎
Kozhimannil KB et al. “Association Between Loss of Hospital-Based Obstetric Services and Birth Outcomes in Rural Counties in the United States,” JAMA 319(12):1239-1247 (2018).↩︎
Massarweh NN et al. “Association Between Travel Distance and Metastatic Disease at Diagnosis Among Patients With Colon Cancer.” Journal of Clinical Oncology 32(9):942-948 (2014).↩︎
U.S. Department of Commerce, United States Census Bureau.↩︎
U.S. Department of Commerce, United States Census Bureau. 2018 Population Estimates.↩︎
Chereb S. “Tonopah Hospital Closes, Leaving Medical Care 100 Miles Away,” Las Vegas Review-Journal, August 21, 2015.↩︎
Johnson B. “Officials Seek to Revive Rural Tonopah Hospital,” Nevada Public Radio, November 22, 2019↩︎
Kyser H. “Four Years Later, Tonopah Recovering from Hospital Closure.” Nevada Public Radio, November 14, 2019.↩︎
King, M. “DeQueen Medical Center Closes Doors, Part of Larger Trend of Closings,” Arkansas Money & Politics, May 8, 2019.
Stromquist, K. “As De Queen’s Hospital Struggles, Workers, Residents on Edge,” Arkansas Democrat-Gazette, January 13, 2019.↩︎Artiga S, Rae M. The COVID-19 Outbreak and Food Production Workers: Who is at Risk? Kaiser Family Foundation, June 3, 2020↩︎
Centers for Disease Control, based on July 2, 2020 data.↩︎
Bachman M. “County Passes Ordinance to Sell Bonds, Fund Hospital Construction.” The DeQueen Bee, September 14, 2020.↩︎
Probst, JC et al. “Economic Impact of Hospital Closure on Small Rural Counties, 1984 to 1988: Demonstration of a Comparative Analysis Approach.” The Journal of Rural Health 15(4): 375-390 (Fall 1999).
Manlove JL and Whitacre BE. Short-Term Economic Impact of Rural Hospital Closures. Paper presented at the Southern Agricultural Economics Association’s 2017 Annual Meeting, February 4-7, 2017.
The impact depends on the nature of the closing; one study of rural hospital closures found significant reductions in per capita income and significant increases in unemployment in communities that lost their sole hospital but not in communities with alternative sources of hospital care. Holmes GM et al. “The Effect of Rural Hospital Closures on Community Economic Health.” Health Services Research 41(2): 467-485 (April 2006).↩︎U.S. Department of Agriculture, National Agricultural Statistics Service. 2017 Census of Agriculture.↩︎
U.S. Department of Commerce, Bureau of Economic Analysis. Gross Domestic Product by County, 2020.↩︎
U.S. Department of the Interior, National Park Service. Visitation Numbers.↩︎
Most of the top 10 National Parks are very large and have multiple entrances and attractions. For example, the main entrance to the Olympic National Park is in Port Angeles and is only 6 minutes from the Olympic Medical Center, but the Hoh Rain Forest Center on the southwestern side of the Park is nearly two hours from Port Angeles and 46 minutes away from Forks Community Hospital. (Travel times were calculated using the Google Maps Distance Matrix API.)↩︎
Artiga S, Rae M. The COVID-19 Outbreak and Food Production Workers: Who is at Risk? Kaiser Family Foundation, June 3, 2020.↩︎
U.S. Department of Agriculture, National Agricultural Statistics Service. 2017 Census of Agriculture.↩︎
Agriculture in Eastern Washington State is supported either directly by the Columbia River or by the Columbia Basin Project, which is the largest water reclamation project in the country. The Grand Coulee Dam, located in the middle of the region, provides water to the Columbia Basin Project through more than 1600 miles of canals, which in turn provide irrigation water to over 600,000 acres of land. The hydroelectric plants at the Grand Coulee Dam are the largest single power station in the United States. The region also contains the Channeled Scablands that were shaped by Ice Age floods.↩︎