Cost of Rural Hospital Services
Most spending at small rural hospitals is for delivery of six essential services: (1) the Emergency Department, (2) inpatient services, (3) the laboratory, (4) radiology, (5) drugs and medical supplies, and at most hospitals, (6) one or more Rural Health Clinics.
The cost of an Emergency Department visit is inherently higher at small rural hospitals than at larger hospitals. At least one physician needs to be available around the clock in order to respond to injuries and medical emergencies quickly and effectively, regardless of how many patients actually visit the ED. Since this “standby capacity” cost will not decrease even if fewer patients visit the ED, the average cost per ED visit will be higher in a smaller community.
The cost of inpatient care, laboratory tests, imaging studies, primary care visits, and most other essential services is also inherently higher at small rural hospitals. For almost every type of service the hospital delivers, there is a minimum level of staffing and equipment required to deliver the service. As a result, the average cost per service will be higher in a smaller community where fewer services are needed.
Use of fee-for-service payments increases the likelihood of financial losses at small rural hospitals. Under the fee-for-service payment systems used by most health plans, the hospital receives the same fee for delivering a service regardless of how many times the hospital delivers that service. When fewer services are delivered, fee-for-service revenues decrease, even though the costs at a small rural hospital will not decrease. As a result, a hospital will be financially penalized if it helps the residents of its community stay healthy and they need fewer services.
Eliminating inpatient care would harm both the hospitals and their communities rather than preventing closures. In most cases, the revenues generated by inpatient care at a small rural hospital exceed the direct costs of delivering that care, so the hospital would be worse off financially if it no longer received those revenues. Moreover, the smallest rural hospitals have many patients receiving inpatient rehabilitation and/or long-term nursing care in their inpatient beds in addition to individuals receiving acute inpatient care. Closure of the inpatient unit would deprive the residents in the community of all of these services, as well as limit the ability of the hospital to respond to a pandemic or other health emergency.
The Major Categories of Expenses in Small Rural Hospitals
Direct Service Costs vs. Overhead Costs
Most hospital expenses fall into two major categories:
- Direct Service Costs. These are the costs associated with personnel who provide the services individual patients receive, such as the nurses in the inpatient unit, the physicians and nurses in the emergency department, and the technicians in the laboratory, as well as the costs of the equipment and supplies these personnel use to deliver services to patients.
- Overhead Costs. These are the costs associated with personnel who do not provide services directly to or for patients, such as the hospital’s accounting and billing departments, the human resources department, medical records, information systems, and maintenance.This also includes the costs of building and maintaining the hospital’s facilities.
A third and much smaller category consists of the direct costs of non-patient service activities, such as a gift shop, parking lot, or housing for staff.
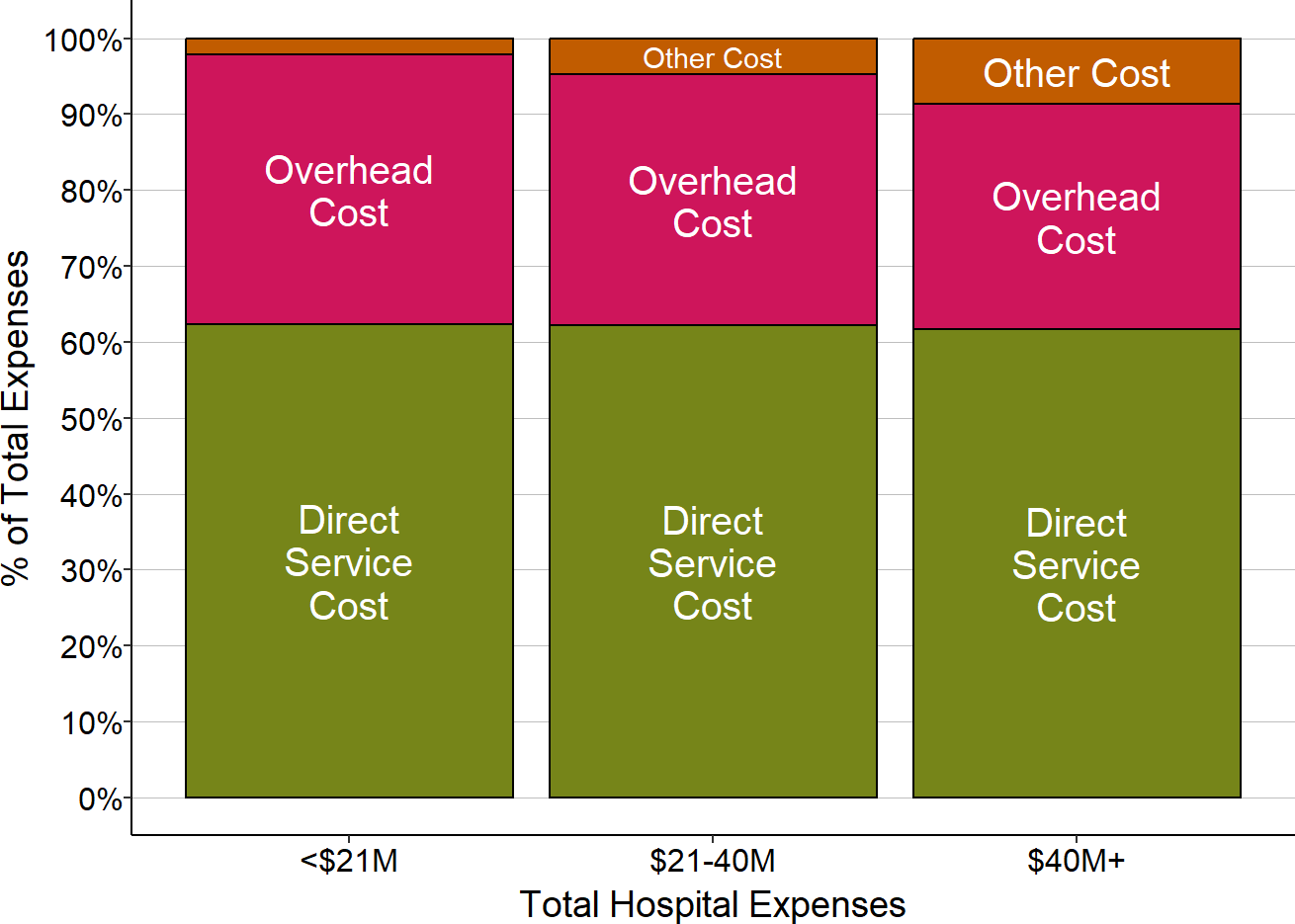
About 60% of the total expenses of small rural hospitals consists of direct service costs, and about 35% consists of overhead costs. Non-patient service activities represent less than 5% of total expenses at most hospitals.
Figure 1
Spending on Direct Services vs. Overhead Costs
in Small Rural Hospitals
Medians for most recent three years available. “Other” = costs associated with non-patient service activities.
The Largest Categories of Direct Service Costs
A core group of six services constitute the majority of direct patient service costs at small rural hospitals:
- the Emergency Department,
- inpatient services,
- the laboratory,
- radiology,
- drugs and medical supplies, and
- the Rural Health Clinic (if the hospital operates an RHC).
At small rural hospitals, these six core services represent over 60% of the hospital’s total direct patient service costs. Larger hospitals are more likely to offer other services, such as surgery and maternity care and to have larger numbers of patients receiving those services, so a smaller share of total costs at larger hospitals will be associated with the six core services, but the core services still represent more than half of direct patient service costs.
Figure 2
Direct Patient Service Costs in Rural Hospitals
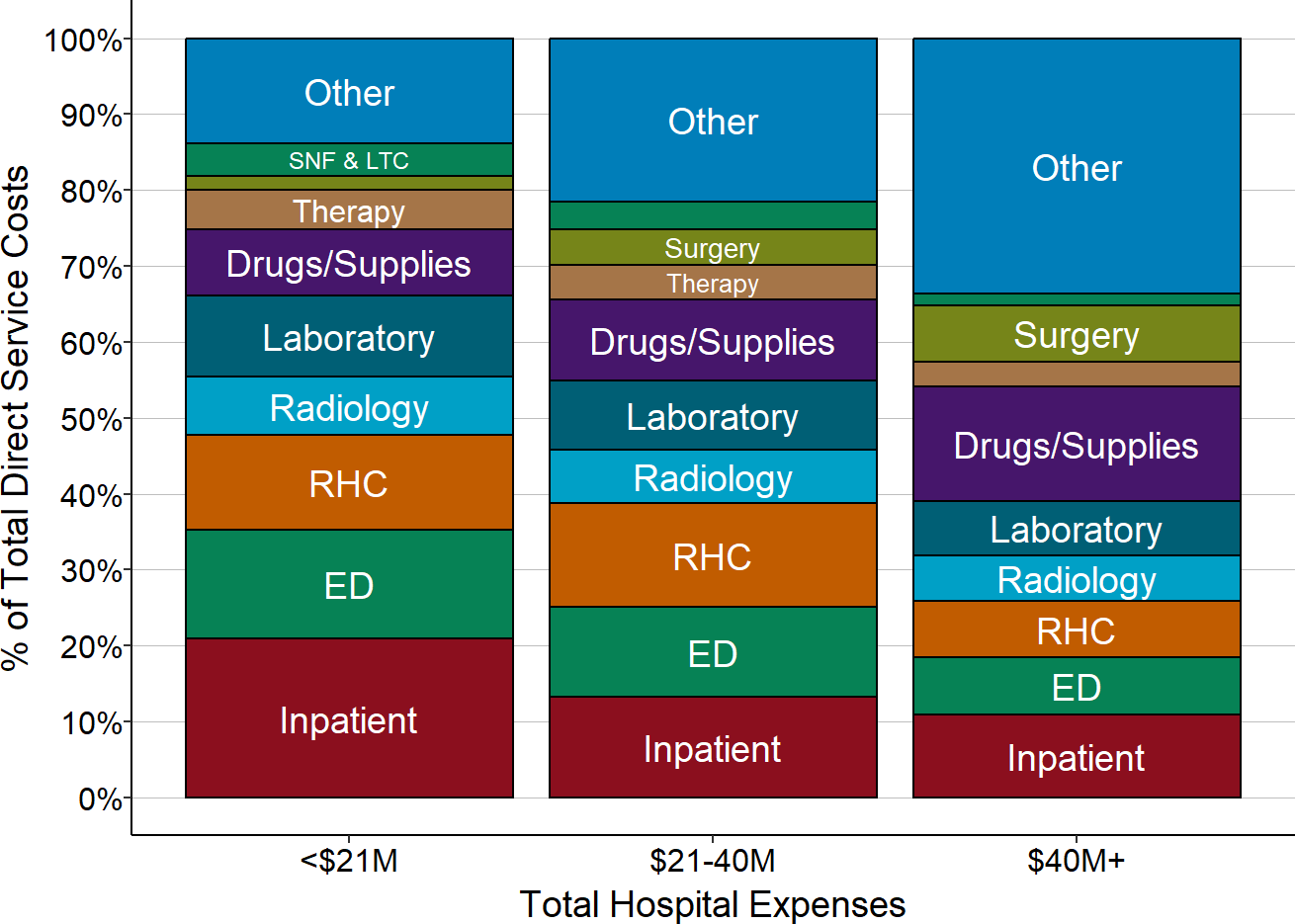
Medians for most recent three years available.
Categories of Overhead Costs
About half of overhead costs are for general administration of the hospital. This encompasses a broad range of activities, including accounting, human resources, billing, information systems, etc. Many small rural hospitals have had to spend large amounts of money to purchase and maintain an Electronic Health Record (EHR) system, and this contributes to the large share of costs in this category.
Not surprisingly, the second largest categories of costs are capital and maintenance costs, since it is expensive to build and maintain hospital facilities. On average, this represents nearly 30% of the total overhead costs at small hospitals.
The remaining 20% of overhead costs are associated with a variety of smaller functions, such as nursing management, medical records, housekeeping, dietary, and laundry services.
Since every hospital will need a minimum level of administrative services such as accounting, human resources, billing, etc. regardless of how many patients the hospital treats, one might expect that economies of scale would result in significantly lower administrative costs at the larger hospitals. However, the proportion of total expenses used for administrative costs is only slightly lower at larger hospitals.
Figure 3
Overhead Costs in Rural Hospitals
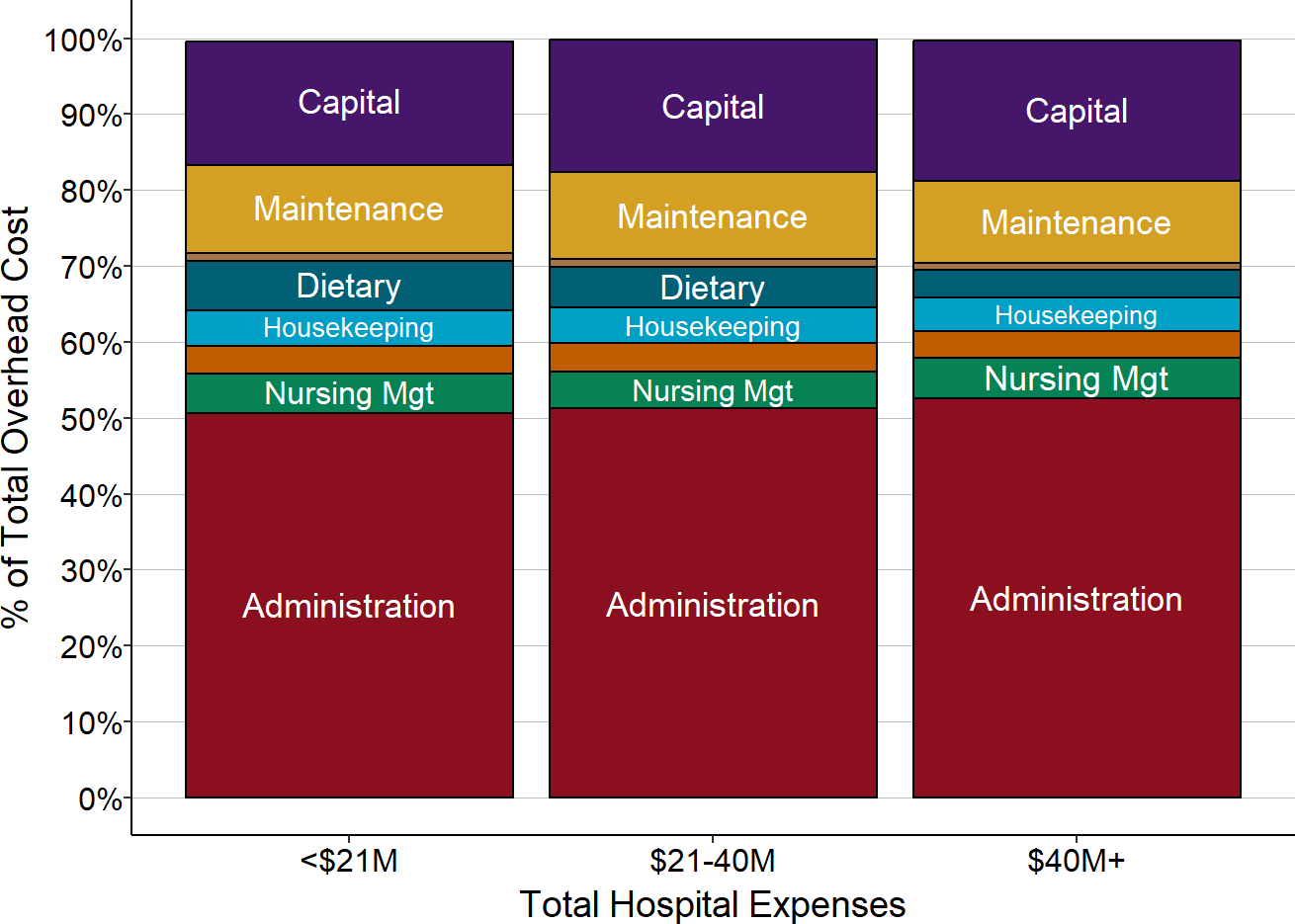
Medians for most recent three years available.
Total Service Line Costs
Hospitals are only paid for the services they provide to patients, so the payments the hospital receives for those services have to be adequate to cover not only the direct costs of the services, but also the overhead costs of the hospital. As a result, in order to set its charges for services, each hospital needs to allocate its overhead costs among the service lines.
The total cost of each service line will, on average, be about 60% higher than the direct costs when overhead costs are included. Since some services are more dependent on certain overhead cost centers than others, the percentages of overhead allocated to different service lines differ. For example, the inpatient unit is generally the largest user of the hospital’s dietary services, so a higher share of dietary costs is allocated to inpatient services.
Impact of Changes in the Number of Service Lines on Costs of Services
If a hospital is able to add an additional service line with little or no increase in administrative and overhead costs, the cost assigned to each of the existing service lines will decrease. This is because the hospital’s overhead costs are allocated across all of the hospital’s service lines, and so, all else being equal, the more service lines there are, the smaller the amount of overhead that will need to be allocated to each individual service line. As a result, the cost of a service line may differ at two hospitals not because of differences in the number of patients receiving the services, or differences in the staffing levels or wages paid to the staff, but because of how many other types of services each hospital offers.
An important corollary is that if a hospital eliminates a particular service line:
- the hospital’s total expenses will decrease by less than the total cost of the service line, because only a portion of the total cost allocated to the service line represents the direct costs of delivering that service; the rest represents a portion of the hospital’s general overhead expenses. While it may be possible for the hospital to make some reductions in one or more central administration cost centers when a service line is eliminated if the service line was a heavy user of those cost centers, in general, most of the hospital’s overhead costs will remain unchanged.
- The cost of every other service at the hospital will increase, because most of the overhead costs that had previously been allocated to the terminated service line now have to be recovered from the remaining service lines.
The Key Role of the Core Services on the Financial Viability of Small Rural Hospital
After allocation of overhead costs, the six core service categories still represent 60-70% of the total expenses at small rural hospitals. Because these services represent such a large proportion of the hospital’s total expenses, it will be difficult for a small hospital to be profitable if it does not receive payments for each of these core services that are adequate to cover the total (direct and overhead) costs of those service lines and if it cannot reduce the costs of the services to match the payments it is able to receive.
Figure 4
Total Service Line Costs in Rural Hospitals
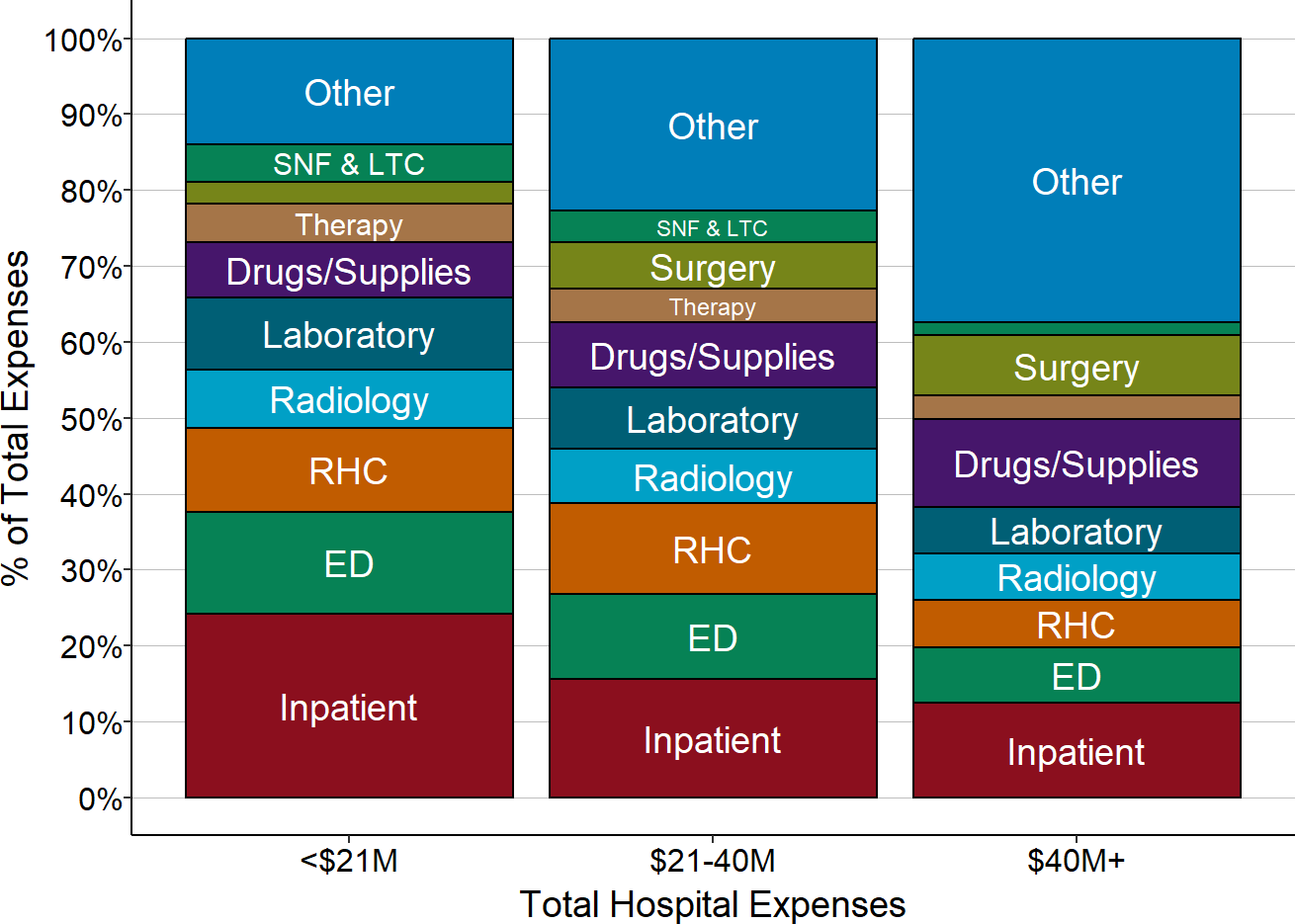
Medians for most recent three years available.
The following sections examine the factors affecting the costs of each of these core services in greater detail.
The Cost of Delivering Rural Emergency Department Services
The single most essential service that rural hospitals provide is a 24/7 Emergency Department. Although emergency departments at small rural hospitals do not have the capability to treat severe trauma cases and emergencies that require highly-specialized services, neither do many urban hospital EDs. The primary roles all EDs perform are to quickly and accurately diagnose health problems, provide any necessary treatment to the patients, and transfer the small set of patients who need specialized care to a trauma center, stroke center, etc. Residents of rural communities who do not have access to an Emergency Department may be more likely to die or experience complications that could have been prevented.
This section will examine the costs involved in operating Emergency Departments at small, rural hospitals. The focus in this section will be on the basic ED visit itself, not on any additional services a patient may receive during the visit that are delivered by other hospital departments, such as a laboratory test or an imaging study. The costs of delivering those other services will be examined separately below.
The Number of ED Visits at Small Rural Hospitals
It is reasonable to expect that the cost of an Emergency Department will depend on how many visits the ED has. Rural hospitals that have a small number of inpatient admissions seem less small when one counts ED visits. The majority of small rural hospitals had fewer than 5,000 ED visits in 2017, i.e., about one visit every 2 hours.1 However, there is also considerable variation in the volume of ED visits among these hospitals; 10% of small rural hospitals (i.e., hospitals with less than $30 million per year in total expenses) had more than 11,000 ED visits in 2017, while another 10% had fewer than 1,000 visits.
Figure 5
ED Visits in Small Rural Hospitals, 2017
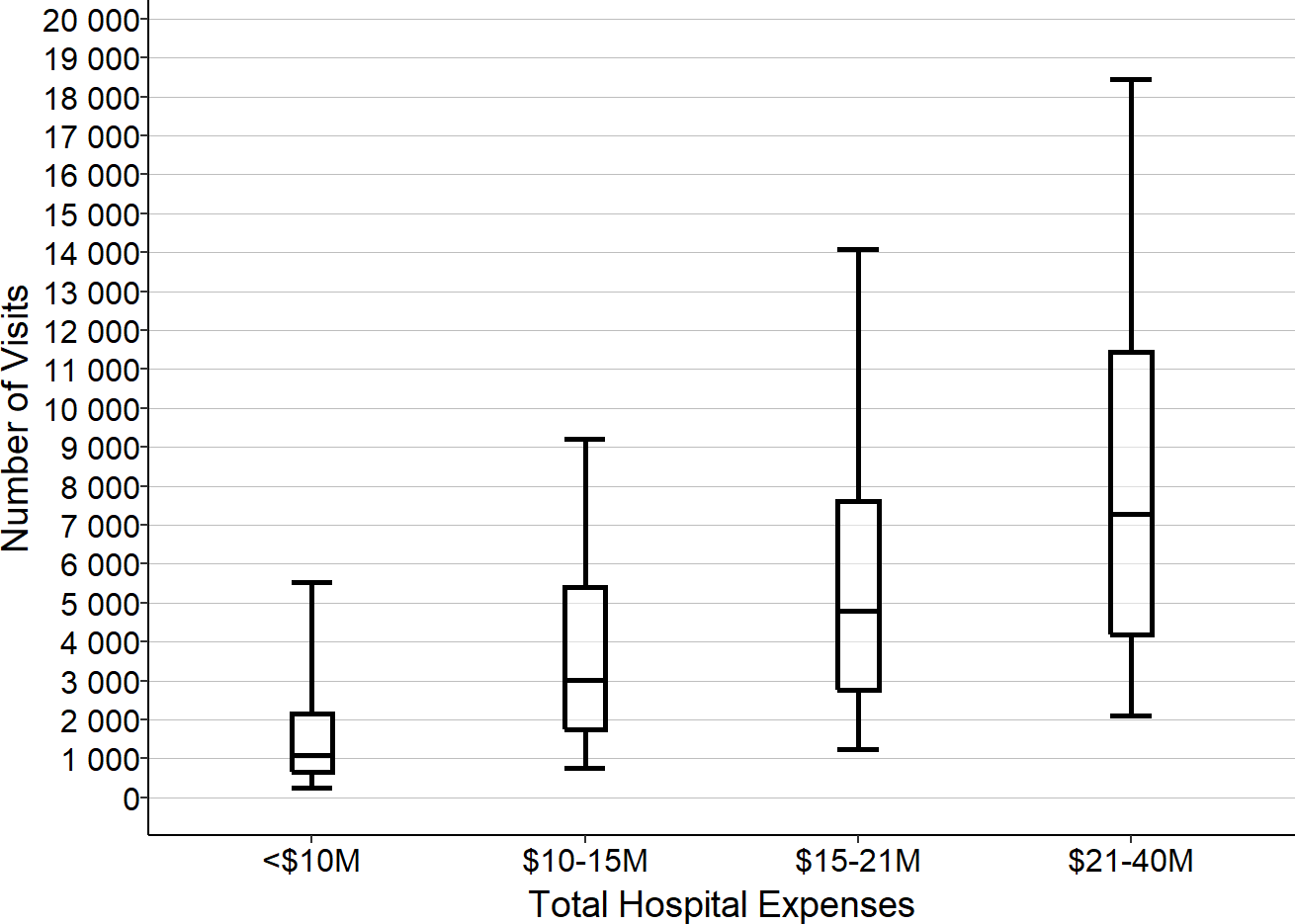
ED Visits are for 2017. Total Expense is for 2017 or for 2018 if 2017 is not available. Box shows 1st quartile, median, and 3rd quartile. Whiskers show 5th/95th percentile.
The large variation in the number of visits is due to a variety of factors, including the size of the community the hospital serves, the age and health status of the residents in the community, the number of businesses and workers in the community, the number of tourists who visit the community, and the community’s proximity to an interstate highway. Importantly, the number of ED visits will also depend on the availability of primary care in the community. For example, a hospital with no Rural Health Clinic will likely have more ED visits than a hospital that has an RHC because, without easy access to a primary care practice, more residents of the community will need to use the ED for non-emergency care.
The Cost of Operating an ED With 10,000 Visits Per Year
Each hospital’s cost report includes information on the total cost of operating its emergency department, but it is impossible to determine why some EDs are more expensive than others, even with the same number of visits, because there is very little information on the individual components of that cost. In particular, personnel costs would be expected to be the single largest component of the cost of an ED, but there is no information available on the number of physicians, nurses, or other staff who work in the ED, the number of hours they work, or the wage rates they are paid.2 However, since the ED needs to deliver high-quality care to patients who come with a wide range of problems at unpredictable times, one can estimate the level of staffing that a hospital would likely need in order to provide that care and how the staffing would change based on the volume of ED visits the ED receives.
Physician Staffing
An Emergency Department that has 10,000 visits per year will see an average of one new patient every hour. Although not every patient who comes to the ED will need to see a physician, the ED will need to have a physician available in case they do, so there will have to be at least one physician on duty at all times.3
The volume of visits will generally be higher at certain times of the day, days of the week, and months of the year. For example, hospitals in communities with a large number of seasonal businesses, such as those in agriculture and tourism, will have higher volumes of ED visits during some months than others. However, since productivity standards for Emergency Departments generally assume that an ED physician can manage 2-3 visits per hour, it will generally not be necessary for an ED with 10,000 visits per year to have any more than one physician on duty at a time except during exceptional circumstances.4
However, since the ED is a 24/7 operation, the hospital will have to employ or contract with at least 4 full-time equivalent (FTE) physicians in order to have one physician in the ED at all times.5 (The exact number of physicians will depend on the number of shifts each physician is willing and able to work each week, the amount of time the physicians need to spend in continuing education, vacation days, etc. Some rural hospitals have to hire or contract with multiple physicians, each of whom come to the community for a short period of time, in order to have one “full-time equivalent physician.”)6
A hypothetical hospital that employs 4 FTE physicians to staff its ED will need to spend about $1.2 million to do so if it pays the physicians a salary of $120/hour with benefits equivalent to 20% of the salary. However, the actual cost of employing emergency physicians can vary significantly from community to community and from year to year depending on a hospital’s ability to attract and retain physicians. If a physician retires or resigns, a hospital will often need to hire a temporary physician to fill in while a permanent replacement is found, and the hourly cost of the temporary physician will generally be significantly higher than the cost of a permanent employee. Many rural hospitals contract with national ED staffing companies in order to eliminate the burden of maintaining a full staffing complement and to make the cost of staffing the ED more predictable7, but this can increase the overall cost of the ED because the staffing company has to be paid more than the physicians themselves receive.
Nursing Staff
In addition to a physician, the ED will also need at least one Registered Nurse (RN) around the clock to help in triaging, treating, and discharging patients. Since a nurse will generally need to spend more time with each patient than the physician does, it is possible that one nurse will be insufficient if multiple patients come to the ED at the same time or if the patients have more serious conditions. Small rural hospitals will typically deal with multiple visits or more serious cases by having a nurse from the inpatient unit come to the ED to provide assistance. (The need for this backup coverage will affect the nurse staffing levels the hospital will need in the inpatient unit, as discussed in a later section.) If the higher volumes occur at predictable times, the hospital may need to have two nurses on those shifts.
In order to have at least one nurse in the ED at all times, a hospital will have to employ as many as 5 FTE RNs.8 If the hypothetical hospital pays RNs $38/hour and provides benefits equal to 20% of salary, the total cost for the year will be more than $400,000. Here again, though, the cost of employing nursing staff will vary across communities and over time based on the ability of individual hospitals to attract and retain nurses and how much it costs them to fill vacancies temporarily while permanent replacements are being recruited.
Other Staff
The hospital will likely also need at least one non-clinical staff member to check patients in, help family members, etc. so that the physician and nurses can focus on providing clinical services to the patients. In order to have such a staff member in the ED at all times, the hospital will need to employ 4-5 FTEs. Assuming a $16/hour wage and 20% benefits, this will cost the hypothetical hospital an additional $170,000 per year.
Other Direct Costs
Almost all of the direct costs of operating an Emergency Department are associated with the physicians, nurses, and other staff. The costs of any medications used and other supplies that are billed to a patient separately are ordinarily assigned to a separate hospital cost center (these costs will be discussed separately in a later section), so non-personnel direct costs for the ED itself will generally be relatively small.
Indirect Costs
Finally, the operation of the ED also depends on the hospital providing space and utilities, maintenance for equipment, housekeeping, billing for patient visits, payroll and benefits for staff, medical records, etc. Consequently, a portion of the hospital’s costs for those activities must be allocated to the ED to properly represent the total cost of operating the ED. Typically, these indirect costs increase the total cost of an ED by about 50% beyond the personnel and other direct costs discussed above.9
Total Cost
These five components together imply that it will likely cost the hypothetical hospital nearly $3 million to deliver services to 10,000 ED patients during the year.
Figure 6
Cost of Emergency Department
at a Hypothetical Small Rural Hospital
ED Visits: 10,000
|
|||
|---|---|---|---|
| Unit Cost | FTEs | Cost | |
| Physician | $120/hour | 4.0 | $994,000 |
| RN | $38/hour | 5.0 | $397,000 |
| Other Staff | $16/hour | 4.2 | $140,000 |
| Total Wages | $1,530,000 | ||
| Benefits | 20% of Wages | $306,000 | |
| Other Direct | $65,000 | ||
| Total Direct | $1,901,000 | ||
| Indirect Cost | 50% of Direct | $951,000 | |
| Total Cost | $2,852,000 | ||
The Cost of Operating an ED with More or Fewer Visits Per Year
How does the cost differ for an ED with more or fewer visits?
- For a hospital ED with 7,500 visits per year (i.e., 25% fewer than the 10,000 visits discussed above), there will still be almost one visit every hour, so this ED will also need one physician, one nurse, and a third staff member on duty round the clock. Other direct costs will be slightly lower with fewer patients and the indirect costs assigned to the ED may also be lower. Using the same assumptions about wage and benefit rates as for the hypothetical hospital discussed above, the total cost of the ED will be 96%-97% of the cost of the 10,000 visit ED, even though there are 25% fewer visits.
- Even if a hospital ED has only 5,000 visits per year, it will generally need to have a physician and nurse on duty around the clock, since it would have more than one visit every two hours on average. It is possible that the ED might be able to avoid using a third, non-clinical staff member during certain times of the day or week when the volume of visits is low, particularly if there is someone working in a different department at the hospital who can perform the same functions when needed, but this would only reduce the personnel costs by a relatively small amount. The total cost of an ED this size would likely still be more than 90% as much as the cost of the 7,500-visit ED, even though there are 33% fewer visits.
- If the ED has 12,500 visits per year (25% more than the 10,000 visits at the hypothetical hospital discussed earlier), it will have an average of 1.5 visits per hour, which can also generally be managed with a single physician on duty. However, because of the greater potential for delays during peak times, a hospital may choose to have an additional nurse on some shifts, which will increase the total number of nurses needed to staff the ED overall. As a result, direct costs and indirect costs may be 13% higher than at the ED with 10,000 visits.
- If the ED has 15,000 visits per year (50% more than the 10,000 visit ED), it will have an average of nearly 2 visits every hour. Because ED visits do not occur at a constant rate throughout the day and week, it is likely that the ED will have more than 3 visits per hour during its busiest times, which is more than a single physician can safely handle. Consequently, the hospital will likely need to hire additional physicians in order to have two physicians on duty during the high-volume shifts, in addition to a larger number of nurses. This would increase the cost of operating the ED by 45% over the cost at the 10,000 visit level, although this increase is still smaller than the 50% increase in visits.
Figure 7
Cost of Hypothetical Emergency Departments
with Different Numbers of Visits
| ED Visits | |||||
|---|---|---|---|---|---|
| ED Visits | 5,000 | 7,500 | 10,000 | 12,500 | 15,000 |
| Staffing (FTEs) | |||||
| Physician | 4.0 | 4.0 | 4.0 | 4.0 | 6.0 |
| RN | 5.0 | 5.0 | 5.0 | 7.5 | 7.5 |
| Other Staff | 2.0 | 4.2 | 4.2 | 4.2 | 4.2 |
| Cost | |||||
| Physician | $994,000 | $994,000 | $994,000 | $994,000 | $1,498,000 |
| RN | $397,000 | $397,000 | $397,000 | $593,000 | $593,000 |
| Other Staff | $67,000 | $140,000 | $140,000 | $140,000 | $140,000 |
| Total Wages | $1,457,000 | $1,530,000 | $1,530,000 | $1,726,000 | $2,230,000 |
| Benefits | $291,000 | $306,000 | $306,000 | $345,000 | $446,000 |
| Other Direct | $50,000 | $60,000 | $65,000 | $70,000 | $75,000 |
| Total Direct | $1,798,000 | $1,896,000 | $1,901,000 | $2,142,000 | $2,751,000 |
| Indirect Cost | $899,000 | $948,000 | $951,000 | $1,071,000 | $1,178,000 |
| Total Cost | $2,698,000 | $2,844,000 | $2,852,000 | $3,213,000 | $3,929,000 |
The Cost of Operating an ED with Even Fewer Visits
Most small rural hospitals have fewer than 5,000 ED visits per year. If the number of visits is less than about 10 per day (i.e., less than one visit every 2-3 hours), the hospital may be able to staff the ED differently, at least during some shifts. However, its ability to do so will depend on what other services the hospital offers, the availability of other physicians in the community and their willingness to help staff the ED, and the availability of remote support services from larger hospitals:
- If the hospital operates a Rural Health Clinic in or next to the facility where the ED is located, the physicians, nurse practitioners, or physician assistants who work in the clinic could leave the clinic and go to the ED to see a patient who comes to the ED during normal clinic hours.10
- At a hospital with a Rural Health Clinic(RHC), the RHC physicians/clinicians could also provide on-call coverage during night or weekend shifts when visit volumes are lower. If there are other primary care physicians in the community, they may also be willing to provide on-call coverage for the ED.
- A very low-volume ED could potentially use emergency-trained nurses to staff the ED if the hospital can arrange for telemedicine support from emergency physicians at a larger hospital.11
- If the nursing staff in the hospital’s inpatient unit is large enough (e.g., because the hospital has a large number of swing-bed patients), if the inpatient unit is close enough to the ED, and if the volume of ED visits is low enough, the hospital could rely on the inpatient unit nurses to staff the ED when a patient arrives, either during some shifts or all shifts, rather than having a nurse assigned exclusively to the ED.
The table below shows what the cost might be to operate a hypothetical ED that has 1,000 visits per year. This represents an average of fewer than 3 visits per day or less than one visit every 8 hours. The hospital where this ED is located is assumed to also operate a Rural Health Clinic staffed by both a physician and a Nurse Practitioner (NP), and the physician and the NP take responsibility for seeing patients who come to the ED during clinic hours. In addition, the Rural Health Clinic clinicians and one or more other physicians in the community are assumed to be willing to contract with the hospital to provide on-call support, i.e., they would agree to come to the ED quickly if and when a patient arrives. The example also assumes that there would be no dedicated nurses in the ED, and that one of the nurses from the hospital’s inpatient unit would go to the ED when a patient arrives. The total cost of this arrangement is just over $1 million. This is still about 40% of the cost of the ED with 10,000 visits, even though there are only one-tenth as many visits.
A hospital with 2,500 visits per year (about 6 visits per day) might still be able to rely on physicians at the Rural Health Clinic and in the community to diagnose and treat patients. However, it would be more problematic to rely solely on nurses from the inpatient unit to staff the ED, particularly during busier times, so it might need to employ additional nurses for this purpose. As shown in the table, the total cost might be about $1.6 million.
Figure 8
Cost of Hypothetical Emergency Departments with On-Call Staff
1,000 ED Visits
|
2,500 ED Visits
|
|||||
|---|---|---|---|---|---|---|
| Unit Cost | FTEs | Cost | Unit Cost | FTEs | Cost | |
| Clinicians | ||||||
| Physician (PT) | $130/hour | 0.2 | $43,000 | $130/hour | 0.5 | $122,000 |
| NP/PA (PT) | $60/hour | 0.1 | $10,000 | $60/hour | 0.2 | $19,000 |
| On Call | $60/hour | $496,000 | $60/hour | $451,000 | ||
| Nurses | ||||||
| RN | $38/hour | 2.0 | $158,000 | |||
| RN (Shared) | $38/hour | 0.5 | $38,000 | $38/hour | 0.8 | $57,000 |
| Other Personnel | ||||||
| Other Staff | $16/hour | 2.0 | $67,000 | |||
| Total Wages | $587,000 | $873,000 | ||||
| Benefits | 20% of Wages | $117,000 | 20% of Wages | $175,000 | ||
| Other Direct | $10,000 | $25,000 | ||||
| Total Direct | $714,000 | $1,072,000 | ||||
| Indirect Cost | 50% of Direct | $357,000 | 50% of Direct | $536,000 | ||
| Total Cost | $1,071,000 | $1,609,000 | ||||
Variation in Costs for EDs of Similar Size
The cost estimates for the hypothetical EDs described above are based on multiple assumptions about the availability and cost of staff in the ED and other costs in the hospital, some or all of which may not be realistic for hospitals in every community. As a result, the actual costs in individual hospitals will vary significantly from community to community; moreover, costs can change from year to year for reasons beyond the control of the hospital. For example:
- There may be no primary care physician in the community or no physician who is willing to provide on-call coverage for the ED, in which case the hospital would have to hire dedicated physicians for the ED.
- A hospital located in a more remote area may have greater difficulty attracting and retaining physicians to staff the ED, and may need to pay physicians more to work there.
- If a physician resigns or retires, the hospital will often need to engage a locum tenens physician until a replacement is found, and it will generally need to pay a much higher hourly rate for the temporary physician, for their travel costs, etc.
- A hospital with large seasonal differences in the numbers of ED visits may need to have higher staffing levels during a portion of the year that cannot be offset by smaller staffing levels during the remainder of the year.12
- A hospital that does not have easy access to a part-time nursing workforce may need to employ a larger complement of nurses in order to ensure it has adequate coverage for illnesses, vacations, training, etc.
- A hospital located in an area where health insurance is more expensive will incur higher benefit costs for its employees.
- A hospital that offers a broader array of services will need to assign a smaller portion of its administrative costs to the ED than a hospital with a more limited set of services. For example, if the hospital operates a Rural Health Clinic, a portion of the hospital’s general administrative costs will be allocated to the RHC in addition to the ED, reducing the cost assigned to the ED.
In some cases, favorable and unfavorable differences in different aspects of cost may offset each other, but it is more likely that hospitals experiencing higher costs in one component of costs will also have higher costs in other areas. The table below shows an example of how the total cost of two EDs with similar numbers of ED visits can differ dramatically due to the combined effects of multiple small differences in staffing levels, wage rates, benefit rates, and overhead allocations. Hospital A and Hospital B have the same number of ED visits and they each have one physician, one nurse, and one other staff member on duty at any given time. However, Hospital B needs slightly more physicians and nurses in order to achieve this level of staffing, it has to pay the employees more than Hospital A, and it has fewer service lines overall, so it has to allocate a higher share of administrative costs to the ED. The combined result is that Hospital B’s overall cost for the ED is 26% higher than the cost at Hospital A.
Figure 9
Impact of Variations in Unit Costs on Total Emergency Dept. Cost
Hospital A (5,000 ED Visits)
|
Hospital B (5,000 ED Visits)
|
Difference | |||||
|---|---|---|---|---|---|---|---|
| Unit Cost | FTEs | Cost | Unit Cost | FTEs | Cost | ||
| Physician | $115/hour | 4.0 | $952,000 | $125/hour | 4.5 | $1,170,000 | 23% |
| RN | $37/hour | 5.0 | $385,000 | $39/hour | 5.0 | $406,000 | 5% |
| Other Staff | $15/hour | 2.0 | $62,000 | $17/hour | 2.0 | $71,000 | 15% |
| Total Wages | $1,400,000 | $1,646,000 | 18% | ||||
| Benefits | 18% of Wages | $252,000 | 22% of Wages | $362,000 | 44% | ||
| Other Direct | $40,000 | $60,000 | 50% | ||||
| Total Direct | $1,692,000 | $2,069,000 | 22% | ||||
| Indirect Cost | 48% of Direct | $812,000 | 52% of Direct | $1,076,000 | 33% | ||
| Total Cost | $2,504,000 | $3,144,000 | 26% | ||||
Because the unit costs can vary for many reasons beyond the control of a small rural hospital, the staffing and compensation levels for the hypothetical hospital EDs shown in Figures 3-7 and 3-8 do not represent what any individual hospital ED should cost or what the differences in costs between EDs of different sizes should be. However, the cost models for the hypothetical hospitals do provide useful insights into what it can cost to operate small rural hospital EDs and the potential magnitude of differences based on size.
The amounts calculated above for the hypothetical EDs are very similar to the median actual costs of Emergency Departments at small rural hospitals, after adjusting the estimates downward to reflect several years of inflation since 2016-18.13 There is also significant variation in the actual amounts that small rural hospitals spend to operate Emergency Departments with similar numbers of visits, much of which is likely due to the kinds of factors described above.
Figure 10
ED Actual and Estimated Costs in Small Rural Hospitals
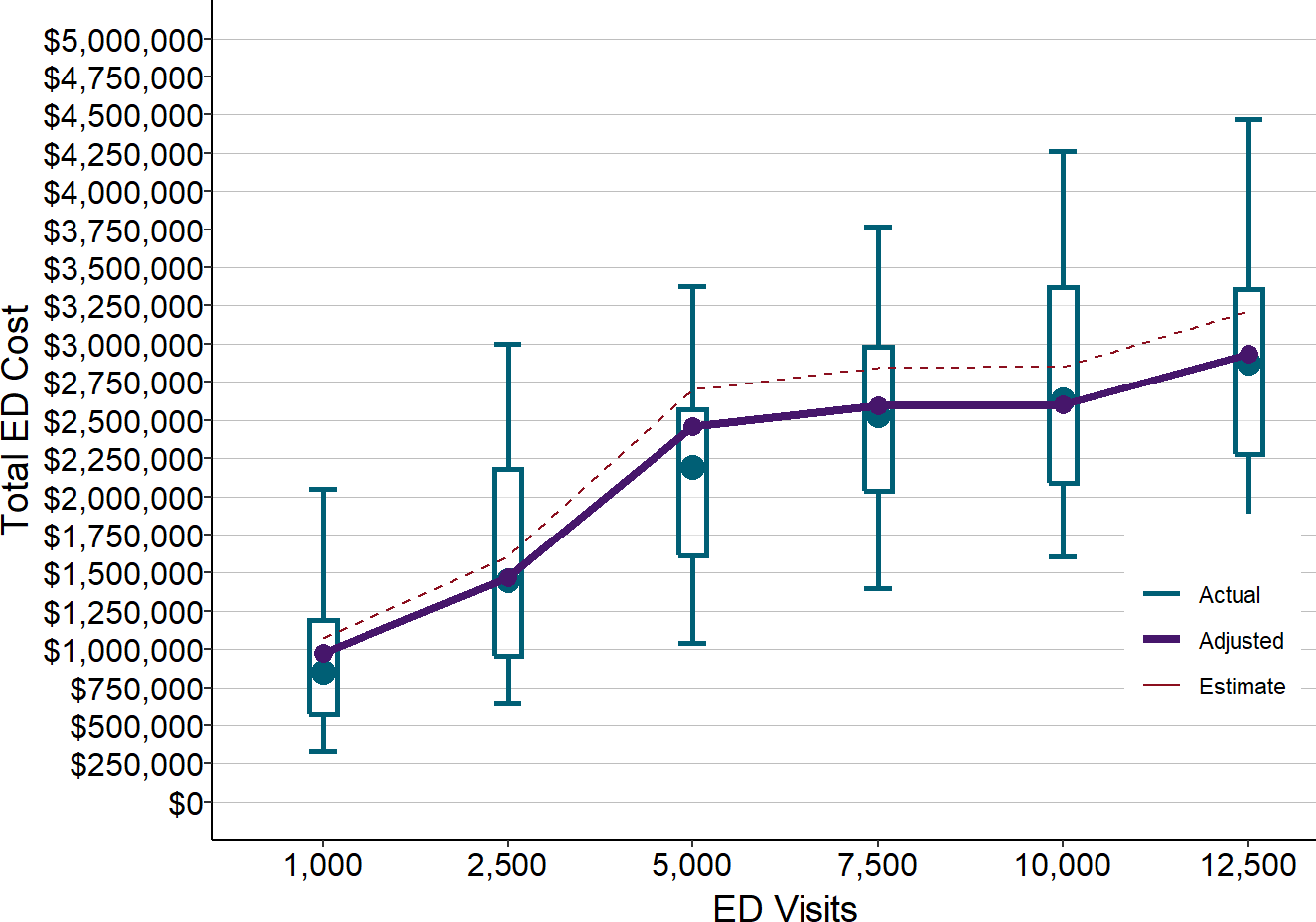
Actual amounts are for rural hospitals with less than $30 million in total expenses in 2016-18. Estimates (dotted line) are from Figure 7 and Figure 8. Adjusted values (solid line) are the estimated values reduced to reflect inflation between 2017 and 2020.
Differences in the Cost of an ED Visit at Different Hospitals
The total cost of operating an ED is generally not directly proportional to the number of ED visits because the same level of staffing is needed for a wide range in the number of visits. This means that the average cost per visit in the ED will be significantly lower at a hospital with more ED visits. While the estimated total cost of operating the hypothetical ED with 12,500 visits was 13% more than the cost of an ED with 7,500 visits, the cost per visit at the 12,500-visit ED is 32% lower because there are 67% more visits. The average cost per visit at the hypothetical ED with 1,000 visits is over $1,000, more than 4 times the average cost per visit at the hypothetical ED with 12,500 visits, because the total cost of the ED is 1/3 as much even though there are only 10% as many visits.
Figure 11
Cost Per Service at Different Service Volumes in Emergency Depts.
| ED Visits | |||||||
|---|---|---|---|---|---|---|---|
| ED Visits | 1,000 | 2,500 | 5,000 | 7,500 | 10,000 | 12,500 | 15,000 |
| Cost | |||||||
| Total Cost | $1,071,000 | $1,609,000 | $2,698,000 | $2,844,000 | $2,852,000 | $3,213,000 | $3,929,000 |
| Cost Per Service | |||||||
| Cost Per Visit | $1,071 | $643 | $540 | $379 | $285 | $257 | $262 |
However, once the number of visits reaches a certain level, the cost per visit begins to stabilize because more of the total cost represents the “semi-variable” cost of additional physicians and nurses needed to handle additional visits, rather than the fixed cost of the minimum capacity to handle even a small number of visits. For example, even though the total cost of the ED with 15,000 visits is 45% higher than the cost of the ED with 10,000 visits, the cost per visit is only slightly less.
As shown below, the actual cost per visit at rural hospitals follows this pattern. The median cost per ED visit at hospitals with small number of visits is double, triple, or even more than quadruple the median cost per visit at hospitals with larger number of visits.
There is much greater variation in the cost per visit among the smallest hospitals, which likely reflects the variety of challenges in staffing such EDs in different communities.14
Figure 12
Cost Per ED Visit in Small Rural Hospitals
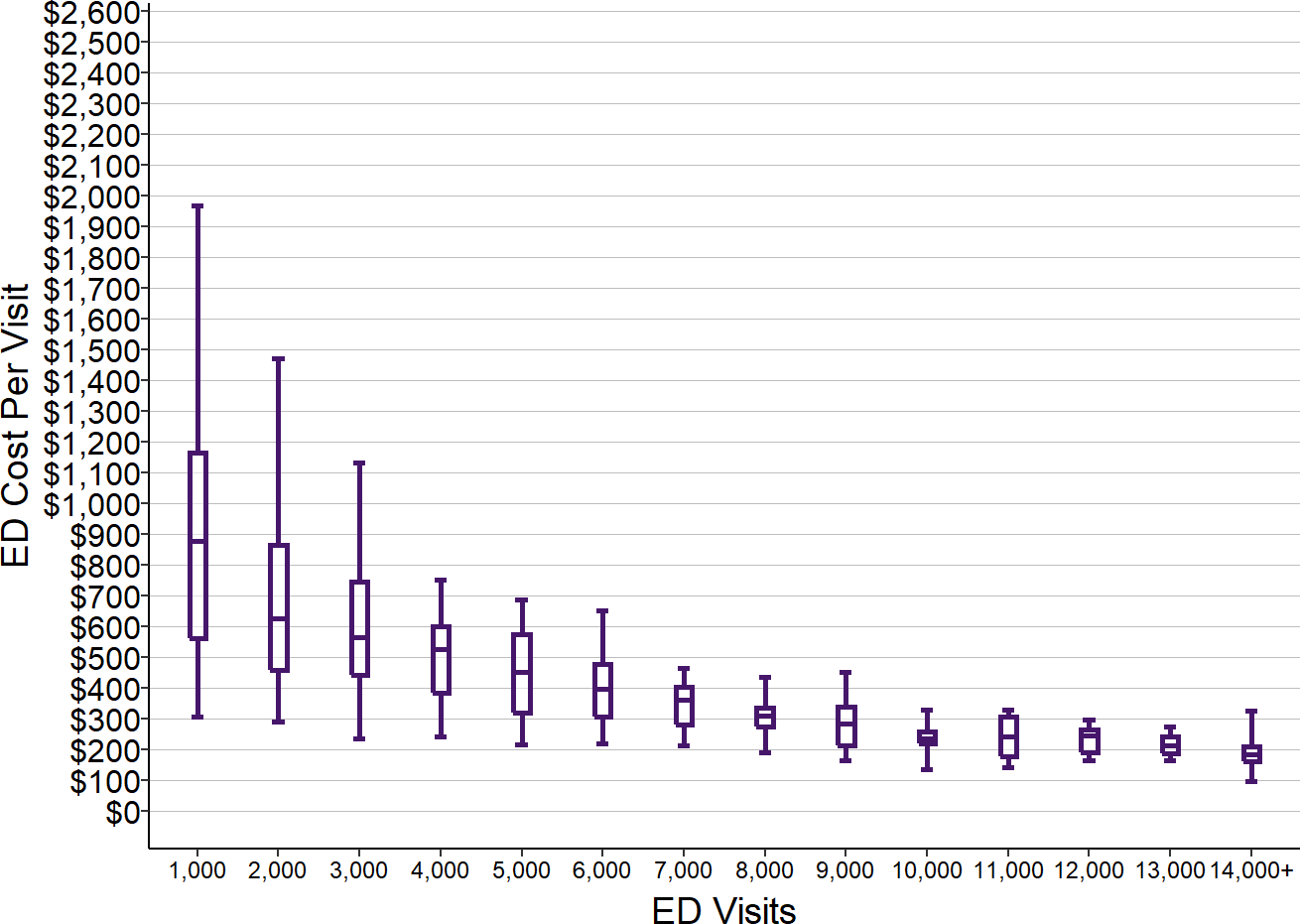
Values shown are for rural hospitals <$30M total expenses. ED Visits are from 2017. ED cost is the median for each hospital in 2016-18.
The cost models of the hypothetical EDs make it clear that the primary reason smaller hospitals have higher costs per visit than larger hospitals is not because the smaller hospitals are “inefficient” in delivering services, but because they have to incur a minimum level of fixed costs in order to operate an ED regardless of how many visits the ED actually receives. As a result, any effort to evaluate the relative efficiencies of hospitals based solely on differences in their average cost per ED visit will lead to erroneous conclusions.
Impact of Changes in Volume on the Cost Per Visit
Because the cost of operating an ED is not directly proportional to the number of visits, the average cost per visit at a hospital ED will vary from month to month and year to year based on the number of people who happen to visit the ED during that particular period of time.
For example, the table below shows a hypothetical hospital with 5,000 ED visits; the total estimated cost of operating the ED is $2.7 million, using the same assumptions about staffing and unit costs shown earlier. If the hospital has exactly 5,000 visits, its average cost per visit will be $540.
If the hospital happens to get only 4,500 visits during the year instead of 5,000, it will not be possible to reduce the staffing in the ED, so the cost of operating the ED will not change. However, dividing the same cost by 10% fewer visits causes the average cost per visit to increase by $59, a more than 11% increase.
Similarly, if the hospital ED happens to receive 5,500 visits during the year instead of 5,000, no additional physicians, nurses, and other staff will be needed, so the cost of operating the ED will not change. But with 10% more visits, the average cost per visit will decrease by $50, a reduction of more than 9%.
As a result, the average cost per visit at any hospital will vary from year to year, not because the hospital has become more or less efficient in delivering services, but simply due to the inherently random nature of the number of ED visits.
Figure 13
Changes in Cost Per Visit When Number of Visits Changes
Base Volume
|
Lower Volume
|
Higher Volume
|
|||
|---|---|---|---|---|---|
| Amount | Amount | Change | Amount | Change | |
| ED Visits | |||||
| ED Visits | 5,000 | 4,500 | −10% | 5,500 | 10% |
| Cost | |||||
| Physician | $994,000 | $994,000 | 0% | $994,000 | 0% |
| RN | $397,000 | $397,000 | 0% | $397,000 | 0% |
| Other Staff | $67,000 | $67,000 | 0% | $67,000 | 0% |
| Total Wages | $1,457,000 | $1,457,000 | 0% | $1,457,000 | 0% |
| Benefits | $291,000 | $291,000 | 0% | $291,000 | 0% |
| Other Direct | $50,000 | $50,000 | 0% | $50,000 | 0% |
| Total Direct | $1,798,000 | $1,798,000 | 0% | $1,798,000 | 0% |
| Indirect Cost | $899,000 | $899,000 | 0% | $899,000 | 0% |
| Total Cost | $2,698,000 | $2,698,000 | 0% | $2,698,000 | 0% |
| Cost Per Service | |||||
| Cost Per Visit | $540 | $599 | 11% | $490 | −9% |
The Problems Caused by Visit-Based Fees
Although the cost of operating a hospital ED is not directly proportional to the number of ED visits, the hospital’s revenue usually is. Most of the revenue hospitals use to cover ED costs comes from a fee paid each time a patient visits the ED. As a result, when the number of visits increases, revenue increases proportionally, and when the number of visits decreases, so does revenue.15 (Separate fees are paid for the other services the patients receive, such as lab tests or x-rays, and those will be discussed in a later section in conjunction with the costs of those services.)
This approach to payment causes two serious problems for small rural hospital EDs:
- Fees that are adequate for larger hospitals will not be adequate for smaller hospitals; and
- The adequacy of a visit fee depends on how many patients make ED visits.
Fees for ED visits that are adequate for larger hospitals will cause losses at small rural hospitals.
Figure 12 showed that for EDs with 7,000 visits, the median cost per visit was $400, with much higher costs per visit at smaller EDs. But as shown in Section 2, the median payments by private health plans for ED visits at small rural hospitals ranged from under $200 to $350 in the states examined. If the payment per visit is $200 - $350 when the cost per visit is $500 - $700 or more, the hospital will be unable to cover more than half of the cost of operating the Emergency Department.
As shown below, if every hospital in Figure 12 was paid $350 per ED visit16, the hospitals with 8,000 or more visits would have made a profit on every visit, whereas almost every hospital with less than 4,000 visits would have lost money on every visit. Most of the hospitals with the largest numbers of visits could have covered their costs or made a small profit even with a payment of $250 per visit, but a payment that low would have increased the size of the losses at the smallest hospitals and caused additional small hospitals to have losses.
Figure 14
Profit/Loss Per ED Visit with $350 Per Visit Fee
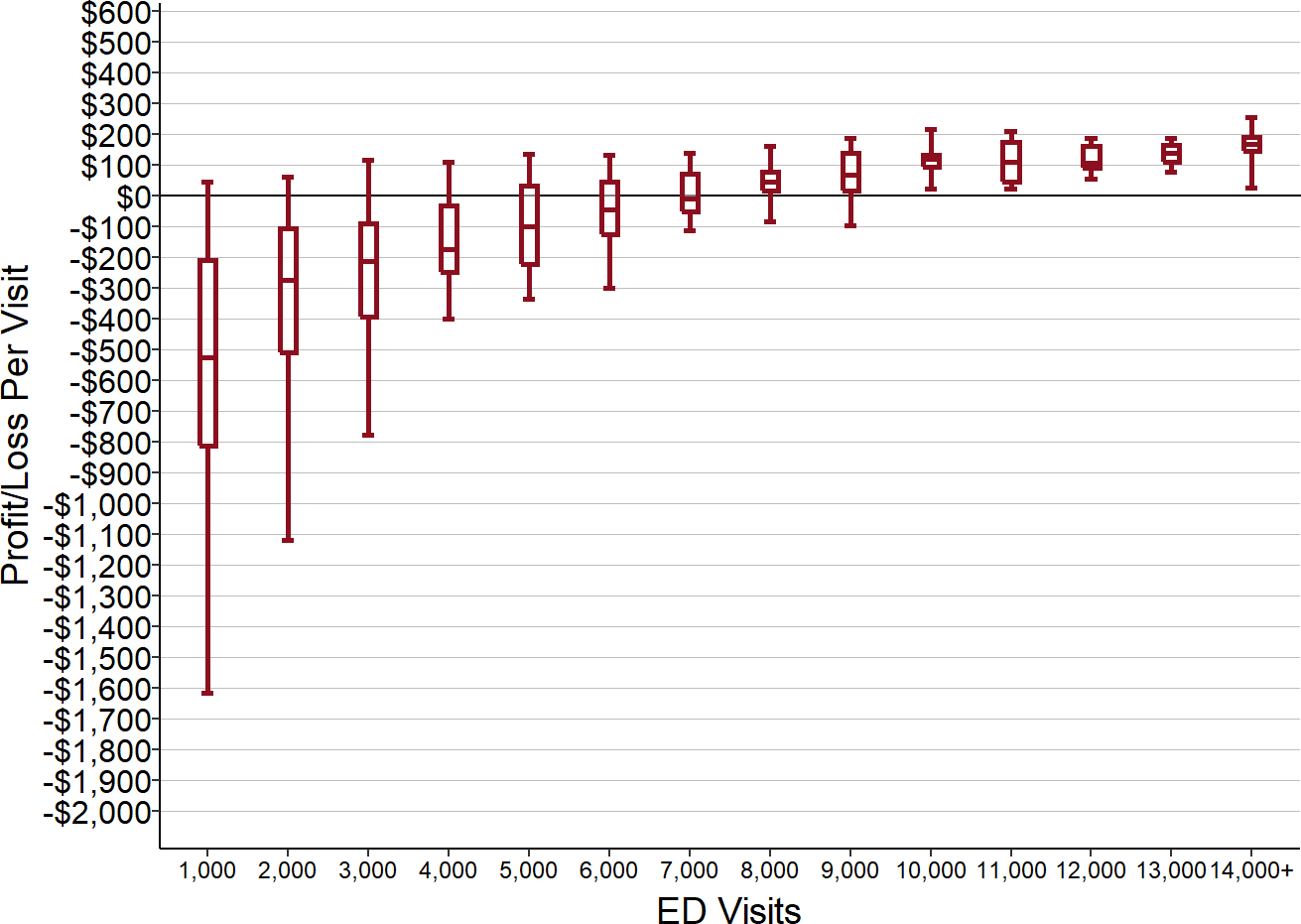
Values shown are the ED cost per visits amounts from Figure 12 subtracted from $350.
Some small hospitals will have larger losses than others, even if they receive the same payment per visit and have the same number of visits, if they have to pay more to attract and retain an adequate number of physicians and nurses in the community where they are located. In the example shown in Figure 9, even though Hospital A and Hospital B have the same number of ED visits and the same level of staffing in the ED on any given day, Hospital B would lose far more than Hospital A if they were both paid the same amount for a visit.
An unexpected illness or resignation of physicians or nurses will generally require the hospital to hire temporary physicians or nurses. This is far more likely at a small rural hospital because the smaller staff provides less capacity to cover temporary vacancies and because it takes longer to fill vacancies. Moreover, the higher cost of a temporary employee combined with the cost required to recruit a new employee will cause a larger percentage increase in personnel costs at a hospital that has a small number of employees to begin with. As a result, a visit fee that appeared to be adequate at the beginning of the year may no longer cover costs, and the hospital would experience losses by the end of the year.
The adequacy of any visit fee amount depends on how many patients actually have emergencies.
The problem with ED visit fees is not just the amount of payment, but the method of payment. Because revenues change in direct proportion to the number of visits when visits increase or decrease but costs may barely change at all, even small changes in the number of ED visits can result in larger or smaller losses or profits.
The table below shows that for the hypothetical hospital shown previously, if the ED receives 5,000 visits, a payment of $540 per visit would be just enough to cover the costs of the ED. However, if the fee is set at that level and the hospital only receives 4,500 visits (10% fewer than expected), the reduction in revenue would result in an 10% loss. Conversely, if the hospital happened to experience a 10% increase in the number of ED visits, it would receive a windfall profit of 10%.
It is impossible to predict exactly how many ED visits any hospital will have, so even if the visit fee appears adequate at the beginning of the year, it may well turn out to be inadequate by the time the year ends.
Figure 15
Impact on ED Margin When Number of Visits Changes
Baseline
|
Fewer Visits
|
More Visits
|
|||
|---|---|---|---|---|---|
| Amount | Amount | Change | Amount | Change | |
| ED Visits | 5,000 | 4,500 | −10% | 5,500 | 10% |
| Payment Per Visit | $540 | $540 | 0% | $540 | 0% |
| Total Revenue | $2,700,000 | $2,430,000 | −10% | $2,970,000 | 10% |
| Total Cost | $2,698,000 | $2,698,000 | 0% | $2,698,000 | 0% |
| Margin | $2,000 | ($268,000) | −13,500% | $272,000 | 13,500% |
| Pct Margin | 0% | −10% | −11,083% | 10% | 11,083% |
Tradeoffs Between Quality, Affordability, and the Financial Viability of Services
The problems with current payments mean that many small rural hospitals face problematic choices between delivering the highest-quality care at an affordable cost and avoiding financial losses.
Financial Penalties for Using Full-Time Emergency Physicians vs. Part-Time Providers
A patient experiencing an emergency will receive much faster care if there is a physician present in the ED at all times than if a physician has to be called in to the ED from home. Moreover, an emergency physician will have more training and experience in handling a wide range of emergencies than most primary care physicians. Consequently, it is preferable for the hospital to have emergency physicians on duty around the clock than to rely on on-call coverage from primary care providers.
However, the cost will likely be much higher to employ full-time emergency physicians than to rely on on-call providers, and it will often be more difficult and expensive to attract and retain full-time emergency physicians to work in an ED where they will only spend a fraction of their time actually treating patients. The increase in the median cost per visit between 3,000 and 4,000 visits that can be seen in Figure 12 is probably at least partially due to the fact that some hospitals with 3,000 visits have the ability to use part-time providers who are not emergency physicians to staff their ED, whereas hospitals with more visits will need to use full-time physicians, and it is much more expensive to do the latter than the former.
Because of the higher cost, a hospital will have to charge more per visit in order to employ full-time emergency physicians instead of using only part-time providers, and this will cause higher financial burdens on patients and increase the hospital’s bad debt. If patients’ health insurance plans refuse to pay the higher charges, the hospital will lose money.
Financial Penalties for Improving Care Management and Preventive Care
Many patients come to an ED for treatment of a problem that could have been prevented through better management of a chronic disease or better preventive care. For example, patients with asthma or COPD may experience exacerbations and breathing problems if they fail to take the appropriate medications, and individuals are more likely to get sick if they are not properly vaccinated for influenza or pneumonia.
However, the hospital is paid when the patient comes to the ED and it is not paid if the patient has no problems, so the hospital is penalized financially if the residents of the community are healthier. If primary care practices in the community or the hospital’s own Rural Health Clinic provide better care management and preventive care for their patients, the hospital ED could lose revenues as a result.
Financial Penalties for Charging Affordable Prices
As shown below, the median charge for an ED visit is generally between $600 - $900 at both smaller and larger rural hospitals. Based on the cost per visit data in Figure 12, if the hospitals were actually paid that amount, it would be more than adequate to cover the costs of an ED visit at all but the very smallest hospitals. However, that charge would be unnecessarily high at hospitals with larger numbers of visits.
Figure 16
Estimated Charge Per ED Visit at Small Rural Hospitals
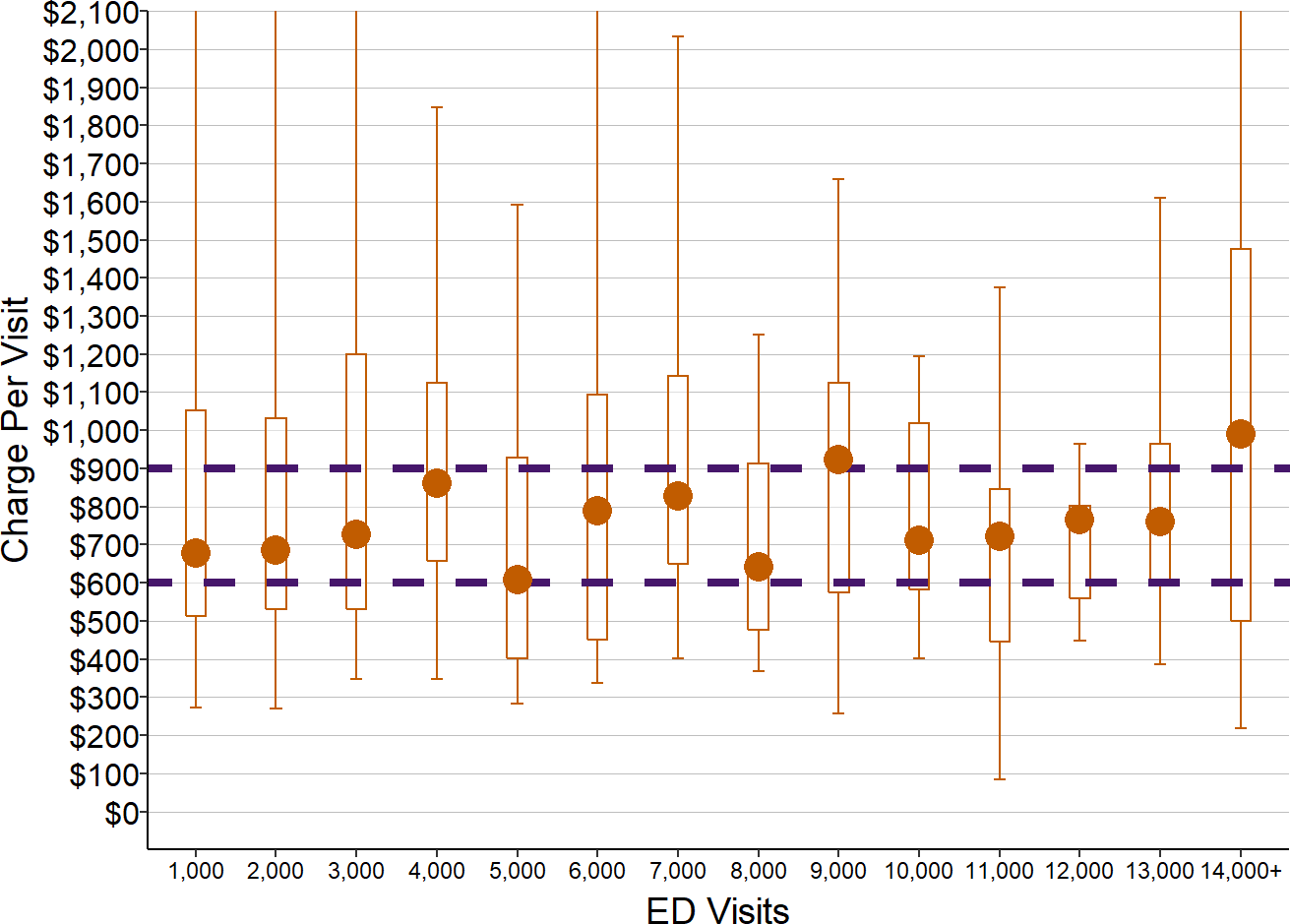
Amounts shown are estimated using median charges for 2016-18 and ED visits in 2017 for rural hospitals with less than $30 million in total expenses.
However, the chart also shows that the charges for ED visits vary dramatically among hospitals. Most health insurance plans demand that hospitals, physicians, and other healthcare providers provide large discounts on their standard prices in order to contract with the health plan. In order to give a discount, a hospital has to charge far more for a service than the cost of delivering the service so that the actual amount of payment the hospital receives for the service is sufficient to cover the cost. Typical commercial contract discounts are 50%, 67%, 75% or an even higher percentage of the charge, so the hospital has to set the charge at 2, 3, 4, or more times what the service actually costs.
However, these high charges make the hospital’s services unaffordable for patients who do not have insurance, and this can discourage patients from getting care that they need. If patients receive services but cannot afford to pay what the hospital charges, the hospital will have large amounts of patient bad debt and the patients could face bankruptcy.
If the hospital charges lower amounts for its services that patients could afford to pay, the discounts demanded by health insurance companies could result in “allowed amounts” that are lower than the hospital’s cost of delivering services. Since there are far more patients with insurance than without, there is a strong financial incentive for the hospital to set charges as high as possible. Since the cost per visit is higher at the smaller hospitals, the charges have to be even higher there, making care even less affordable for patients without insurance.
The Cost of Inpatient Care in Small Rural Hospitals
An emergency department alone is not enough to qualify a facility as a “hospital;” the facility must also offer inpatient care.17 This section will examine the costs involved in delivering inpatient care in small, rural hospitals. The focus here will be solely on the general nursing care and “bed and board” services a patient receives during an inpatient stay, not laboratory tests, imaging studies, therapy, surgery, or other services that may be delivered by other hospital departments during their stay. The costs of delivering those other services will be examined in the next section of this chapter.
As with the ED, hospital cost reports include information on the total cost of operating the inpatient unit, but it is impossible to determine why some units are more expensive than others because there is very little information on the individual components of that cost. It is possible to estimate the level of staffing that a hospital would likely need to provide high-quality inpatient care, but this will depend not only on the number of patients who receive inpatient care, but how sick they are and what kinds of services they will need.
The Different Types of Inpatient Care at Small Rural Hospitals
Acute Inpatients
Small rural hospitals have been experiencing the greatest financial challenges. 95% of rural hospitals with less than $45 million in total expenses have fewer than 10 acute inpatients per day, and the majority have fewer than 3 acute inpatients per day on average.
Three patients may seem like a very small number, but in order to have an average of 3 acute patients in the hospital each day, a hospital will generally have to admit over 400 patients during the course of a year. A hospital that has an average of 10 patients receiving acute inpatient care every day will have more than 1,000 admissions per year.
Moreover, annual averages can mask enormous variations from month to month and day to day. Although there are no national data available on the daily numbers of admissions to hospitals, individual small rural hospitals report that the monthly acute inpatient census can vary from 50% to 200% of the annual average. For example, a hospital with an annual average daily acute census of 2 may have an average of 4 patients in the hospital each day during some months, and an average of only 1 patient per day in other months.
Swing Bed Patients
However, small rural hospitals do not use their inpatient beds solely for patients with an acute illness. At almost all small rural hospitals, some or all of the inpatient beds are classified as “swing beds.” A swing bed can be used either for an acute patient (i.e., a patient who is sick enough to require admission to a hospital for treatment or observation), or for a non-acute patient who needs daily skilled nursing care. Swing beds allow rural hospitals to provide two types of services:
- Post-Acute Rehabilitation Services. Many patients cannot return home immediately after discharge from a hospital and need a period of rehabilitation that may last several days or several weeks. Some of the patients receiving post-acute care in rural hospital swing beds are the same individuals who just completed an inpatient stay at the same hospital, but many are patients who received surgery or medical treatment at a hospital in a larger community and then return to the rural hospital to receive rehabilitation care closer to home.
- Long-Term Nursing Care. Three-fourths of small rural hospitals also have long-term nursing patients in their swing beds. These are patients who have medical conditions or physical limitations that require a level of nursing care and personal care that they cannot receive at home.
In larger communities, these types of services are generally provided by Skilled Nursing Facilities (SNFs), but many rural communities are too small to support a separate SNF, particularly in states with low Medicaid payments for long-term nursing care, and the only way residents of the community can receive these services locally is if the hospital provides them through swing beds.
A Rural Hospital’s Total Inpatient Census is Larger Than Its Acute Census
Because a rural hospital’s inpatient unit(s) have both acute patients and swing bed patients, the total inpatient census in the hospital will generally be larger than its acute census, and often significantly larger. The total number of inpatients in the smallest hospitals is 2-3 times as large as what the acute census would suggest.
Figure 17
Average Daily Acute Census
and Total Inpatient Census
in Rural Hospitals
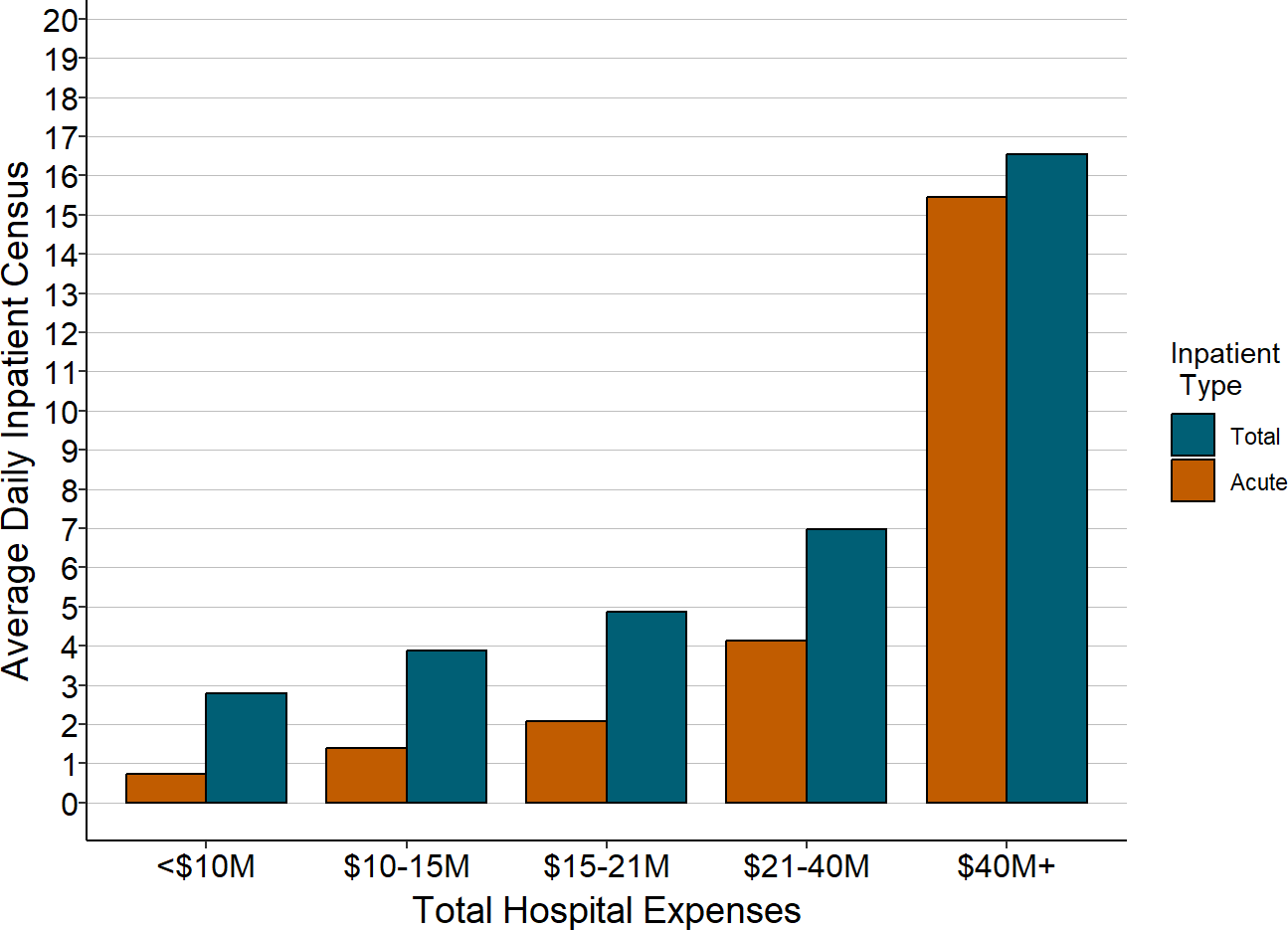
Average daily census and total expense is the median for the most recent three years available, excluding 2020. Acute includes both acute inpatient and observation stays. Total includes acute and swing bed patients.
Most rural hospitals use swing beds primarily for post-acute rehabilitation services, and they have at most one or two long-term nursing patients on any given day. Rural hospitals are not restricted to providing rehabilitation services to patients from the local community, so some hospitals with very small numbers of acute patients will have patients from a broader geographic area in their swing beds. The majority of hospitals with an average of less than 1 acute inpatient per day have a much higher total census due to patients in swing beds who are receiving short-term rehabilitation.
In a subset of hospitals, primarily those located in small isolated communities, the majority of patients in the hospital’s inpatient beds are long-term nursing care patients. 5% of small rural hospitals have an average of more than 6 long-term nursing care patients in their inpatient swing bed unit, and 2% have more than 15. In fact, some of the rural hospitals with the smallest number of acute inpatients have more total patients in their inpatient unit on any given day than many larger hospitals do because of the large number of nursing care patients in their swing beds. Among hospitals with less than 1 acute patient per day on average, the largest 10% of the hospitals have an average of more than 16 patients in total in their inpatient units, and the majority of those patients are receiving long-term nursing care.
Figure 18
Types of Inpatients in Rural Hospitals
With Very Small Acute Census
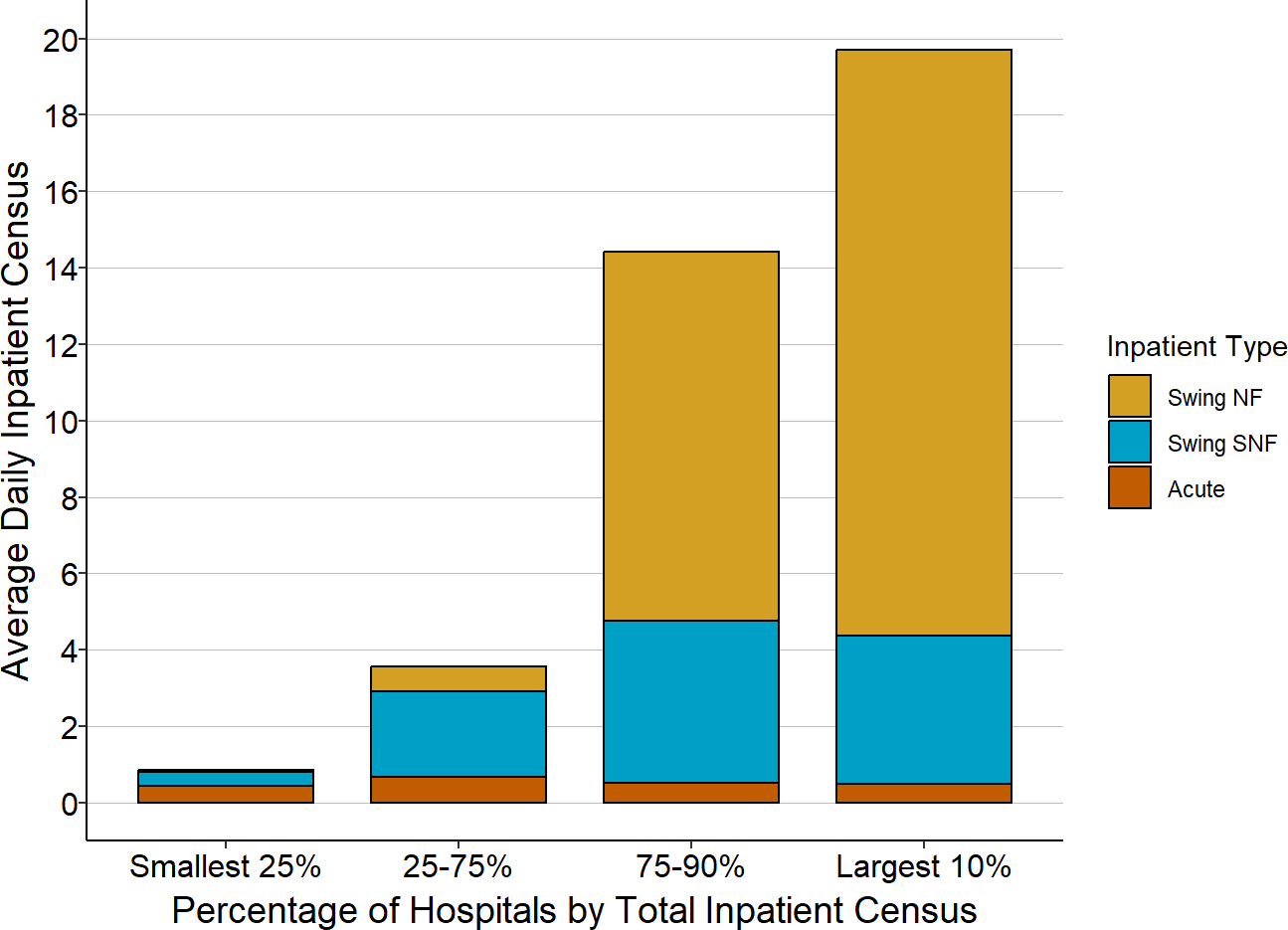
“Swing NF” is patients receiving long-term nursing care in hospital swing beds. “Swing SNF” is patients receiving short-term nursing care and rehabilitation in swing beds. Numbers shown are only for rural hospitals with an average of less than one acute inpatient or observation patient per day in the most recent three years available (excluding 2020).
The Cost of Delivering Inpatient Care in Small Rural Hospitals
Most patients who are admitted to small rural hospitals are there for treatment of a common acute medical condition (e.g., pneumonia or cellulitis) or an exacerbation of a chronic disease (such as COPD or heart failure), not for treatment of complex conditions or to receive invasive procedures. (Even if a small rural hospital delivers babies or performs orthopedic procedures, maternity care and surgical cases will generally represent a small fraction of the total acute inpatients.) The patients who are admitted may be too sick to safely return home immediately after they are diagnosed and treated in the emergency department, or they may need a type of treatment that they cannot receive at home, such as intravenous fluids or antibiotics. It is a significant advantage for a patient to be able to receive that kind of care in their own community rather than having to be transported to a hospital in a distant community, but this is only feasible if the hospital can financially sustain an inpatient.
The Cost of Delivering Inpatient Care to a Small Number of Acute Patients
The very smallest hospitals (those with total annual expenses under $10 million) have a median total daily census of 3 in their inpatient unit; the majority of these patients will generally be acute inpatients, with the rest receiving SNF-level rehabilitative care or possibly long-term care in swing beds.
In order to staff such a unit safely, the hospital will likely want to have two nurses on duty during each 12-hour shift. This might seem like a very high nurse:patient ratio to those familiar with staffing patterns for medical inpatient units, where the staffing ratios would be more like 1 nurse for every 5-7 patients. However, there are several reasons why the staffing ratio has to be higher in a small rural hospital:
- Variability in Patient Census. The fact that the average census is 3 does not mean that the census is 3 every day. The daily census can vary significantly because of the inherently random nature of when patients get sick and need to be admitted to the hospital, so on any given day, the number of patients receiving inpatient care could be twice as high or more. One analysis estimated that a hospital with an average daily census of 5 or less would need to staff for twice as many patients in order to have even a 95% assurance of adequate staffing during peak times.18
- Variability in Nursing Time Per Patient. Even if there are only two acute patients on the unit during the day, both patients could need hands-on nursing care at the exact same time, making it unsafe to have only one nurse available. Similarly, if a nurse on duty were to be injured or become ill, it would be unsafe if there were no backup nurse available. In a larger hospital, a nurse from another inpatient unit could be called on to help in such a situation, but in a small rural hospital, there is no “other unit.” In fact, because the nurses on the inpatient unit may be the only nurses in the hospital, they may be called on to help with peak demand in the ED or if someone experiences a medical problem while visiting another outpatient department, and so two nurses will be needed in order to provide that capacity.
- Multiple Nursing Tasks Per Patient. In contrast to a larger hospital, there is no separate set of nurses responsible for admitting or discharging patients; the nurses on the inpatient unit will need to perform these tasks as well as direct patient care. Because the average length of stay is only 2-3 days and some patients will only be in the hospital for a day, there will likely be 1-2 admissions or discharges every day19 and it would be impossible for a single nurse to do this as well as provide constant supervision of the patients who have been admitted.
In order to have two nurses on duty at all times during the day, every day of the year, the hospital will have to employ more than two nurses in total. As discussed in the previous section with respect to the Emergency Department, in order to have a nurse present around the clock, a hospital will have to employ 4-5 nurses in total. So, on an inpatient unit, in order to have two nurses for each of the two 12-hour shifts each day, the hospital will need to employ as many as 10 nurses in total. Because of the cost and difficulty of attracting and retaining Registered Nurses (RNs), many hospitals will likely use a combination of an RN and a Licensed Practical Nurse (LPN) on some or all shifts.20
If the hospital pays $38/hour for RNs, $26/hour for LPNs, and provides benefits equivalent to 20% of wages, it would need to spend over $800,000 on nursing staff for an inpatient unit with this many patients.
In addition to the nurses, a hospital will also be likely to employ additional staff to directly support the inpatient unit, such as:
- A Nursing Assistant on each shift, who could carry out a variety of patient care duties to enable the nurses to focus on tasks requiring nursing skills.
- A Unit Secretary/Coordinator, at least on the day shift, to handle calls, visitors, paperwork, and other tasks.
Figure 19
Cost of the Inpatient Unit
at a Hypothetical Small Rural Hospital
Daily Inpatient Census: 3
|
|||
|---|---|---|---|
| Unit Cost | FTEs | Cost | |
| RN | $38/hour | 5.0 | $395,000 |
| LPN | $26/hour | 5.0 | $270,000 |
| Nursing Assistant | $15/hour | 5.0 | $156,000 |
| Other Staff | $16/hour | 2.5 | $83,000 |
| Total Wages | $905,000 | ||
| Benefits | 20% of Wages | $181,000 | |
| Other Direct | $130,000 | ||
| Total Direct | $1,216,000 | ||
| Indirect Cost | 100% of Direct | $1,216,000 | |
| Total Cost | $2,432,000 | ||
Most of the direct costs of the inpatient unit will be associated with the nurses and other staff. As with the Emergency Department, the costs of any medications and other supplies that are billed separately will ordinarily be assigned to a separate hospital cost center (these costs will be discussed separately in the next section), so non-personnel costs for the inpatient unit will generally be a small proportion of the total direct cost.
However, the inpatient unit will depend on the hospital providing space and utilities, maintenance, housekeeping, dietary services, laundry, billing for patient visits, payroll and benefits for staff, medical records, etc., and a portion of the hospital’s costs for those activities must be allocated to the inpatient unit to properly represent the total cost of inpatient care. Typically, the indirect costs will increase the total cost of an inpatient unit by 100% beyond the personnel and other direct costs discussed above.21
Figure 19 shows that the total cost could be expected to be about $2.4 million for an inpatient unit with this level of staffing at a hypothetical hospital.
The Cost of Inpatient Care for a Smaller Number of Acute Patients
A hospital will still likely want a similar level of nurses even if the average daily census is lower than 3. Even if the hospital has only 1 or 2 patients per day on average instead of 3, the random nature of admissions and the seasonality in admission rates means that it will still have 2, 3, or even more patients on some days and it needs to be prepared for that. Moreover, many hospitals with small numbers of admissions also have small emergency departments that rely on the nurses on the inpatient unit to help with ED visits as well as provide care on the inpatient unit, so it would be unsafe to have only one nurse available. A hospital would be less likely to have a nursing assistant or other staff if the total census was very low, but very few hospitals have a total daily census below 2.
The Cost of Inpatient Care for a Larger Number of Acute Patients
Because the nursing staffing levels described above are designed to handle variations in the number of patients, there will be no need to change the staffing levels if the average daily census is slightly higher than 3. If a hospital has a significantly larger number of patients every day, it will need to have additional nurses and potentially other staff on the unit, but the number of staff will not be directly proportional to the number of patients. For example:
- If the average daily census is closer to 6 than to 3, the hospital will likely want 3 nurses on duty on some or all shifts instead of 2 nurses, particularly if a high proportion of the patients are acute admissions rather than patients receiving rehabilitation or long-term care in swing beds.
- If the average daily census is closer to 9 and most of the patients are receiving acute care, the hospital will likely want another nurse on the day shift because of the higher workload during the day than at night.
- If there are an average of 14 patients on the unit, most of whom are acute patients, the inpatient unit begins to look more like an inpatient unit at a larger hospital, except that the staffing will still need to be higher than at a larger hospital because there are no other units at the small hospital to provide backup support and no other nurses to perform admission and discharge tasks, so the hospital may have 4 nurses on every shift.
The table below shows estimated costs for hypothetical hospitals with these levels of staffing, wages, and benefits for the different levels of inpatient census.
Figure 20
Cost of Hypothethical Inpatient Units
With Different Numbers of Patients
| Daily Inpatient Census | ||||
|---|---|---|---|---|
| Acute Census | 2.0 | 4.0 | 6.0 | 9.3 |
| Swing SNF Census | 1.0 | 2.0 | 3.0 | 4.7 |
| Swing NF Census | 0.0 | 0.0 | 0.0 | 0.0 |
| Total Inpatients | 3.0 | 6.0 | 9.0 | 14.0 |
| Staffing (FTEs) | ||||
| RN | 5.0 | 10.0 | 10.0 | 12.0 |
| LPN | 5.0 | 5.0 | 7.5 | 7.5 |
| Nursing Assistant | 5.0 | 5.0 | 5.0 | 7.5 |
| Other Staff | 2.5 | 2.5 | 5.0 | 5.0 |
| Cost | ||||
| RN | $395,000 | $790,000 | $790,000 | $948,000 |
| LPN | $270,000 | $270,000 | $406,000 | $406,000 |
| Nursing Assistant | $156,000 | $156,000 | $156,000 | $234,000 |
| Other Staff | $83,000 | $83,000 | $166,000 | $166,000 |
| Total Wages | $905,000 | $1,300,000 | $1,518,000 | $1,754,000 |
| Benefits | $181,000 | $260,000 | $304,000 | $351,000 |
| Other Direct | $130,000 | $135,000 | $140,000 | $150,000 |
| Total Direct | $1,216,000 | $1,695,000 | $1,962,000 | $2,255,000 |
| Indirect Cost | $1,216,000 | $1,695,000 | $1,962,000 | $2,255,000 |
| Total Cost | $2,432,000 | $3,390,000 | $3,924,000 | $4,511,000 |
Actual vs. Estimated Costs
The estimates shown for the hypothetical hospitals in Figure 20 do not represent what any individual hospital inpatient unit should cost or what the differences in costs between inpatient units of different sizes should be. For example:
- the exact number and types of nurses the hospital employs, and the amounts it pays those nurses, will depend heavily on the hospital’s ability to attract and retain nurses in the community. Hospitals in isolated areas are less likely to have a pool of nurses in the community who are able and willing to work part-time, so a hospital in one of these areas may need to employ more nurses on a full-time basis in order to ensure that it will have adequate coverage for all shifts.
- a hospital in a more isolated area may also need to pay more to hire nurses than a hospital in an area that is closer to an urban center.
- if a nurse retires or resigns, the hospital will likely have to hire a “traveling” nurse to temporarily fill the vacancy, and this will increase the hospital’s personnel costs in the year in which the vacancy occurs.
- if outpatient surgical procedures are performed at a small hospital, there will likely not be enough procedures to support a separate nursing staff for that, and so the nurses on the inpatient unit will spend a portion of their time assisting with the procedures and the patients’ recovery. The portion of the inpatient nurses’ time that is assigned to the surgical cost center will reduce the cost of the inpatient unit, but the hospital may also need a higher number of nurses on the days when surgical procedures are performed than if the nurses were only caring for inpatients.
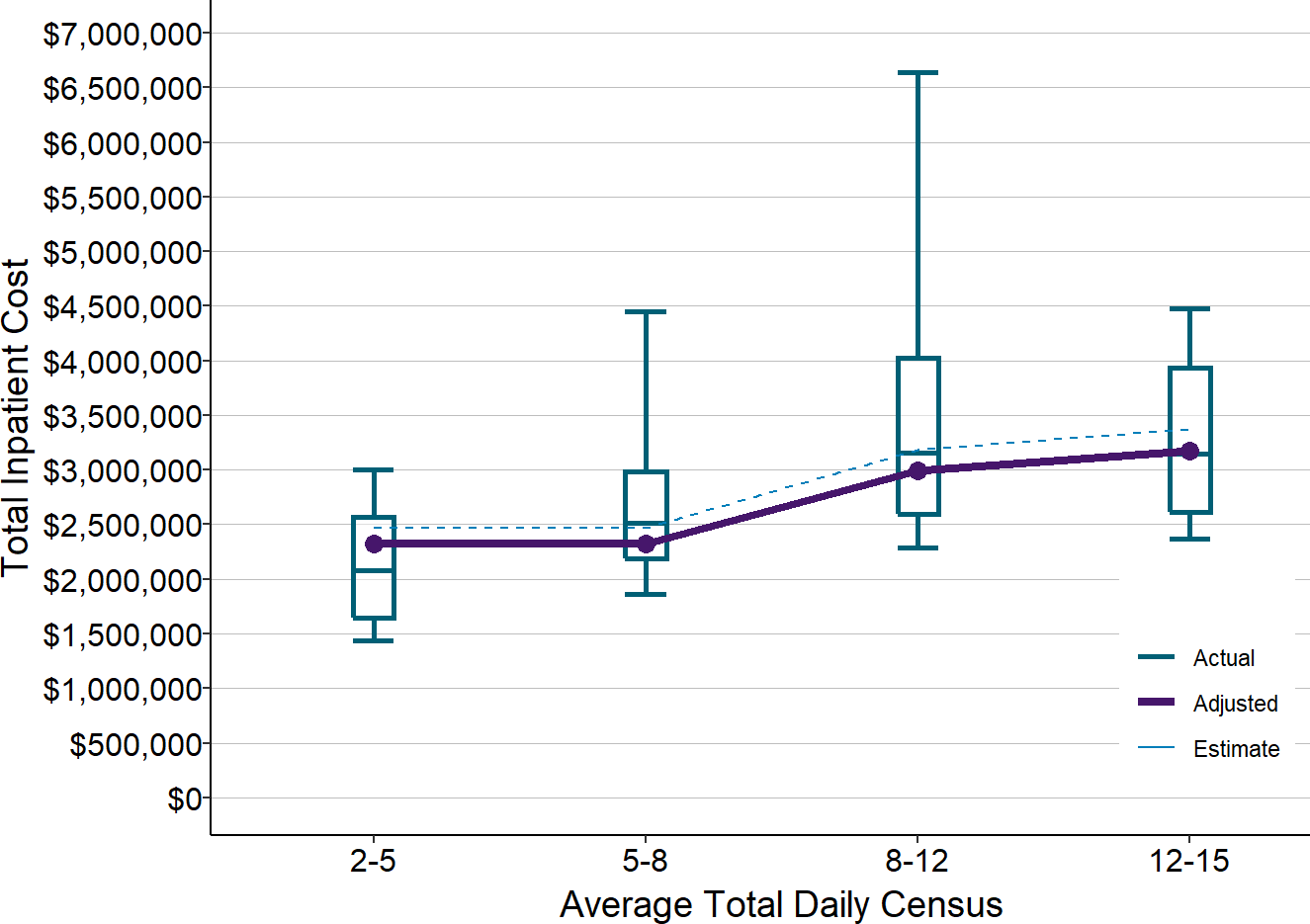
Nonetheless, the cost models provide useful insights into what it can cost to operate inpatient units at small rural hospitals and the potential magnitude of differences based on size. As shown below, the estimated costs in Figure 20 are similar to the median actual costs for rural hospitals, but there is also considerable variation for individual hospitals.22
Figure 21
Actual vs Estimated Costs of Inpatient Units
at Small Rural Hospitals
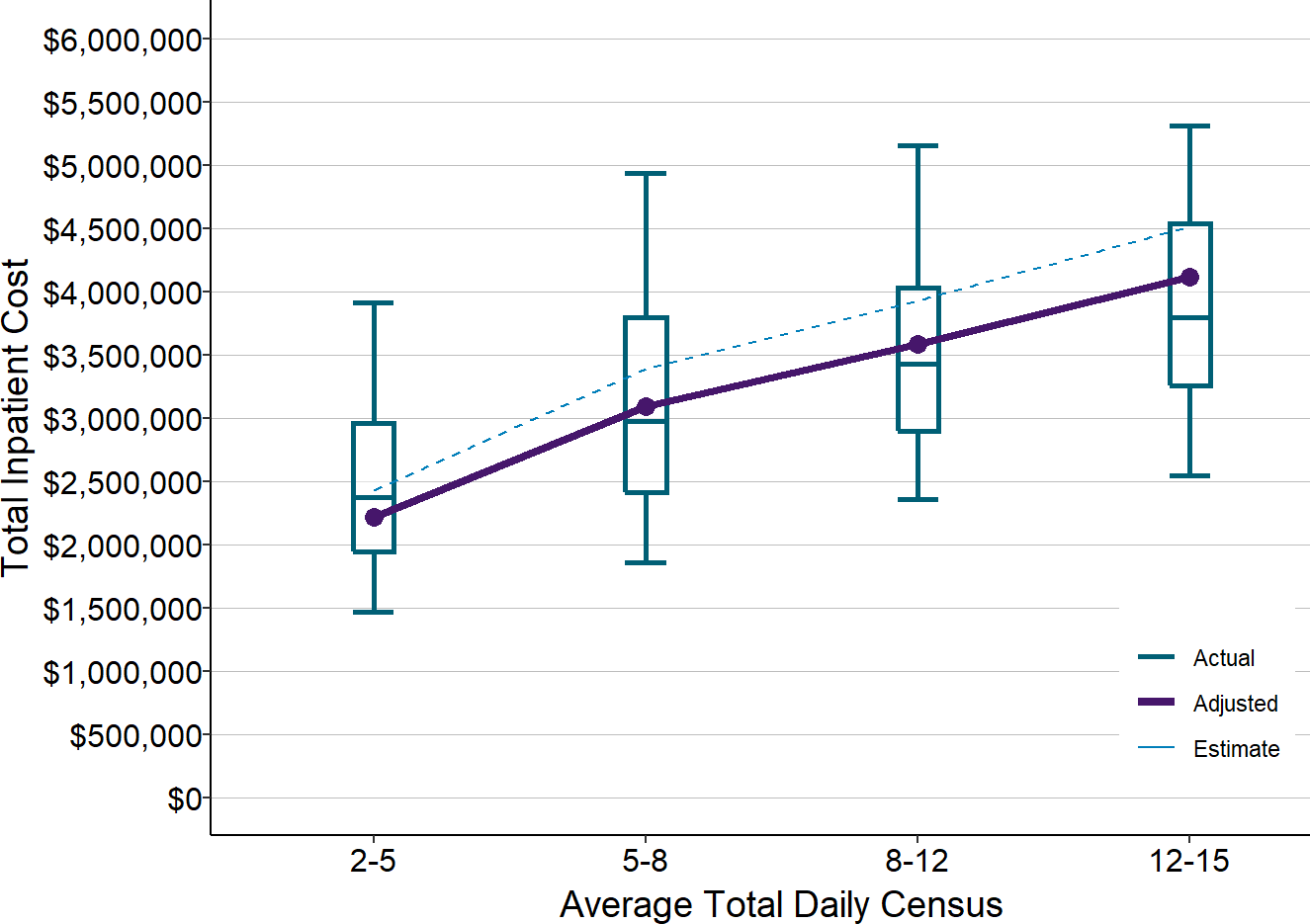
Actual amounts are from 2017-19 at rural hospitals with less than $30 million in total expenses. Estimates (dotted line) are from Figure 20. Adjusted values (solid line) are the estimated values reduced to reflect inflation between 2018 and 2020.
The Cost of Inpatient Care with Large Numbers of Swing Bed Patients
As discussed earlier, some small rural hospitals have a small number of patients receiving acute care but a large number of long-term nursing care patients in swing beds. These hospitals may have the same total number of patients in inpatient beds each day as other hospitals, but the average acuity level of the patients will be lower, so the number and types of staff needed will likely be somewhat different. For example, although the hospital will still need to have at least 2 nurses, including one RN, to handle the work associated with the acute patients, they may have more LPNs and more nursing assistants for the patients in swing beds than if those patients were acute patients. The following table shows what the costs might look like with hypothetical levels of staffing and wages for different numbers of patients.
Figure 22
Cost of Hypothetical Inpatient Units
With Different Types of Patients
| Daily Inpatient Census | ||||
|---|---|---|---|---|
| Acute Census | 0.5 | 1.0 | 1.5 | 2.3 |
| Swing SNF Census | 1.0 | 2.0 | 3.0 | 4.7 |
| Swing NF Census | 1.5 | 3.0 | 4.5 | 7.0 |
| Total Inpatients | 3.0 | 6.0 | 9.0 | 14.0 |
| Staffing (FTEs) | ||||
| RN | 5.0 | 5.0 | 5.0 | 5.0 |
| LPN | 5.0 | 5.0 | 7.5 | 7.5 |
| Nursing Assistant | 5.0 | 5.0 | 7.5 | 10.0 |
| Other Staff | 0.0 | 0.0 | 2.5 | 2.5 |
| Cost | ||||
| RN | $395,000 | $395,000 | $395,000 | $395,000 |
| LPN | $270,000 | $270,000 | $406,000 | $406,000 |
| Nursing Assistant | $156,000 | $156,000 | $234,000 | $312,000 |
| Other Staff | $0 | $0 | $83,000 | $83,000 |
| Total Wages | $822,000 | $822,000 | $1,118,000 | $1,196,000 |
| Benefits | $164,000 | $164,000 | $224,000 | $239,000 |
| Other Direct | $250,000 | $250,000 | $250,000 | $250,000 |
| Total Direct | $1,236,000 | $1,236,000 | $1,592,000 | $1,685,000 |
| Indirect Cost | $1,236,000 | $1,236,000 | $1,592,000 | $1,685,000 |
| Total Cost | $2,472,000 | $2,472,000 | $3,183,000 | $3,370,000 |
Here again, the exact number and types of nurses and other staff that a hospital employs, and the amounts that it pays those employees, will depend heavily on the ability of the hospital to attract and retain nurses and other staff in the community. As shown in the figure below, the costs at the hypothetical hospitals above are similar to the median costs at actual hospitals with those numbers and types of patients, but there is considerable variation among individual hospitals.
Figure 23
Actual vs. Estimated Costs of Inpatient Units
at Small Rural Hospitals with Many Swing Bed Patients
Actual amounts are from 2017-19 at rural hospitals with less than $30 million in total expenses. Estimates (dotted line) are from Figure 22. Adjusted values (solid line) are the estimated values reduced to reflect inflation between 2018 and 2020.
This shows that another reason for variation in inpatient costs across different hospitals is the difference in the types of patients at those hospitals. Even if two hospitals have the same average number of acute inpatients, the cost of the inpatient unit will be higher if it also has a large number of patients in swing beds. Conversely, if two hospitals have the same number of total inpatients, the cost of one inpatient unit will be higher if a higher proportion of the patients are acute admissions.
Differences in the Average Cost Per Patient Between Different Hospitals
Although the total cost of operating an inpatient unit will generally be higher for inpatient units with more patients, the analysis above shows that the differences in costs will not be proportional to the differences in the number of patients. The estimated cost in Figure 20 for a hospital with an average daily census of 6 is only 39% higher than the estimated cost for a hospital with an average census of 3, even though there are twice as many patients on an average day. On the other hand, the total cost may not differ at all for hospitals that have only small differences in the number of patients; in the example, the same staffing would likely be appropriate whether the average daily census is 2.5, 3.0, or 3.5, and so the cost could be the same even though the number of patients differs by as much as 33%.
This means that the average cost per patient day will be significantly lower at hospitals with higher numbers of patients. As shown below, the average cost per patient day at the hypothetical hospital with an average daily census of 3 is $2,221, while the average cost per patient day for the hypothetical hospital with an ADC of 6 is $1,548, i.e., 30% less. At the high end of the range, the cost per day at the hospital with an average of 14 patients per day is $883, which is less than half the cost at the hospital with an average of 3 patients.
Figure 24
Differences in the Estimated Cost Per Inpatient Day
at Hospitals with Different Numbers of Patients
| Daily Inpatient Census | ||||
|---|---|---|---|---|
| Acute Census | 2 | 4 | 6 | 9 |
| Swing SNF Census | 1 | 2 | 3 | 5 |
| Swing NF Census | 0 | 0 | 0 | 0 |
| Total Inpatients | 3 | 6 | 9 | 14 |
| Cost | ||||
| Total Cost | $2,432,000 | $3,390,000 | $3,924,000 | $4,511,000 |
| Cost Per Service | ||||
| Cost Per Day | $2,221 | $1,548 | $1,195 | $883 |
The figure below shows that the actual cost per day at rural hospitals follows this pattern. The median cost per day at hospitals with small numbers of inpatients is double, triple, or even quadruple the median cost per day at hospitals with larger numbers of patients.
Figure 25
Cost Per Inpatient Day
at Small Rural Hospitals
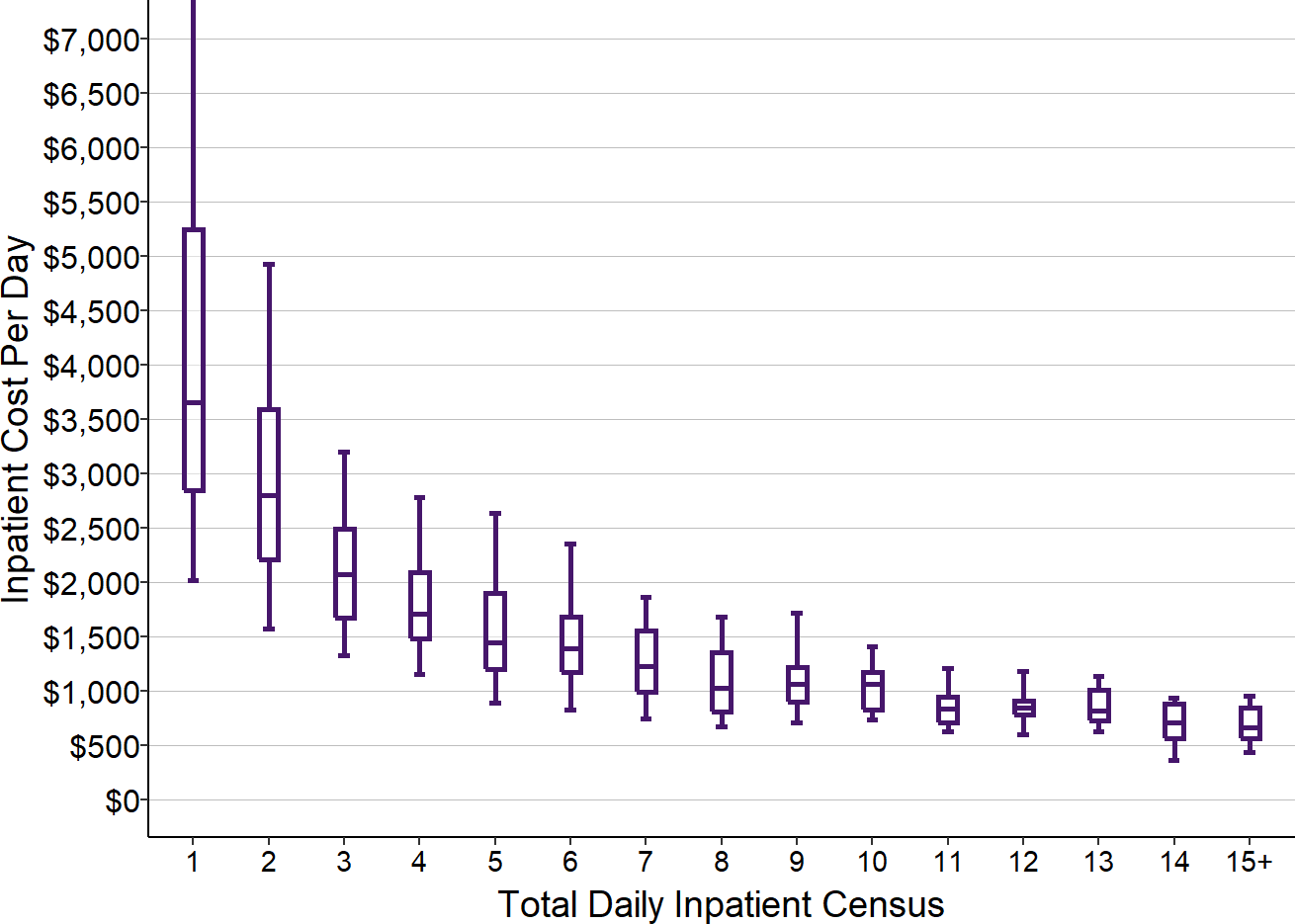
Values are the medians for 2017-19 at rural hospitals <$30M total expenses where long-term nursing care patients in swing beds represented less than 5% of all inpatient days.
The fact that some hospitals have higher costs per day than hospitals with a smaller census does not necessarily represent inefficiency; in some cases, it is simply due to variations from community to community in the ability to attract and retain nurses and other staff.
The average cost per patient at a hospital will depend not only on the average cost per patient day, but also the average length of stay for the patients. The average length of stay for acute inpatients at small rural hospitals is about 3 days, so the total bed and board cost of an inpatient stay will generally be hundreds or thousands of dollars higher at hospitals with fewer patients.23
The Problems Caused by Per Diem and Per Case Payments
Although the cost of operating an inpatient unit is not directly proportional to the number of patients, the hospital’s revenue usually is. Hospitals are generally paid for inpatient care either through a per-diem fee (i.e., a payment for each day that a patient spends in the hospital) or a single case rate (a payment for the entire hospital stay regardless of how long the patient is in the hospital). As a result, when the number of patients admitted to the hospital increases, the hospital’s revenue increases proportionally, and when the number of admissions decreases, so does revenue.24
This approach to payment causes the same kinds of problems for the inpatient services delivered by small rural hospitals that fees for ED visits cause for the emergency department.
Payments for hospitalizations that are adequate for larger hospitals will cause losses at small rural hospitals.
For inpatient units with a total daily census above 9, the median cost per day was under $1,000, so a per diem payment of $1,000 would be sufficient to cover the cost of the nursing care for those patients. However, a $1,000 per diem payment would cause significant losses at hospitals with fewer patients. Those hospitals that have to pay more to attract and retain an adequate number of nurses and other staff will also have greater losses if they are paid the same amount per patient as other hospitals of similar size.
Even if the per-diem or case rate amounts appear adequate to cover the costs of inpatient services when the year begins, if unexpected vacancies occur in the nursing staff that require the hospital to hire temporary nurses, the cost of the inpatient unit will increase and the payments may no longer be adequate.
The adequacy of any payment amount depends on how many patients are actually admitted.
As with visit-based fees in the emergency department, the problem with per diem and per admission payments for inpatient care is not just the amount of payment, but the method of payment. Because revenues change in direct proportion to the number of admissions when admissions increase or decrease, but costs barely change at all, even small changes in the number of patients admitted can result in larger or smaller losses or profits.
Figure 26
Impact of Changes in the Number of Inpatients
on the Cost Per Inpatient Day
| Daily Inpatient Census | |||
|---|---|---|---|
| Acute Census | 3.8 | 4.0 | 4.2 |
| Swing SNF Census | 1.9 | 2.0 | 2.1 |
| Swing NF Census | 0.0 | 0.0 | 0.0 |
| Total Inpatients | 5.7 | 6.0 | 6.3 |
| Cost | |||
| Total Cost | $3,390,000 | $3,390,000 | $3,390,000 |
| Cost Per Service | |||
| Cost Per Day | $1,629 | $1,548 | $1,474 |
Figure 24 showed that for the hypothetical hospital with an average total census of 6.0, an average per diem payment of $1,600 would be large enough to cover the costs of the inpatient unit and make a small profit. However, if it turns out that the hospital has 5% fewer patients than expected, resulting in an average total census of only 5.7, the total cost of the inpatient unit would still be the same, but the cost per day would increase above $1,600. As a result, the $1,600 per diem that would have been adequate with a census of 6.0 would result in a loss when the number of patients decreases by a small amount. Conversely, if the hospital happened to experience a 5% increase in the number of patients, the hospital’s cost per day would decrease by 5% (because the same number of staff are needed but the cost can be spread across a larger number of patients) and profits would increase significantly.
It is impossible to predict exactly how many patients will be admitted to a hospital over the course of a year, so even if the payment appears adequate at the beginning of the year, it may well turn out to be inadequate by the time the year ends.
Hospitals face tradeoffs between quality, affordability, and the financial viability of services
Payments for inpatient care create the same kinds of problematic tradeoffs between quality, affordability, and financial viability for hospitals that were described in the previous section with respect to the emergency department:
- Patients on an inpatient unit can receive more individualized attention if there are more nurses and other staff working on the unit, but it will cost more to have more staff, and the hospital may not be able to charge or be paid enough to cover the higher cost.
- Better chronic care management and preventive care can not only reduce ED visits, they can also reduce the number of patients who need to be admitted to the hospital. However, the hospital is paid if the patient is admitted and it is not paid for inpatient care if the patient does not need to be admitted, so the hospital is penalized financially if the residents of the community are healthier.
- In order to receive payments for hospital admissions from private insurance plans that are sufficient to cover the costs of the inpatient unit, the hospital will have to set its charges several times higher than the cost, which will make hospital care less affordable for people without insurance.
Differences in Costs and Payments for Acute Admissions vs. Swing Bed Patients
The problems associated with mismatches between payments and costs for inpatient services are magnified in small rural hospitals because of the use of swing beds. In general, patients admitted for acute care will require more nursing time than patients in swing beds, so it would be inappropriate for the hospital to charge or be paid the same per diem or per patient amount for an acute patient as is paid for a swing bed patient. Similarly, many swing bed patients receiving post-acute care will have more intensive nursing care needs than long-term care patients, so payments for the post-acute care patients should, in principle, reflect that difference.
If the payments for rehabilitation or long-term care patients in swing beds are below the cost of delivering care to them, that will exacerbate the losses caused by low payment for acute patients. Medicare and most commercial insurance plans do not pay at all for long-term nursing care, and Medicaid payments for long-term care are generally less than what it costs to deliver that care either in a hospital or a separate nursing facility, so losses for a rural hospital can be particularly high if the hospital happens to have fewer acute or rehabilitation patients and more long-term nursing patients in swing beds during a particular period of time.
The Cost of Ancillary Services in Small Rural Hospitals
The Number and Types of Ancillary Services in Small Rural Hospitals
Many of the patients who come to a rural hospital’s Emergency Department will need a laboratory test or an imaging study to assist in diagnosis of their condition. Patients who are admitted to the hospital will typically need laboratory testing and potentially imaging studies to monitor their condition during their stay. Patients who receive rehabilitation in a swing bed will need therapy services (physical therapy, occupational therapy, speech therapy) in addition to nursing care.
These “ancillary” services are not delivered by nurses but by laboratory technicians, radiology technicians, and therapists who have specialized training, and they require the use of specialized laboratory, radiology, and therapy equipment and supplies. As a result, the grand total of the costs associated with a patient’s emergency department visit or an inpatient stay is higher than the costs associated with the ED and inpatient unit described in the previous sections.
However, the majority of patients who receive these ancillary services are not patients in the hospital ED or inpatient unit; they are patients in the community who need a lab test, imaging study, or therapy in conjunction with ambulatory care they are receiving from a primary care physician or specialist. The availability of these services is an important way that rural hospitals help the residents of their community stay healthy.
Since different patients receive different numbers and types of ancillary services, a charge for each service must be billed to a patient and their health insurance plan. Medications given to patients and medical supplies used during an inpatient stay or emergency department visit are also treated as ancillary services and they are billed separately to patients and health plans. Many small rural hospitals deliver one or more ancillary services beyond laboratory, radiology, therapy, drugs, and medical supplies, such as surgery or maternity care, but these other services represent a relatively small part of the total costs for most small rural hospitals. (Indeed, many hospitals that are larger in terms of total expenses are larger not only because they serve larger communities, but because they offer a broader array of ancillary services.)
Although hospitals report their total charges for each category of ancillary services on their cost reports, they do not report exactly how many and what types of lab tests, imaging studies, therapy services, drugs, etc. they provided, and there are no other good sources of data on this. This is partly because there is no easy way to measure the volume of ancillary services in a comparable way across hospitals. For example, there are hundreds of different laboratory tests, some of which are very simple while others are much more complex (e.g., a “comprehensive metabolic panel” is generally ordered and billed as one test, but it is actually a collection of several separate tests), so knowing that one hospital delivered “more laboratory tests” than another hospital is not very helpful. Due to variation in the amounts hospitals charge for individual tests, imaging studies, and other services, differences between hospitals in the total charges they bill for a group of services do not give any reliable indication as to the difference in the volume or types of services delivered at the hospitals. Although there is a system of “relative value units” (RVUs) assigned to different services that Medicare and other payers use for setting payment amounts, the difference in RVUs is not necessarily proportional to the difference in costs at a small hospital, so even if one knew that one hospital delivered more RVUs than another, that would still not allow clear conclusions to be drawn about whether its costs should be higher.
The Cost of Laboratory Services in Small Rural Hospitals
Because each type of ancillary service is delivered by different types of staff with different types of equipment and supplies, the costs associated with each type of service are tracked in separate cost centers. In most hospitals, the laboratory is the largest ancillary service in terms of total cost, partly because of the large number of residents in any community who will need a lab test for some purpose during the course of a year.
There are three primary components of the cost of operating a hospital laboratory: (1) laboratory technicians, (2) laboratory equipment, and (3) the materials and chemicals used for individual tests. The hospital cost reports do not provide information on these separate components, but it is possible to estimate what the costs would be in laboratories of different sizes.
Laboratory Technicians
Even the smallest hospital will need at least one full-time laboratory technician (lab tech) who is trained to perform the minimum set of tests needed for immediate diagnosis and treatment of patients, such as urine tests, blood tests, and pregnancy tests.25 Although a single lab tech working a 40 hour week might have the capacity to process all of the tests at a very small hospital26, there could be problematic delays when multiple tests are needed quickly at the same time. The lab tech would also have to be on call to come to the hospital at night or on weekends if a patient comes to the ED and needs a test that can’t be performed by the ED staff, or if an inpatient experiences a problem during the night that requires a test to diagnose. Moreover, employing a single laboratory technician provides no coverage for illnesses, vacations, etc. and places all of the on-call burden on one individual. As result, except for the very smallest communities, a rural hospital will likely want to have at least two full-time laboratory technicians.27
The higher the volume of testing, the more lab techs the hospital will need in order to provide timely processing of tests. However, in contrast to the inpatient unit, where each increment in the nursing staffing level requires 4-5 additional FTE employees, staffing in the laboratory can be increased in increments of a single FTE. The more ED visits the hospital has, particularly at night, the more important it will be to have round-the-clock staffing in the laboratory rather than expecting the daytime lab techs to be on call. However, since the majority of tests will not be for emergency visits, most of the testing work can be scheduled to occur during the daylight shift on weekdays, which enables more efficiency and flexibility in staffing.28
Equipment and Supplies
Every hospital will need the minimum level of laboratory equipment required to perform the most commonly used tests; this will require not only purchasing or leasing the equipment, but also ongoing costs for maintenance and calibration of the equipment. The more tests that are performed, the more equipment that will be needed, but since a single piece of laboratory testing equipment can be used across multiple shifts and not every test uses the same testing device, the increment of testing volume that triggers the need for additional equipment may be larger than the increments that trigger an increase in laboratory technicians. On the other hand, with a higher total volume of testing, the hospital will also be more likely to have requests for less common tests that can only be performed if the hospital has additional types of equipment, and meeting that demand will increase the cost of equipment acquisition and maintenance at a hospital with higher volumes of testing.
The laboratory will also need an inventory of the supplies and chemicals required to perform the tests on the equipment. The more tests that are performed, the higher spending will be on non-reusable supplies and chemicals.
Indirect Costs
The operation of the laboratory depends on the hospital providing space and utilities, maintenance for equipment, housekeeping, billing for tests performed, payroll and benefits for staff, and medical records. Consequently, a portion of the hospital’s costs for those activities must be allocated to the laboratory to properly represent the total cost of operating the laboratory. Typically, these indirect costs increase the total cost of a laboratory at a small hospital by 40-45% beyond the direct cost associated with personnel, equipment, and supplies.
Total Cost of Small Hospital Laboratories
The table below shows what the total cost of hypothetical hospital laboratories of different sizes could be, using assumptions about the number of lab techs, the wage rates they are paid, and the cost of equipment and supplies.
Figure 27
Estimated Cost of the Laboratory
at Hypothetical Small Rural Hospitals
| Population | |||||||
|---|---|---|---|---|---|---|---|
| Population | 1,500 | 5,000 | 7,000 | 9,000 | 15,000 | 20,000 | |
| Staffing (FTEs) | |||||||
| Laboratory Tech | 2.0 | 4.0 | 5.0 | 6.0 | 7.0 | 8.0 | |
| On Call Tech | 0.6 | 0.1 | 0.0 | 0.0 | 0.0 | 0.0 | |
| Cost | |||||||
| Laboratory Tech | $28/hour | $116,000 | $233,000 | $291,000 | $349,000 | $408,000 | $466,000 |
| On Call Tech | $28/hour | $34,000 | $7,000 | $0 | $0 | $0 | $0 |
| Total Wages | $151,000 | $240,000 | $291,000 | $349,000 | $408,000 | $466,000 | |
| Benefits | 20% of Wages | $30,000 | $48,000 | $58,000 | $70,000 | $82,000 | $93,000 |
| Other Direct | $187,000 | $290,000 | $364,000 | $437,000 | $510,000 | $583,000 | |
| Total Direct | $368,000 | $578,000 | $713,000 | $856,000 | $999,000 | $1,142,000 | |
| Indirect Cost | 45% of Direct | $165,000 | $260,000 | $321,000 | $385,000 | $450,000 | $514,000 |
| Total Cost | $533,000 | $838,000 | $1,034,000 | $1,242,000 | $1,449,000 | $1,656,000 | |
As with the hypothetical estimates for emergency departments and inpatient units described in previous sections, these cost estimates for hypothetical laboratories are not intended to represent what the cost of a laboratory at any individual hospital should be, or exactly how large the differences in costs between laboratories of different sizes should be. The ability of a small rural hospital to hire laboratory technicians and the wage rate and benefits it will need to pay to do so will vary from community to community; hospitals will have to spend more when they need to replace older equipment, and hospitals in communities where the population is older or less healthy will need to perform more and different kinds of tests.
The figure below shows actual laboratory costs for small rural hospitals. Since there are no data on the actual number of tests performed in different hospitals, the cost estimates are grouped by the estimated population of their service area. Most laboratory testing will be done to support general healthcare services for residents of the community, not for ED visits or patients admitted to the hospital. As a result, it is reasonable to expect that the volume of laboratory testing in a hospital will be more closely correlated with the size of the community than the inpatient or ED volume.
Figure 28
Actual Laboratory Costs
at Small Rural Hospitals
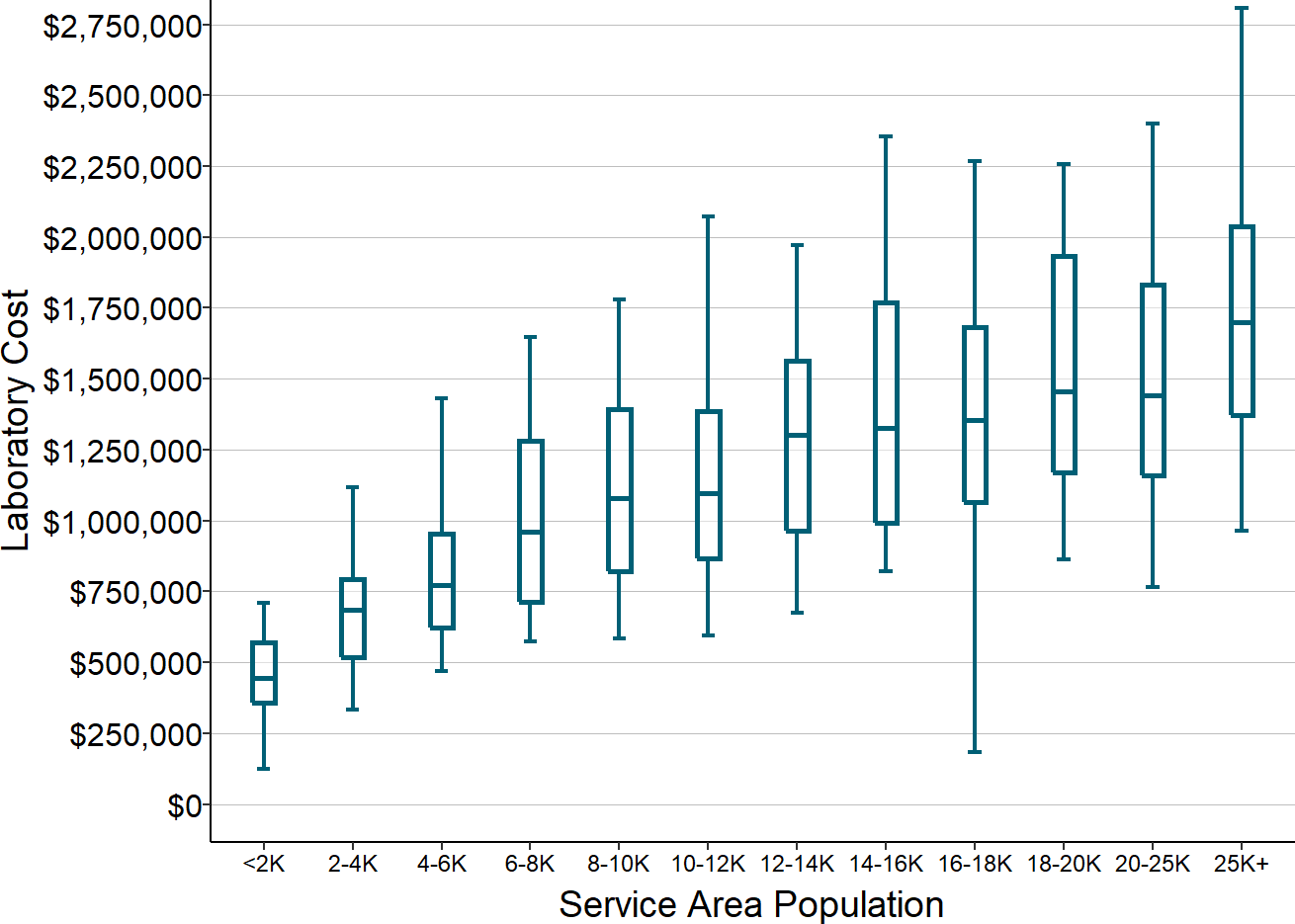
Estimated and actual cost of laboratory services at rural hospitals with less than $30 million in total expenses. Amounts shown are the median for each hospital from 2017-19.
Although there is considerable variation in actual costs at each population level, the medians of the actual costs are very similar to the hypothetical costs for similar-size communities shown in Figure 27. This can be seen more clearly in the chart below, which compares the actual costs for a subset of the service area population categories with the hypothetical estimates for various levels of staffing that would likely be used by many hospitals in communities of those sizes.29
Figure 29
Actual vs. Estimated Costs of Laboratories
at Small Rural Hospitals
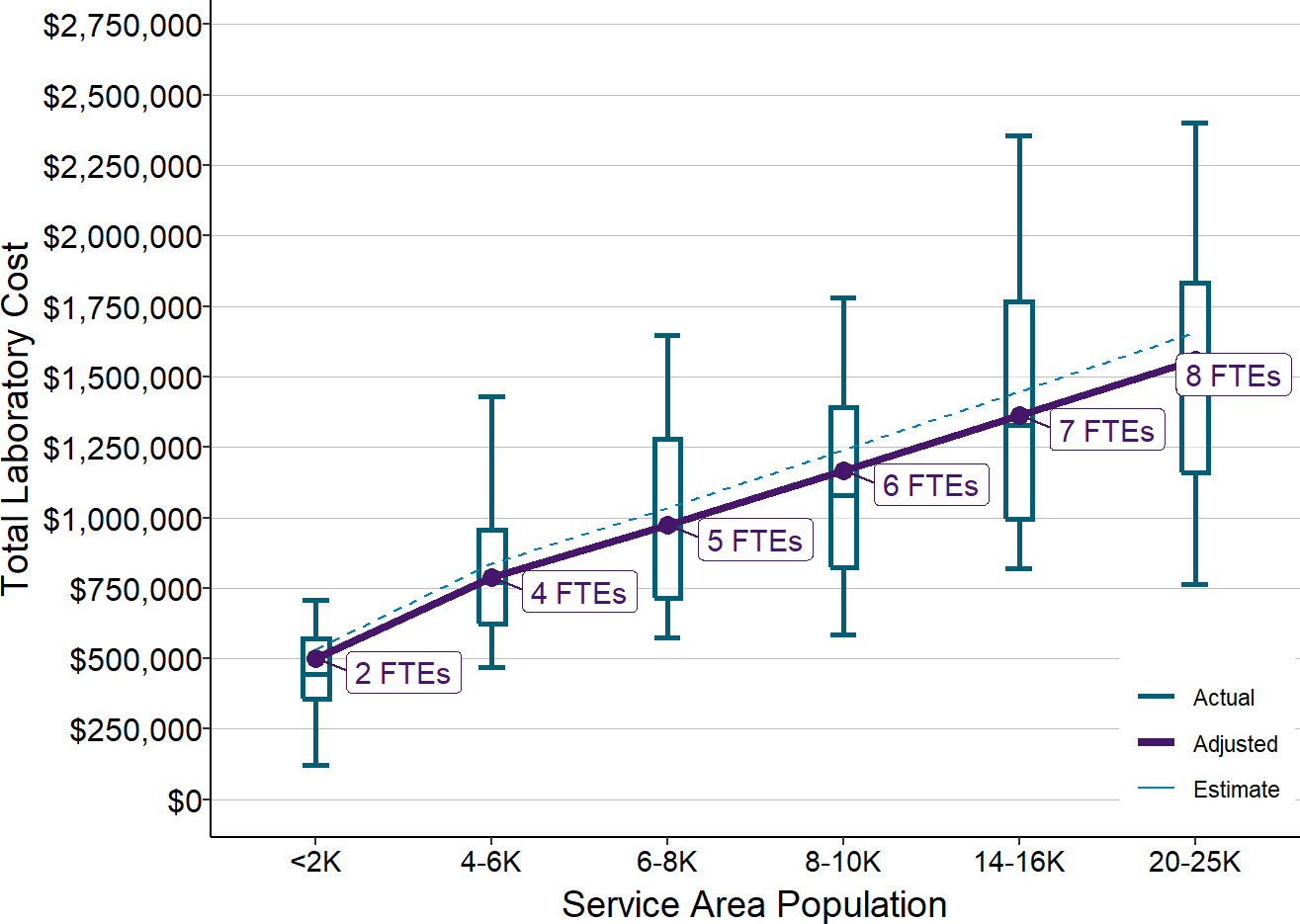
Actual amounts are from 2017-2019 at rural hospitals <$30 million total expense. Estimates (dotted line) are from Figure 27. Adjusted values (solid line) are the estimated values reduced to reflect inflation between 2018 and 2020.
The Impact of Testing Volume on the Cost Per Laboratory Test
Most of the cost of operating the laboratory is associated with the cost of the employees and the laboratory equipment. As a result, at any given level of staffing, the total cost of operating the laboratory will be essentially the same regardless of the exact number of tests the laboratory performs. This means that the cost per test will be lower if more tests are performed within the range of volume that the employees and equipment can handle. However, if the volume of tests at a hospital increases to the point where the hospital needs to add an additional lab tech and equipment, the cost per test will increase.
To illustrate this, assume hypothetically that a laboratory technician can perform a maximum of 8 tests per hour. That means that two technicians, each working 2,000 hours during the year (i.e., a 40-hour week for 50 weeks), could perform as many as 32,000 tests during the year. Assuming the total cost of the laboratory with two technicians is what is estimated in Figure 27, if the lab actually performed 30,000 tests during the year, the average cost per test would be $17.74. However, if the lab only had orders for 25,000 tests, the lab would still need the same number of lab technicians and the total cost would be essentially the same, but the average cost per test would now be $21.29. If the hospital only had 15,000 test orders, it would still likely have the same staffing and costs for the reasons described earlier, but the average cost per test would now be $35.48, double the average cost for 30,000 tests, because there would only be half as many tests performed.
Continuing with the assumption that 8 tests can be performed per hour, if the laboratory had to perform more than 32,000 tests, it would need to hire an additional technician and possibly additional equipment, and this would increase the cost per test by a small amount, but if there were 40,000 or 45,000 tests, the average cost per test would be lower.
As shown in the figure below, the average cost per test likely varies within a relatively narrow range once the volume of tests exceeds a minimum level. However, the cost per test will be much higher for laboratories in smaller communities that do not have as many patients who need tests.
Figure 30
How Changes in Laboratory Testing Volume
Impact the Average Cost Per Test
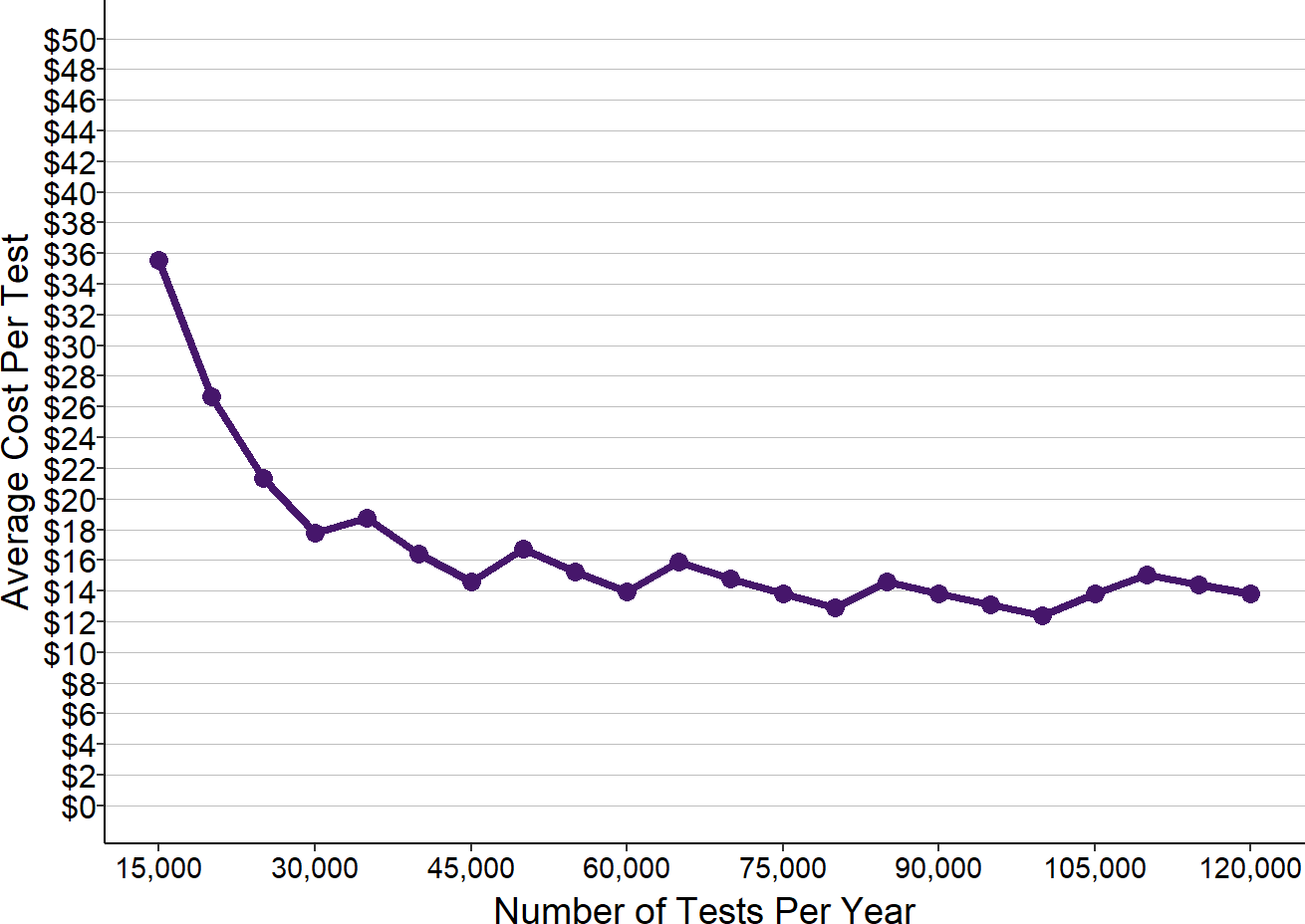
Values shown are based on the estimated laboratory costs at hypothetical hospitals and an estimate of the number of tests that laboratory technicians can perform if 8 tests can be performed every hour.
The Cost of Radiology Services in Small Rural Hospitals
Radiology services are similar to laboratory services in that the cost to the hospital is driven primarily by the number of radiology technicians and the cost of the imaging equipment. Although a physician will need to interpret each image generated by the technicians and equipment, this will generally be done by a radiology practice that bills health insurance plans directly for its services, rather than the hospital itself employing radiologists.
Radiology services are also similar to laboratory services in that the majority of imaging studies will be for community residents, not for patients in the ED or inpatient unit. The total volume of imaging studies at a hospital will generally be much lower than the volume of laboratory tests30, so small hospitals will be likely to have fewer radiology technicians than laboratory technicians. On the other hand, much of the testing equipment in the radiology department is large and expensive; although the smallest hospitals may only be able to offer x-rays, most hospitals will want to offer CT scans, sonograms, and potentially MRIs. In addition, because of the greater space needed to house the equipment, the shielding required due to radiation, and the high electrical power usage, the indirect costs assigned to radiology services will general be higher than for a laboratory.
The table below shows what the total cost of hypothetical hospital radiology departments of different sizes could be, using assumptions about the number of radiology technicians, the wage rates they are paid, and the cost of equipment and supplies. Once again, these are not intended to represent what the cost of radiology services at any individual hospital should be, or exactly how large the differences in costs between laboratories of different sizes should be, since the cost of hiring radiology techs and purchasing/leasing/maintaining equipment will vary from community to community.
Figure 31
Estimated Cost of the Radiology Department
at Hypothetical Small Rural Hospitals
| Population | |||||||
|---|---|---|---|---|---|---|---|
| Population | 1,500 | 5,000 | 7,000 | 9,000 | 15,000 | 20,000 | |
| Staffing (FTEs) | |||||||
| Radiology Tech | 1.0 | 3.0 | 4.0 | 5.0 | 6.5 | 8.0 | |
| On Call Tech | 0.2 | 0.1 | 0.0 | 0.0 | 0.0 | 0.0 | |
| Cost | |||||||
| Radiology Tech | $28/hour | $58,000 | $175,000 | $233,000 | $291,000 | $379,000 | $466,000 |
| On Call Tech | $28/hour | $10,000 | $4,000 | $1,000 | $0 | $0 | $0 |
| Total Wages | $68,000 | $179,000 | $234,000 | $291,000 | $379,000 | $466,000 | |
| Benefits | 20% of Wages | $14,000 | $36,000 | $47,000 | $58,000 | $76,000 | $93,000 |
| Other Direct | $81,000 | $227,000 | $279,000 | $321,000 | $416,000 | $466,000 | |
| Total Direct | $162,000 | $442,000 | $560,000 | $670,000 | $870,000 | $1,025,000 | |
| Indirect Cost | 55% of Direct | $89,000 | $243,000 | $308,000 | $369,000 | $479,000 | $564,000 |
| Total Cost | $252,000 | $684,000 | $868,000 | $1,039,000 | $1,349,000 | $1,589,000 | |
The graphs below show the actual costs of radiology services for small rural hospitals in the U.S. and compare the estimated costs at various levels of staffing are consistent with the costs for actual hospitals.31
Figure 32
Actual Radiology Costs
in Small Rural Hospitals
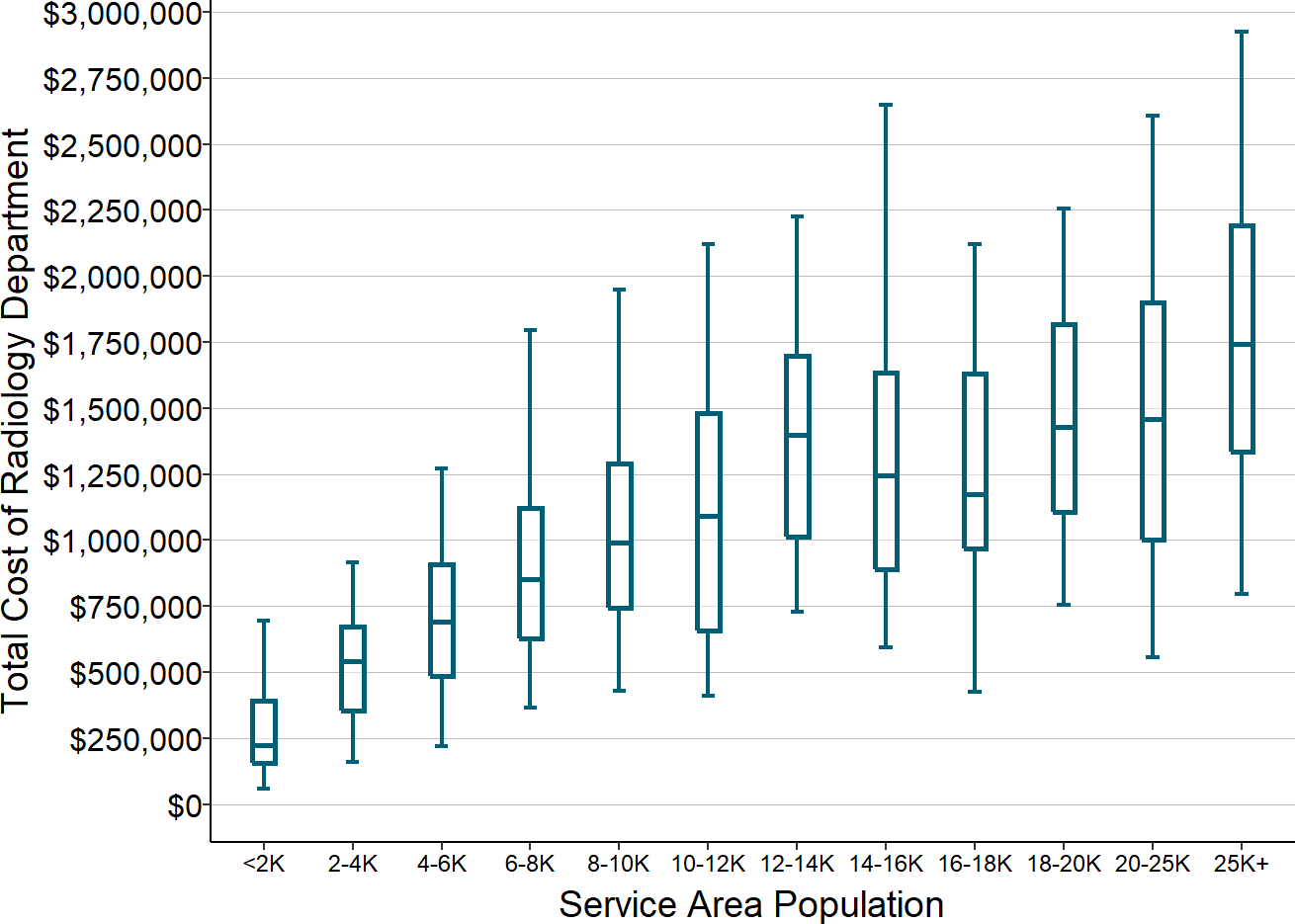
Total cost of radiology services at rural hospitals with less than $30 million in total expenses. Amounts shown are the median for each hospital from 2017-2019.
Figure 33
Actual vs. Estimated Costs of the Radiology Department
at Small Rural Hospitals
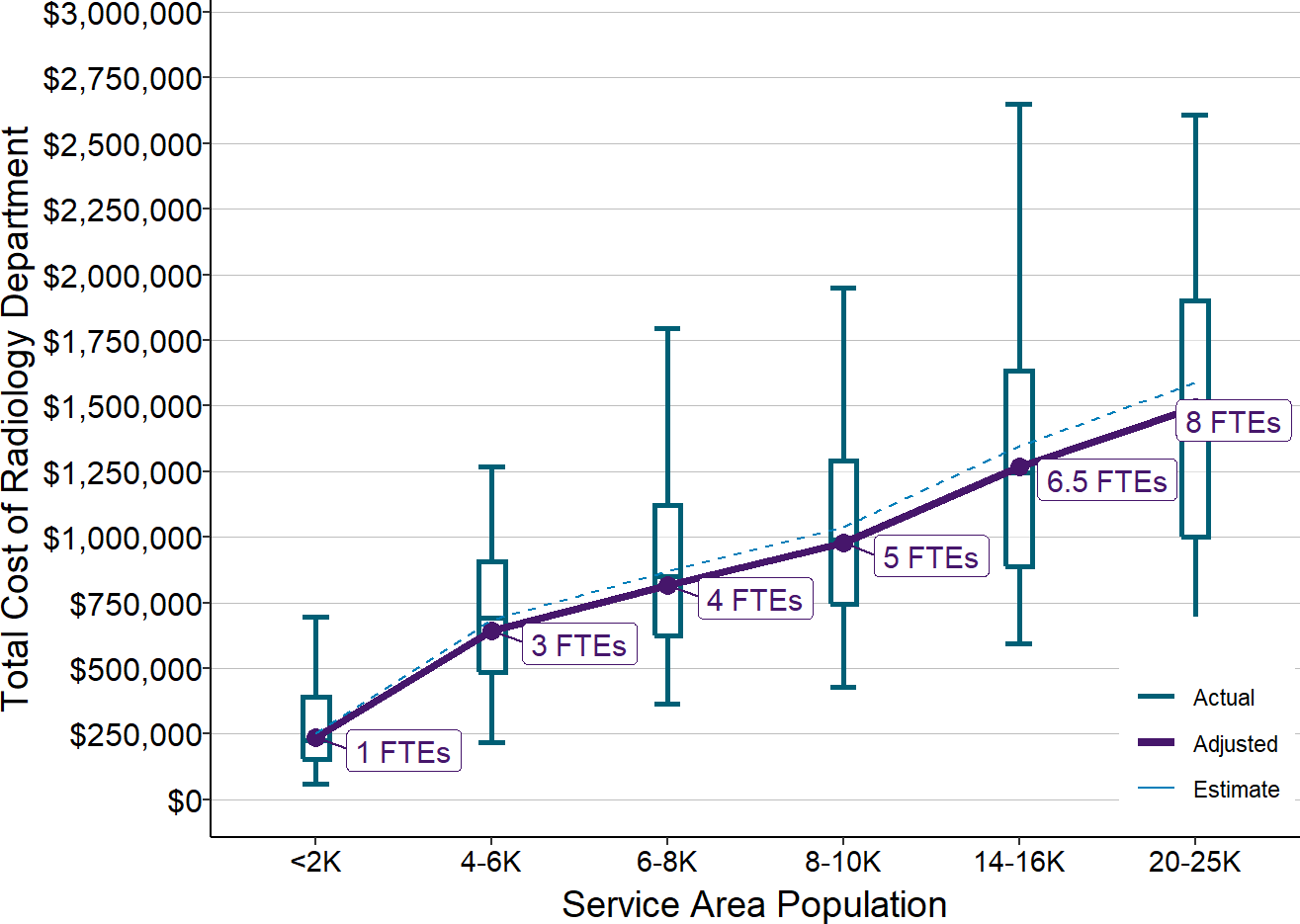
Actual amounts are from 2017-19 at rural hospitals with less than $30 million in total expenses. Estimates (dotted line) are from Figure 31. Adjusted values (solid line) are the estimated values reduced to reflect inflation between 2018 and 2020.
The cost per imaging study will be much higher in a very small hospital that only performs a small number of such studies, since the numerator (the staffing and equipment costs) will be the same, but the denominator (the number of studies) will be lower. At any given level of staffing and equipment, the more tests that are performed, the lower the average cost per test, and the higher the profit for any given amount of payment for the service.
Drugs and Medical Devices and Supplies
As part of the care patients receive during ED visits and inpatient admissions, physicians and nurses administer medications and use a variety of medical devices and supplies, and the hospital charges patients and their health insurance plans separately for these drugs, devices, and supplies.
Primarily Variable Costs Instead of Fixed Costs
The cost of the drugs and supplies to the hospital is primarily driven by the amount the hospital has to pay a manufacturer or wholesaler for each drug or supply item. The hospital may employ staff to purchase and manage the inventory of pharmaceuticals and supplies, and it may need to purchase and maintain equipment needed to store the drugs and supplies safely, but the cost of the employees and equipment is generally very small relative to what is spent to acquire the drugs and supplies.
This is very different from laboratory tests and radiology studies, which the hospital “manufactures” itself using its own staff and equipment. Once a hospital selects a particular level of staffing and equipment, most of the cost of the laboratory or radiology department is a “fixed cost,” i.e., it doesn’t change if more or fewer tests and imaging studies are performed during a particular period of time. In contrast, the cost of drugs and supplies is almost entirely a “variable cost,” i.e., it will change in direct proportion to how many patients the hospital treats and what types of drugs and supplies the patients receive.
Causes of Differences in Costs Between Hospitals
Because there are many different types of drugs, devices, and supplies, and because some individual drugs and other items are far more expensive than others, the cost to the hospital will depend heavily on exactly what conditions patients are treated for and what treatments are used. At hospitals with a small number of patients, a single patient who needs an expensive medication can cause a big increase in the hospital’s total costs for drugs, devices, and supplies from one year to the next.
In addition, two different hospitals can pay different amounts for the same drugs and supply items depending on the discounts and rebates they receive from manufacturers. Since many discounts and rebates are tied to the volume of drugs and products used, smaller hospitals are likely to receive smaller discounts than larger hospitals, and so their costs may be higher even if they treat similar patients in similar ways.
The 340B Program
Most small rural hospitals participate in the federal “340B” program. This program enables hospitals that have large numbers of low-income patients to purchase drugs from the manufacturers at very large discounts.32 Although the program is intended to assist low-income patients, hospitals are not required to use the drugs they purchase solely for such patients.
The Hospital’s Margins for Drugs Will Depend on How It is Paid
Since a small hospital has little control over the cost of the drugs and medical supplies needed for care of its patients, the impact of the drugs/devices/supplies on the hospital’s margin will depend on whether the hospital can charge or be paid more than what it cost the hospital to acquire the drugs and supplies. For hospitals other than Critical Access Hospitals, Medicare “bundles” payment for drugs and supplies used during inpatient stays and many outpatient procedures together with the payment for the nursing care and other services, or it pays pre-defined fees for the drugs. Either approach can result in larger losses for small rural hospitals if their cost for acquiring the drugs or devices is higher than other hospitals. If a private insurance plan pays the hospital a percentage of charges for drugs as well as other services, the hospital may be forced to charge multiple times the acquisition cost in order to receive payments that cover the cost.
Hospitals that participate in the 340B program have not been required to charge Medicare or health plans less for drugs even though the hospital can purchase them at a discount. As a result, the 340B program has enabled hospitals to generate higher profits on drugs administered to patients than they would otherwise be able to receive. However, Medicare is now reducing payments to hospitals for drugs purchased under the 340B program.
The Cost of Other Ancillary Services
In addition to laboratory tests, imaging studies, drugs, and medical supplies, most hospitals provide one or more other ancillary services, such as physical and occupational therapy or surgery. The same kind of analysis shown above can be done to determine the costs for these other ancillary services. The results will have both similarities and differences depending on the following key factors:
- Fixed, Semi-Variable, and Variable Costs. As discussed in the previous section, most of the hospital’s cost for drugs and medical supplies is a variable cost, i.e., the cost will vary in proportion to the number of patients being treated. In contrast, most of the cost of laboratory and radiology services is fixed, at least in the short run, based on whatever decision has been made about the number of staff and equipment. It is actually more accurate to describe the costs as “semi-variable,” because the hospital will need to add more staff and more equipment if the volume of testing/imaging increases sufficiently, and it can reduce staff and equipment if volume decreases sufficiently, but these changes only occur with large changes in volume and they cannot be made instantaneously.
- Number of Patients Needing the Service. Most ancillary service costs are semi-variable rather than either variable or completely fixed, which means that the total cost will depend on the size of the community the hospital is trying to serve. However, differences in cost will not be directly proportional to differences in the number of patients, so the average cost for individual services will be higher when there are fewer patients, as shown earlier for laboratory and radiology services as well as for the ED and inpatient unit.
- Urgency of the Service. Laboratory testing has to be done quickly on a round-the-clock basis because it is an essential service for patients in the Emergency Department and the inpatient unit. As a result, staff and equipment need to be available on site on a 24/7 basis. In contrast, non-urgent outpatient services could be offered only on certain days and certain times, which can facilitate the ability of multiple hospitals to offer the service through use of a shared contractor. For example, physical and occupational therapy (PT/OT) are optional services for a small hospital since they are not used for emergency patients and they are only essential for inpatients if the hospital is offering rehabilitative services in swing beds. This enables many hospitals to contract with external therapy providers who deliver outpatient PT/OT services at the hospital on specific days and times. A small rural hospital can’t provide trauma services because it is unlikely to have round-the-clock access to a surgeon, but it can offer elective surgeries on specific days if there is a surgeon who is willing and able to travel to the hospital to do surgeries on those days.
- Minimum Staffing and Equipment. The minimum cost to provide an ancillary service in a small community will depend on the minimum number of staff and pieces of equipment that are needed to deliver the service at all. For example, the hospital has to have a lab technician and basic laboratory equipment and supplies if it is going to perform even a single lab test, so the hospital cannot spend any less than the cost of that lab technician and equipment. If a physical therapist or surgeon needs a minimum number of cases to justify coming to the hospital to deliver their services, then the hospital will only be able to offer those services if at least that many patients in the community need those services.
- Maximum Capacity of Staff and Equipment. The greater the capacity of individual staff and equipment, the wider the range in the number of patients that can be served with the same staffing and equipment. However, this means that the cost per service will differ significantly between hospitals with service volumes at the low end of the available capacity compared to hospitals with volumes near the maximum capacity.
- Unit Costs of Staff, Equipment, Drugs, and Supplies. Finally, the same number and type of staff, equipment, drugs, etc. will cost different amounts at different hospitals depending on how much those hospitals have to pay to attract and retain staff and what kinds of discounts the hospital can receive on equipment and supplies from manufacturers and suppliers.
The Profitability of Ancillary Services
Hospitals are paid for ancillary services through fees for each individual service delivered, similar to the way they are paid for ED visits and inpatient stays. However, in contrast to the losses they typically incur for the ED and inpatient unit, most small rural hospitals view ancillary services as profitable. A study of ten small rural hospitals in Washington State found that the hospitals lost money on every service except for ancillary services, and the profits on ancillary services offset a portion of the losses they experienced on the emergency department, inpatient unit, clinic, and other services.33 Hospitals that offer surgery have smaller overall losses or higher profits than those that do not offer surgery.
There are several reasons for the profitability difference:
- Low minimum cost to deliver the service. The minimum cost of operating an ancillary service is much less than the minimum cost of operating an ED or inpatient unit; for example, the cost of hiring two laboratory technicians and buying or leasing the associated laboratory equipment is much less than the cost of employing ED physicians and nurses. As a result, the average cost per service is much lower.
- Ability to set charges much higher than costs. The profitability of a service line is based on whether the payment for each service is higher than the average cost of the service. As discussed in the section on ED visits, many insurance plans pay hospitals “discounted charges,” so the profitability of a service line will depend on how high the hospital sets its charges for the services. Because the average cost of most ancillary services is relatively low, it is easier for the hospital to set charges at a higher multiple of costs. Most small rural hospitals charge much more for ancillary services relative ·to the cost of those services than they do for ED visits and acute inpatient care.
- High volume of services. A small amount of profit for each service can translate into a large aggregate profit for the service line if there are a large number of services delivered. For example, small hospital laboratories will deliver thousands or tens of thousands of tests each year, so each dollar of profit on one laboratory service translates into thousands or tens of thousands of dollars in overall profit for the hospital.
Figure 34
Differences in Markup of Charges Over Cost
by Service Line in Small Rural Hospitals
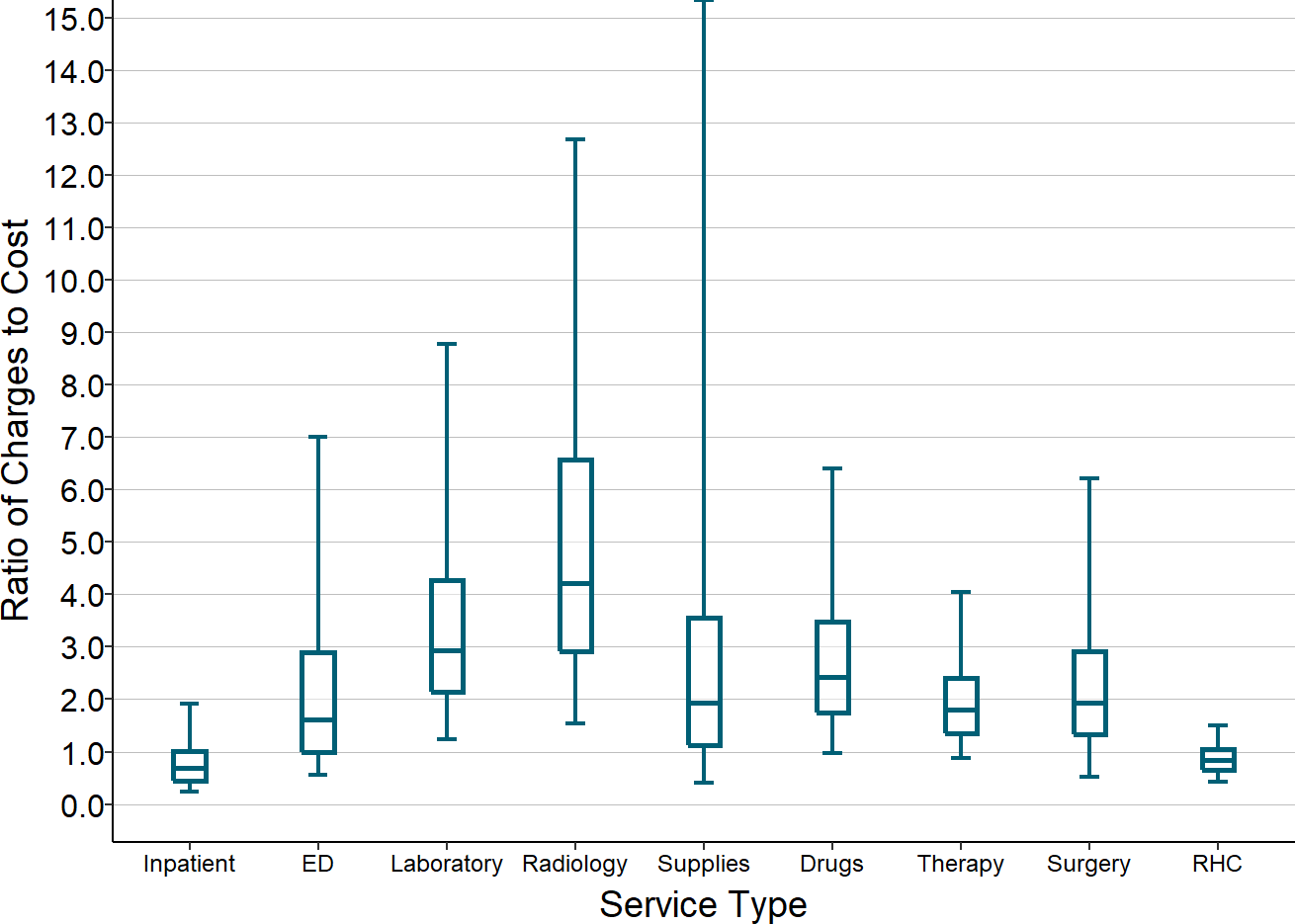
Service line charges divided by costs (inverse of the cost-to-charge ratio) in rural hospitals with less than $30 million in total expenses. Values are medians for the most recent three years available.
The Problems Caused by Ancillary Service Fees
However, as discussed in earlier sections, the problem with fee-for-service payment is not just the amount of payment, but the method. The fact that laboratory and radiology services are profitable for many small hospitals does not eliminate the problematic incentives created by fee-for-service payments:
- Hospitals are rewarded financially for ordering and delivering unnecessary ancillary services. At each level of staffing and equipment, the profitability of an ancillary service line will be higher if more services are delivered. This creates a financial incentive to order more tests and imaging studies as part of an ED visit or hospital admission.
- Hospitals are penalized financially when patients stay healthier. If better chronic care management and preventive care results in fewer patients coming to the ED or requiring a hospital admission, not only will revenues for ED visits and hospital admissions decrease, fewer ancillary services will be needed and ancillary service revenues will also decrease.
- Patients have to pay more in order for the hospital to avoid losses. If a hospital charges more in order to generate profits on ancillary services, a portion of those charges will be paid partly or fully by patients. Patients without insurance will have to pay the full charge for a lab test, x-ray, or therapy service, and patients with high-deductible health plans will have to pay the discounted charge for the service. This can discourage patients from receiving tests and services that they need to diagnose and manage their health problems.
The Cost of Delivering Rural Health Clinic and Primary Care Services
The same factors that make it difficult to financially sustain a hospital in a rural community make it difficult for a primary care physician to establish and maintain a practice in the community. There is widespread recognition that the typical amounts paid by health plans for primary care services are not sufficient to cover the costs of operating small primary care practices even in urban areas. In a small, rural community, those payments will fall even farther below the costs of operating a primary care practice because there are fewer patients who need primary care services. This has contributed to the shortage of primary care practices in many rural communities.
One of the steps taken by Congress to try and address this problem was to require that Medicare and Medicaid pay differently for primary care services when they are delivered through a primary care practice designated as a Rural Health Clinic (RHC). Moreover, Medicare payments for a Rural Health Clinic can be significantly higher if the RHC is part of a hospital with less than 50 beds than if it is a “freestanding” clinic. As a result, two-thirds of small rural hospitals operate a Rural Health Clinic. Most of them operate a single RHC, but 23% operate two RHCs, 13% operate three, and 6% operate four or more in order to make the clinics more accessible to residents living in different parts of the hospital’s service area.
While these Rural Health Clinics provide a very valuable service in the communities served by the hospitals, they generally create or exacerbate financial problems for the hospitals because of the low payments from private health insurance plans. Although Medicare payments for RHCs are “cost-based,” the payments are still less than the cost of services at RHCs, and Medicaid payments are not required to be based on current costs.34
Understanding the reasons for these losses and how to address them requires an understanding of what it costs to deliver primary care in a rural community and what it costs to operate a Rural Health Clinic.
The Volume of Services at Rural Health Clinics
The vast majority of revenue for any primary care practice comes from the fees paid for patient visits. In a typical primary care practice, Medicare and most other payers pay more for a visit with a new patient than for a follow-up visit with an established patient, and the payment is higher for a visit that is longer or involves multiple health problems. If a nurse practitioner or physician assistant sees the patient instead of a physician, the payment is lower. Clinicians can also bill separately for additional services they deliver beyond the basic visit; for example, if the doctor sutures a wound or removes a suspicious mole during the visit, they will be paid extra for those procedures.
Although private insurance companies typically pay RHCs in the same way they pay other primary care practices, Medicare and Medicaid pay Rural Health Clinics almost exclusively through a visit-based payment, with the same amount (the “All Inclusive Rate”) paid for each visit. The payment is the same regardless of whether the patient is new or has been seen previously, regardless of the length or complexity of the visit, and regardless of whether any procedures are performed during the visit. As a result, the principal measure of volume at a Rural Health Clinic is the number of patient visits.
RHCs at the very smallest hospitals (those with less than $10 million in total expenses) generally have between 2,500 and 10,000 RHC visits each year, but the RHCs at most larger hospitals have more than 10,000 visits, and some have 20,000 or more.
Figure 35
Number of Rural Health Clinic Visits
in Small Rural Hospitals
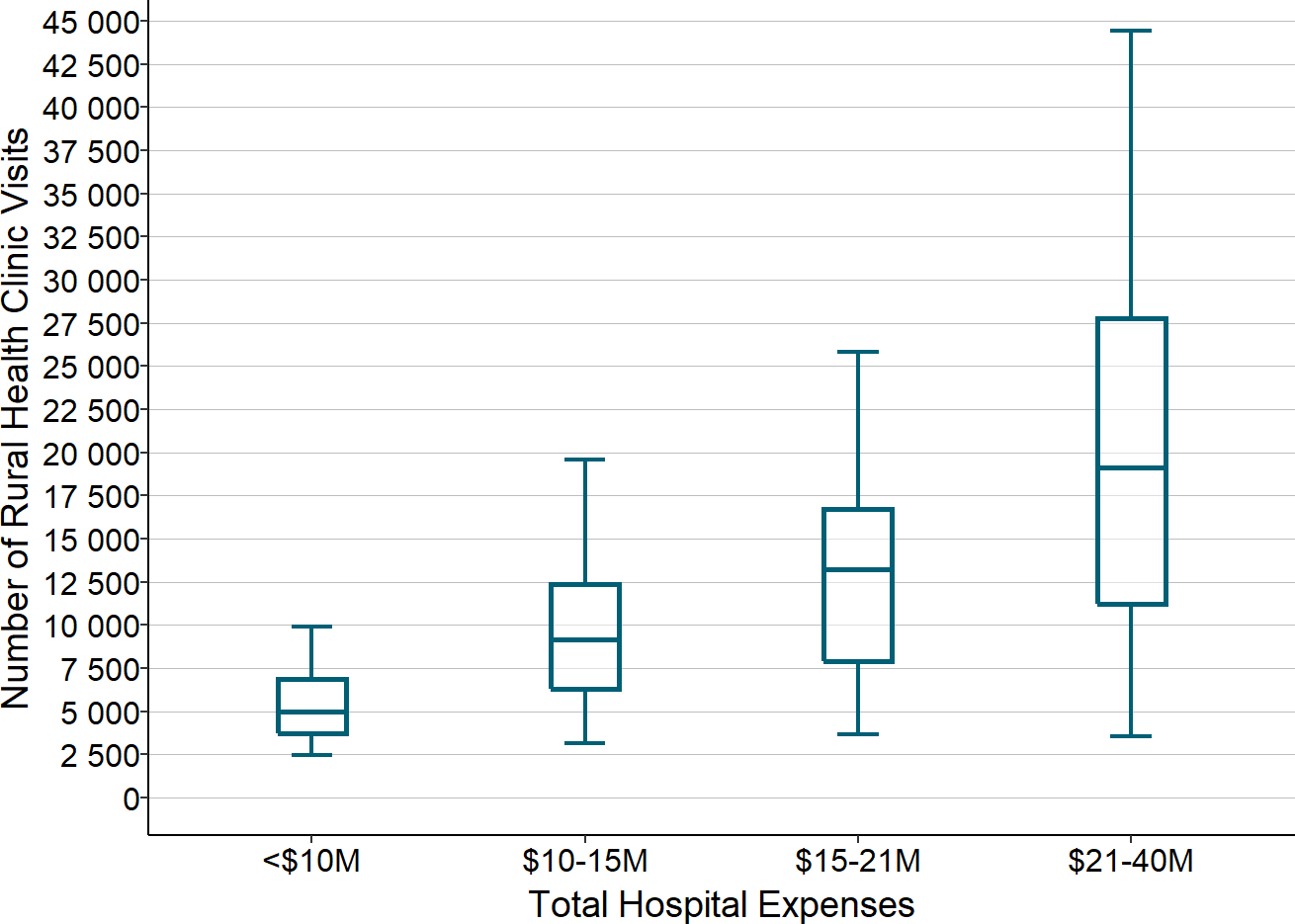
Total number of visits at rural hospitals with rural health clinics. Amounts shown are the median total number of visits at all of the RHCs at a hospital in the most recent three years available.
The volume of RHC visits varies significantly from hospital to hospital for several reasons:
- The population of the community. The more people who live in the community, the more people there are who need primary care.
- The age and health status of the population. Older individuals and people with chronic diseases will need to visit an RHC or primary care practice more often than younger and healthier patients.
- The availability of other primary care options. The more people there are in the community who need primary care, the more feasible it will be for physicians to sustain a private primary care practice in the community, which will reduce the number of residents who need or want to use a hospital’s RHC.
- The accessibility of the clinic. Many small rural hospitals serve a very large geographic area, and even though the hospital is much closer than any alternative hospital or clinic, some residents of the area still have to travel a long distance to reach the hospital. Some hospitals operate one or more clinics at a separate location in order to make clinic services more accessible to people who live in different parts of the service area.
- The cost to the patient. Although Medicare will pay more for a visit to a hospital-based RHC than to other primary care providers, patients may also have to pay higher cost-sharing, which could discourage them from using the clinic.
The Cost of Operating a Rural Health Clinic
There are five primary components that make up the cost of operating a Rural Health Clinic at a rural hospital: (1) primary care clinicians (physicians, nurse practitioners, or physician assistants), (2) other clinicians (e.g., clinical psychologists), (3) nurses, (4) other staff, and (5) overhead costs for facilities, equipment, maintenance, and billing. Medicare cost reports provide much more detailed information on the components of costs at Rural Health Clinics than for most other hospital services, which makes it easier to quantify how staffing and costs vary based on the volume of clinic visits and the amounts the RHC has to pay for staff and supplies.
Primary Care Clinicians
Every Rural Health Clinic will need at least one primary care clinician who can see and treat patients. The RHC does not need to be open for patient visits at night or on weekends, and it does not even need to be open every weekday, so the hospital has greater flexibility in staffing the RHC than it does in staffing the Emergency Department, inpatient unit, or laboratory.
In a very small community, a part-time clinician might be sufficient to handle the total number of visits the RHC expects to receive. However, the hospital may still need to hire a full-time clinician if it cannot find anyone who is available to work in the clinic on a part-time basis or if the cost of using such an individual would be higher than the cost of a full-time employee.35 A hospital that operates two RHCs may be able to hire one clinician to staff each clinic on a part-time basis, but that still requires hiring at least one full-time clinician.
If the RHC needs only one clinician, that clinician will have to be a nurse practitioner or physician assistant, not a physician, because Medicare regulations require that every RHC have at least one nurse practitioner or physician assistant on staff, that at least one nurse practitioner or physician assistant be an employee of the clinic, not a contractor, and that a nurse practitioner or physician assistant be available to provide patient care services at least 50% of the time the RHC is open for patient visits, even if there is a physician present during the same period of time.
However, even if a part-time or full-time nurse practitioner or physician assistant would be sufficient to see all of the patients who visit the clinic, the RHC will still need to employ or contract with a physician on at least a part-time basis because Medicare regulations also require that every Rural Health Clinic have at least one physician on staff (in addition to a nurse practitioner or physician assistant) to supervise care delivery. The regulations allow for the physician to work under contract or be employed, which enables an RHC to contract with a physician located in a different geographic area to provide supervision remotely using telecommunications.
The more patient visits the RHC expects to receive, the more primary care clinicians it will need in the clinic. Here again, unless the RHC is able to find clinicians able to work in the clinic on a part-time basis at a reasonable cost, it will need to add clinicians in one-FTE increments.
Figure 36
Cost of Clinicians in Rural Health Clinics
at Small Rural Hospitals
Ignoring unknown labels:
• fill : "Clinician Type"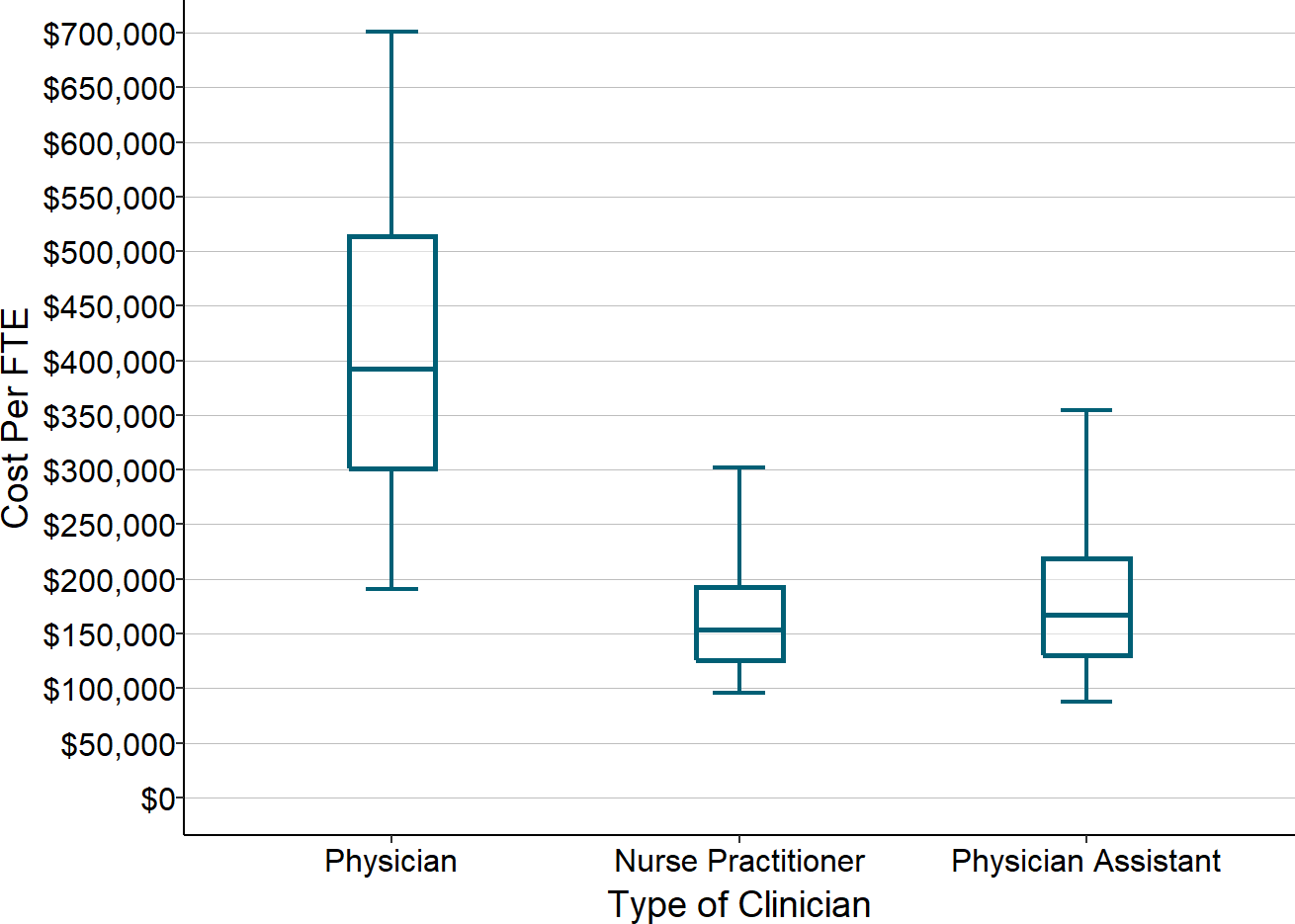
Total cost of clinicians divided by number of FTEs, for clinics with more than 0.5 FTEs of that type of clinician, at rural hospitals <$45 million total expenses. Median for the most recent three years available (excluding 2020).
Most RHCs with multiple clinicians have a mix of physicians and Nurse Practitioners and/or Physician Assistants(NPs/PAs), and the mix differs from hospital to hospital, for three reasons:
- It is generally harder to recruit and retain physicians than NPs/PAs in rural areas;
- It costs an RHC two to three times as much or more to employ a physician as an NP or PA.
- In order to receive full payment from Medicare for RHC visits, the RHC clinicians must meet a productivity standard established by the Centers for Medicare and Medicaid Services (CMS), and the standard is higher for physicians than for NPs and PAs. Each physician FTE is expected to have at least 4,200 patients visits per year, whereas each NP/PA FTE is only expected to have 2,100 patients visits per year. If a clinic wants to employ two clinicians, at least one will need to be an NP/PA to meet the Medicare regulatory requirements described earlier. If the clinic hires a full-time physician in addition to the NP/PA, it would have to have at least 6,300 visits to meet the productivity standard, but if it hires an additional NP/PA, it would only need to have 4,200 visits. As a result, a clinic that only expects to have 5,000 visits will be financially penalized for hiring a physician whereas a clinic with 7,000 visits will not. Similarly, if a clinic has 11,000 visits, it could meet the productivity standard by employing 1 physician and 2-3 FTE nurse practitioners, or 2 physicians and 1 FTE nurse practitioner, but if it employs more than 2 FTE physicians, it would likely experience a financial penalty from Medicare.
As shown in the figure below, hospital-based RHCs have approximately one additional FTE clinician for every additional 4,000 visits. In the majority of larger clinics, 40-50% of the clinicians are physicians and the remainder are a combination of NPs and PAs.
Figure 37
Number of Clinicians and Clinic Visits
in Rural Health Clinics at Small Rural Hospitals
Ignoring unknown labels:
• fill : "Cost Type"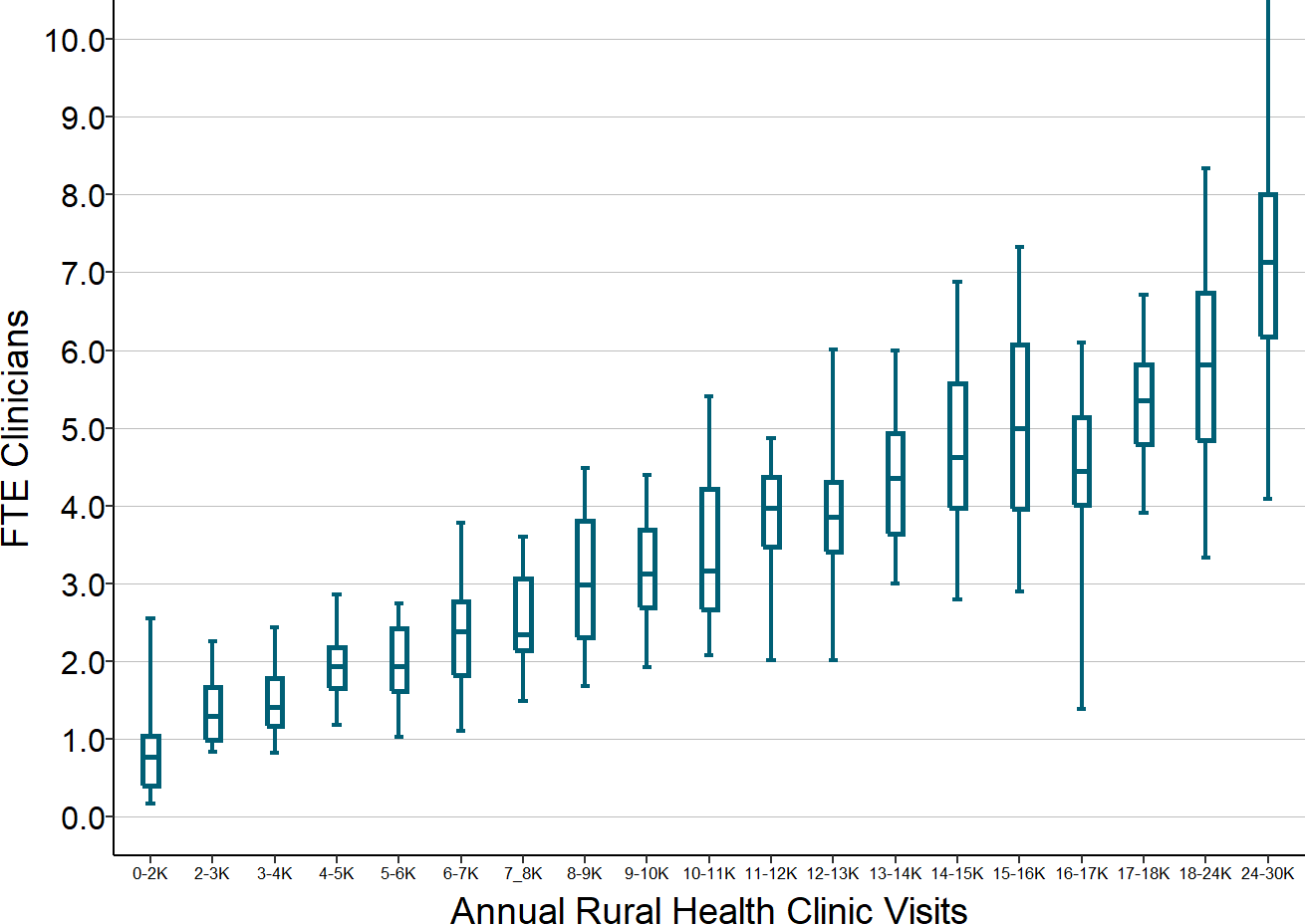
Total number of FTE (full time equivalent) physicians, nurse practitioners, and physician assistants at RHCs operated by rural hospitals <$45M total expenses. Median for the most recent three years available (excluding 2020).
Other Clinicians
Medicare and Medicaid will also pay for visits with clinical psychologists and clinical social workers if the Rural Health Clinic employs or contracts with one or more of these clinicians to work at the RHC. However, generally only RHCs in larger communities will have psychologists or social workers because there are not enough patients in smaller communities to justify hiring them.
Nurses
The majority of RHCs employ one or more nurses to complement the services provided by the physicians and/or NPs/PAs working in the clinic. The clinic generally cannot be paid for a visit unless the patient sees one of the clinicians for a medically necessary reason, but the clinicians can see a larger number of patients if a nurse can provide a portion of the services to patients, including things such as answering phone calls with questions, requests for medication refills, etc.
A common arrangement is to have one FTE nurse for each FTE clinician, although clinics in smaller communities may have fewer nurses or no nurses at all, both because there are fewer patients to support the cost of a nurse and because it is difficult to attract and retain nurses to work in a small clinic in a rural area.
RHCs are permitted to have nurses provide home care visits to patients, but only if there is no licensed home health agency serving the community. Since most communities are included in the official service area of a home health agency, most RHCs do not provide this service, even if the home health agency does not have adequate capacity to meet the need.
Medicare and a growing number of payers are paying RHCs (and other primary care providers) for care management services to patients, and these services are most often delivered by nurses. In some cases, the RHC’s existing nurses may have already been providing these care management services or they may be able to provide them in addition to their other duties, but in other cases, the RHC may need to hire one or more additional nurses in order to provide care management.
Other Staff
Most RHCs will also employ one or more medical assistants or other types of staff to support patient care in the clinic.
Other Costs
The clinic will also require space, equipment, utilities, maintenance, supplies, etc. If the clinic is not located in the same facility as the hospital, it may have to pay some or all of these costs directly, whereas if it is part of the hospital, it will generally be allocated a share of the hospital’s overall facility costs. The clinic will also need to rely on the hospital’s central human resources, medical records, billing, and other services, and so a portion of the hospital’s costs for those services will be allocated to the clinic.
Total Cost
The table below shows what the total cost could be at hypothetical Rural Health Clinics with different numbers of visits, using assumptions about the number of clinicians, nurses, wage rates, benefit levels, and indirect costs that are based on the levels typically seen in small Rural Health Clinics. These estimates are not intended to represent what the cost of any individual Rural Health Clinic should be nor are they intended to indicate what the differences in costs should be for RHCs with different numbers of visits. As discussed above, RHCs in different communities will have different numbers and types of clinicians and they will need to pay different amounts to their clinicians based on the RHC’s ability to recruit and retain clinicians in the community.
Figure 38
Estimated Cost of a Rural Health Clinic
at Hypothetical Rural Hospitals
| RHC Visits | |||||
|---|---|---|---|---|---|
| RHC Visits | 2,500 | 6,500 | 10,500 | 15,500 | |
| Staffing (FTEs) | |||||
| Physician | 0.1 | 1.0 | 1.5 | 2.0 | |
| NP or PA | 1.0 | 1.0 | 1.5 | 3.0 | |
| RN | 1.0 | 2.0 | 3.0 | 5.0 | |
| Other Staff | 1.0 | 1.0 | 2.0 | 4.0 | |
| Cost | |||||
| Physician | $165/hour | $34,000 | $343,000 | $515,000 | $686,000 |
| NP or PA | $70/hour | $146,000 | $146,000 | $218,000 | $437,000 |
| RN | $32/hour | $67,000 | $133,000 | $200,000 | $333,000 |
| Other Staff | $17/hour | $35,000 | $35,000 | $71,000 | $141,000 |
| Total Wages | $282,000 | $657,000 | $1,004,000 | $1,597,000 | |
| Benefits | 20% of Wages | $56,000 | $131,000 | $201,000 | $319,000 |
| Other Direct | $25,000 | $50,000 | $100,000 | $150,000 | |
| Total Direct | $363,000 | $839,000 | $1,304,000 | $2,067,000 | |
| Indirect Cost | 70% of Direct | $254,000 | $587,000 | $913,000 | $1,447,000 |
| Total Cost | $617,000 | $1,426,000 | $2,217,000 | $3,514,000 | |
As shown below, the estimates for the hypothetical clinics are similar to the actual costs for RHCs with those numbers of visits.36 However, there is significant variation in the costs of RHCs. Part of the variation is due to differences in the types of clinicians used, but much of it is due to variation in the amounts paid per clinician.
Figure 39
Actual vs. Estimated Costs of Rural Health Clinics
at Small Rural Hospitals
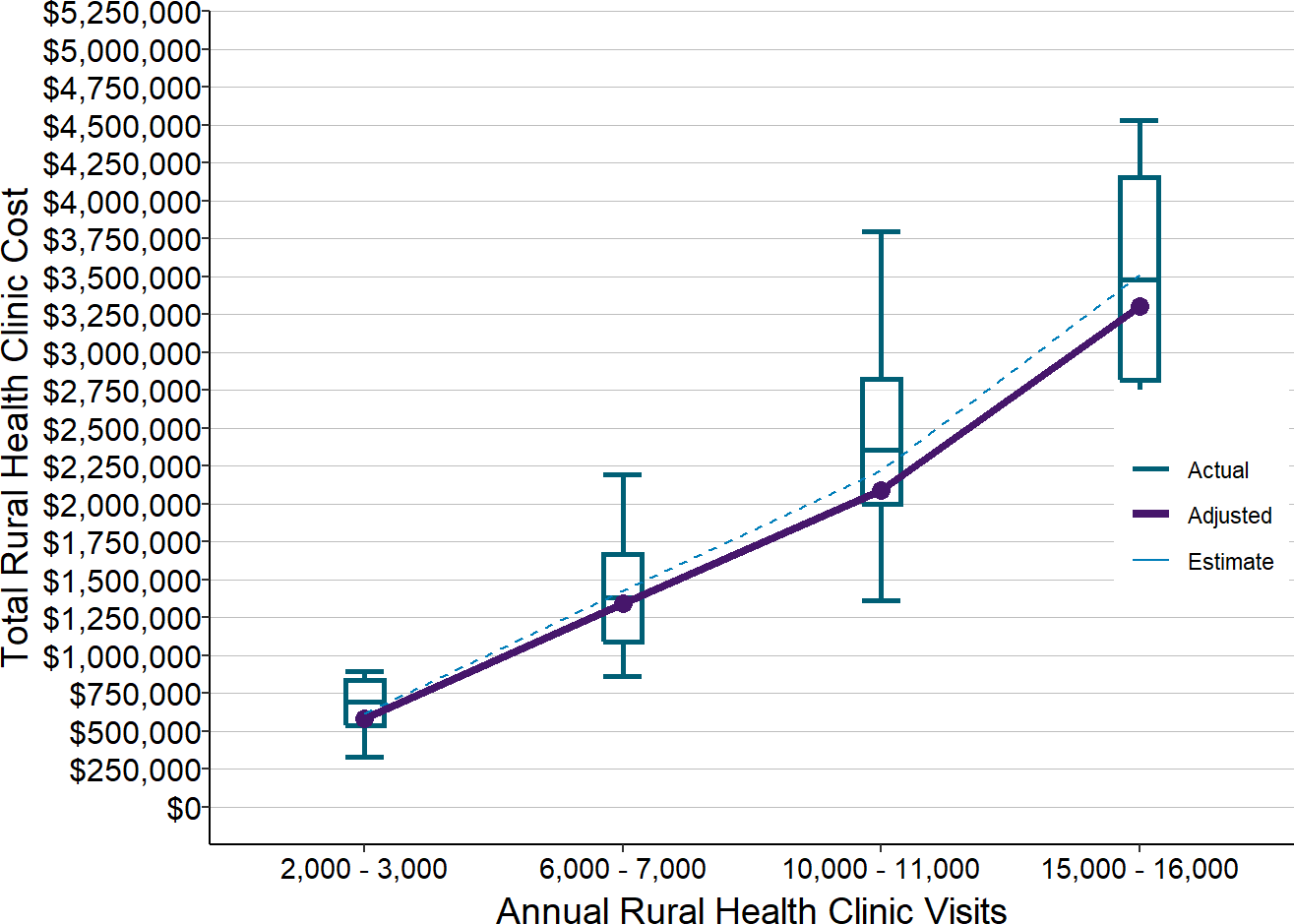
Actual amounts are for 2017-2019 at RHCs at rural hospitals <$30 million total expenses. Estimates (dotted line) are from Figure 38. Adjusted values (solid line) are the estimated values reduced to reflect inflation between 2018 and 2020.
The Average Cost Per Visit in Rural Health Clinics
Since Rural Health Clinics are typically paid a fee for each visit to the clinic, the adequacy of the fee will depend on the average cost per visit in the clinic. In the hypothetical examples, the average cost per visit ranges from $211 to $247. The differences are primarily due to the differences in the numbers of physicians vs. non-physician clinicians. Although physicians see a larger number of patients on average than NPs and PAs, the higher number of visits is generally not enough to offset the higher wages for physicians. As a result, all else being equal, an RHC with a higher ratio of physicians to NPs/PAs will tend to have a higher cost per visit.
The actual average cost per visit in most RHCs in recent years has generally been between $175 and $275. There is significant variation because of the significant variations in staffing and wage rates.
Figure 40
Average Cost Per Visit at Rural Health Clinics
Operated by Small Rural Hospitals
Ignoring unknown labels:
• fill : "Cost Type"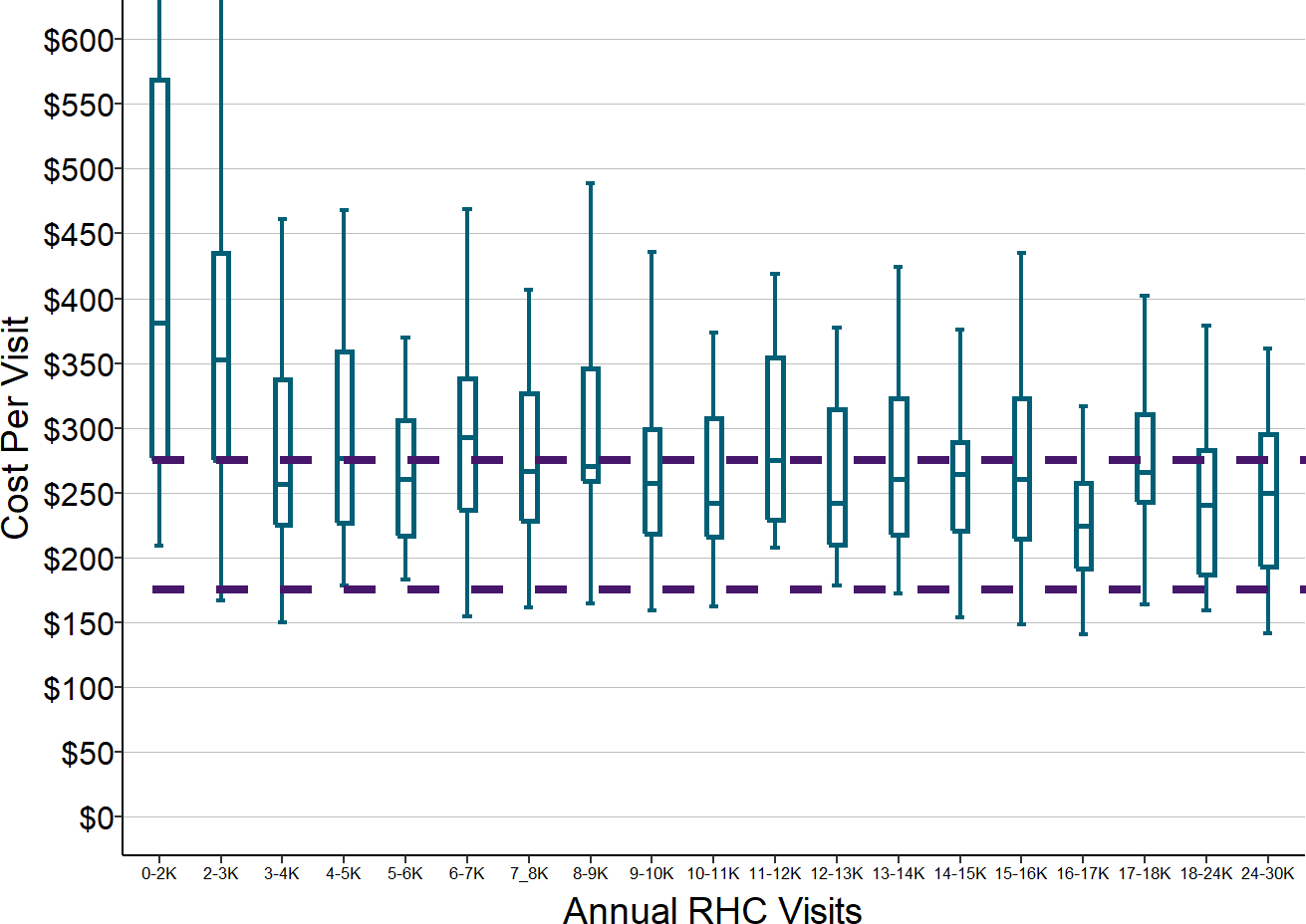
Total RHC cost divided by total RHC visits in the most recent three years available (excluding 2020) at rural hospitals with less than $45 million in total expenses.
As with other services at small rural hospitals, the average cost per visit is generally higher at hospitals with the smallest number of clinic visits. However, because of the large degree of variation in the cost per visit, some hospitals with small numbers of visits have a lower average cost per visit than many hospitals with larger numbers of visits.
Impact of Changes in Volume on the Cost Per Visit
At an individual Rural Health Clinic, the average cost per visit can change significantly over the course of a year depending on how the number of visits changes. The number of visits the clinic receives will vary from year to year and month to month based on the weather, the health of the population, the level of unemployment in the community, when patients have reached the deductibles in their insurance plans, etc. However, since the clinic staffing cannot be adjusted in small increments, the cost of the clinic will typically change very little when the number of visits changes by small amounts. This means that the cost per visit will increase when the number of visits decreases, and the cost per visit will decrease when the number of visits increases.
For example, the table below shows the hypothetical RHC with 2 clinicians that was shown previously. If patients make the 6,500 visits the clinic expected to receive, the average cost per visit will be $219. However, if the clinic receives 10% fewer visits, it still needs 2 clinicians to handle that volume of patients, so its costs will stay the same, and the cost per visit will increase by 11% to $244. If 10% more patients come to the RHC than expected, the existing physician and nurse practitioner will likely be able to handle that increase in volume, so no change in staffing will be needed, and the average cost per visit will decrease by 9% to $199.
Figure 41
Impacts of Changes in the Number of Visits
on the Cost Per Visit at a Rural Health Clinic
Base Volume
|
Lower Volume
|
Higher Volume
|
|||
|---|---|---|---|---|---|
| Amount | Amount | Change | Amount | Change | |
| RHC Visits | 6,500 | 5,850 | −10% | 7,150 | 10% |
| Total Cost | $1,426,000 | $1,426,000 | 0% | $1,426,000 | 0% |
| Cost Per Visit | $219 | $244 | 11% | $199 | −9% |
The Problems Caused by Visit-Based Fees
The standard fees for visits to primary care practices that are paid by Medicare, Medicaid, and commercial health plans are far below the average costs per visit shown above. Although Medicare pays RHCs operated by small rural hospitals based on their actual cost per visit, not based on the standard Medicare physician fee schedule, private health plans typically pay standard fees for primary care visits regardless of whether they are delivered by a Rural Health Clinic or a small physician practice. Payments from private insurance plans are typically based on the relative values in the Medicare fee schedule but may be higher or lower than the Medicare amounts. Medicare payments for Level 3 and Level 4 Evaluation & Management Office Visit for established patients, which are the most common types of visits in primary care practices, were $75 and $110 in 2019. This means that a private payer would have to pay 2-3 times the Medicare standard fees in order to cover the $252 average cost per visit at RHCs in that year.37
In addition, the problem with fee-for-service payment is not just the amount of payment, but the method. In the case of Rural Health Clinics, tying payments almost exclusively to the number of face-to-face visits with clinicians is problematic in a rural area where it can be difficult or even dangerous for a patient to travel to the clinic. If the clinicians working at the RHC can provide adequate help for a patient through a phone call or an email, thereby avoiding the need for the patient to actually come to the clinic, the clinic is financially penalized because it is not paid unless the patient comes to the clinic. In the example shown in Figure 41, if the clinic were to be paid an average of $219 per visit, it would be able to cover its costs, but if it helped 10% of the patients without the need for a visit, it would lose 10% of its revenue and no longer be able to cover its costs.
The Impact of Eliminating Inpatient Care
It is often assumed that small rural hospitals would be financially better off if they did not have to provide inpatient care. This has led to proposals to increase Medicare payments for outpatient services at rural hospitals if they close their inpatient units. For example, Congress has passed legislation to allow a small rural hospital to convert to a “Rural Emergency Hospital” by eliminating its inpatient services 38 and the Medicare Payment Advisory Commission (MedPAC) has recommended that rural hospitals be given additional subsidies if they stop providing inpatient services.39
Eliminating Inpatient Care Would Harm Hospitals Financially
However, eliminating inpatient care would actually make most small rural hospitals worse off financially. There are three reasons for this:
- Even though inpatient care is the most expensive service the hospital delivers on a per-patient basis, it is also the service the hospital delivers least frequently. As a result, the cost of operating an inpatient unit is a small part of the hospital’s overall expenses. The inpatient unit represents only 12-25% of the direct patient service costs at small rural hospitals, and since direct expenses are only 60% of the hospital’s total cost, the direct cost of the inpatient unit represents only about 7-15% of the hospital’s total expenses.
- The payments the hospital receives for inpatient care cover not only the direct cost of the inpatient unit, but a portion of the hospital’s administrative costs and other overhead. Both the direct and indirect costs assigned to inpatient units represent 15-28% of the total expenses at small rural hospitals. While some of the hospital’s overhead costs would decrease if there were no longer an inpatient unit (particularly functions such as laundry and dietary services), most of the administrative costs will not change (for example, the hospital will still need accounting staff, billing staff, and maintenance staff for its outpatient units). If there is no longer an inpatient unit, the administrative costs that had been allocated to it will have to be reallocated to the outpatient services the hospital delivers, and the hospital will have to try and recover those costs through higher charges for the outpatient services. Even if Medicare would increase its payments for outpatient services at a hospital that stops delivering inpatient services, it is unlikely that private health plans would, so the hospital will likely lose more money on outpatient services than it does with the inpatient unit in operation.
- When a patient is admitted to the hospital, the hospital is not only paid for the nursing care on the inpatient unit, but also for any ancillary services the patient receives during their stay in the hospital, such as lab tests, imaging studies, etc. Those payments help to cover the fixed costs of the ancillary services, so if the hospital no longer has inpatients, it will no longer receive those payments, and it will incur even higher losses on the ancillary services.
The graph below shows that even at rural hospitals with very small numbers of inpatients, most of the hospitals would lose far more in revenue by closing their inpatient units than they would save from terminating the nursing staff that provided inpatient care and eliminating other related costs.40 As a result, most hospitals would see their financial margins decrease, rather than improve. Even significant increases in payments from Medicare for outpatient services would not be enough to offset these losses.
Figure 42
Financial Impact of Eliminating Inpatient Services
at Small Rural Hospitals
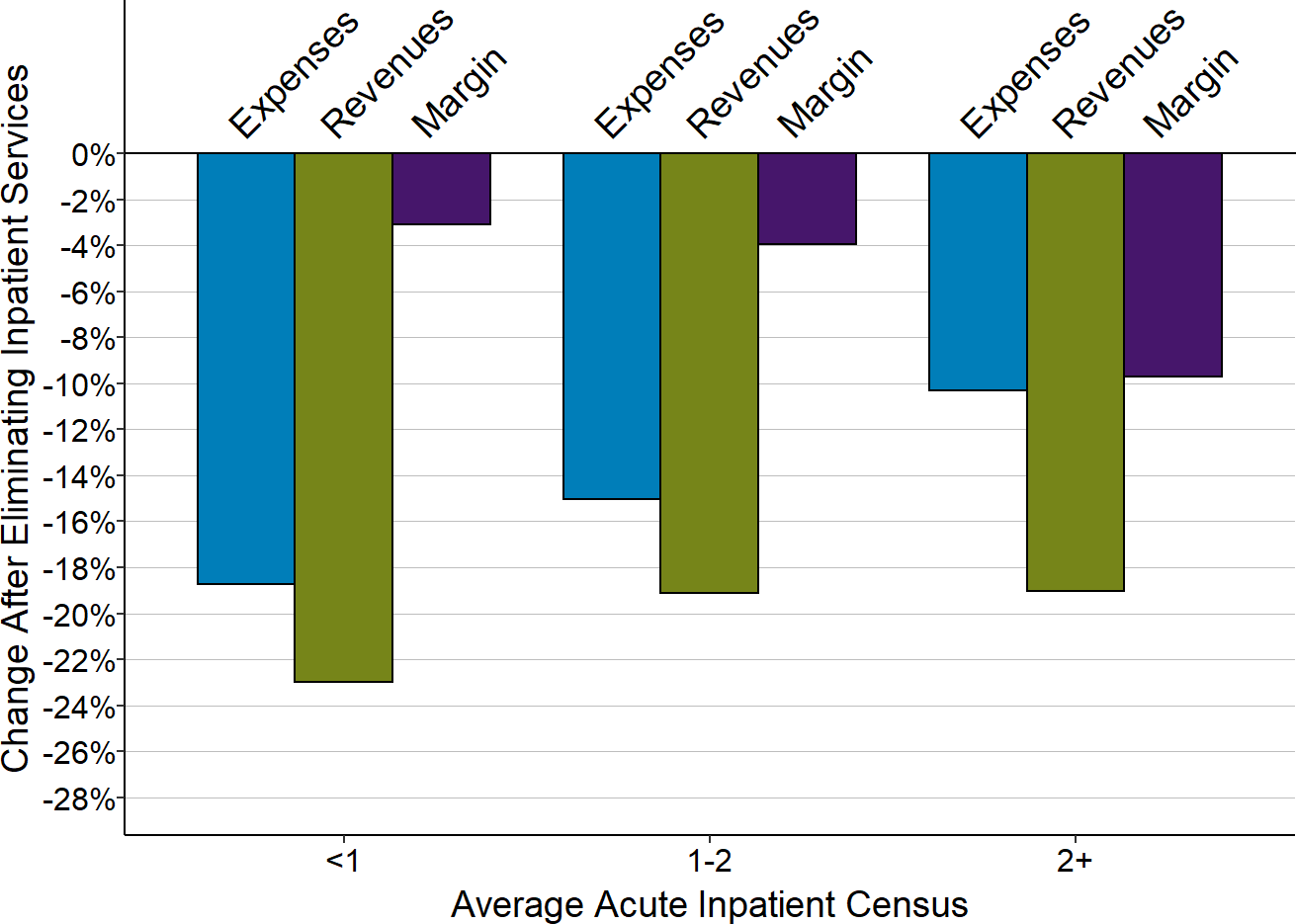
Amounts shown are medians for the most recent three years available based on estimated reduction in costs and revenues for inpatient care at rural hospitals.
Eliminating Inpatient Care Could Harm Rural Residents
In addition to the negative impact on the hospitals’ finances, closing the inpatient units at most small rural hospitals would also have a negative impact on the rural communities they serve, particularly for Medicare beneficiaries. Most of the inpatient admissions at small rural hospitals are senior citizens, and they are admitted for common acute medical conditions, such as cellulitis, pneumonia, and urinary tract infections, and for exacerbations of chronic diseases such as COPD, diabetes, and heart failure. Although better primary care will help to reduce the frequency of these admissions, there will always be some patients who have a problem that requires a short inpatient stay before they can be sent home safely, particularly if they live alone. When a senior citizen or other community resident needs to be admitted to a hospital for a few days to address one of these conditions and there are no serious complications, it will be better for the patient to be admitted to the local hospital than to be transferred to a hospital in another city. At the local hospital, their regular physician can care for them and their family and friends can more easily visit and support them, and it is likely they will receive good care at the local hospital as well as at a large, busy urban hospital.
Moreover, as discussed earlier, most small rural hospitals do not just provide acute care in their inpatient units; they also provide inpatient rehabilitation and/or long-term care services in the swing beds. Closure of the inpatient unit would result in the loss of these services for the community. Since many small rural communities do not have any Skilled Nursing Facilities separate from the hospital, this means the residents of the community would have to go to facilities in other communities for rehabilitation or long-term care, again separating them from their community physicians and families.
Why Fee-for-Service Payment Will Never Sustain Rural Hospitals
The analyses above make it clear that for every essential service that a hospital delivers, it will cost more to deliver that service to the residents of a small rural community than it would cost to deliver the same service in larger communities. Consequently, the average payments per service or per patient at a small rural hospital will have to be higher than the amounts a larger hospital would need to receive for the same service lines.
This does not necessarily mean that payments to small rural hospitals should be higher than what larger hospitals currently do receive for those services, particularly from private health plans. Many private health plans are paying small rural hospitals less than large hospitals for the same services, and the majority of large hospitals receive payments from private health plans that are much higher than the costs of delivering services and in many cases higher than is necessary to offset losses from other payers.
While increasing the fees paid for services at small rural hospitals could reduce or eliminate financial losses in the short run, fee for service payment will never be an effective solution in the long run because of a fundamental mismatch between the way fee-for-service pays for services and the way small hospitals incur costs for delivering services. Most of the hospital’s costs in virtually every service line are either fixed or semi-variable, so when patients need fewer services, fee-for-service revenues will decrease more than the cost of delivering the services will decrease, causing greater losses for the hospital. Conversely, if the volume of services increases, revenues will increase more than costs, creating profits for the hospital. This creates an undesirable incentive to deliver unnecessary services to patients. Even if fees were increased sufficiently to cover current costs, any reduction in the volume of services could push the hospital back into the red, so the hospital will want find ways to deliver more services in order to create a financial cushion against losses.
Figure 43
How Changes in Volume Affect Margins
Under Fee-for-Service Payment
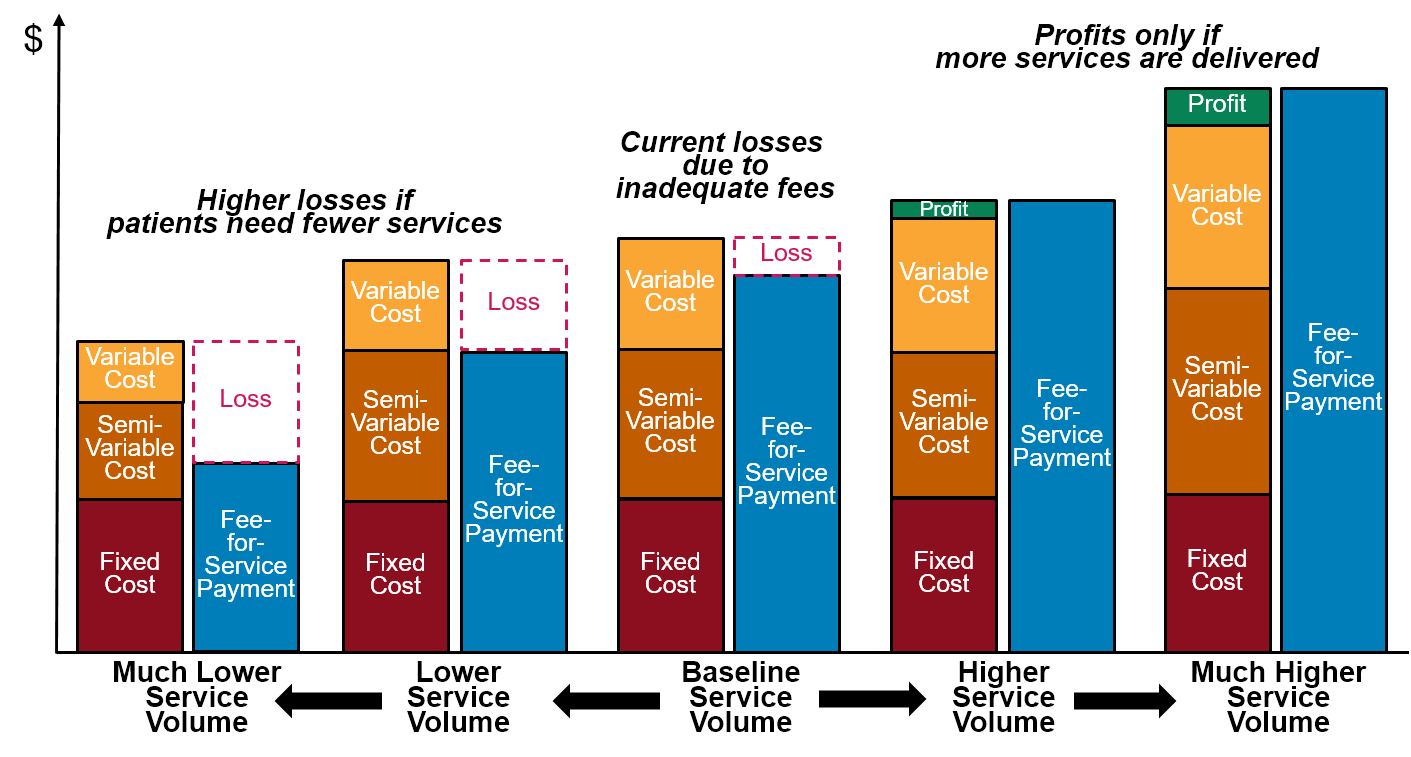
Consequently, a better method of paying hospitals is needed in addition to simply increasing the amounts of payments. Three approaches have been used or proposed for paying rural hospitals – cost-based payment, global budgets, and shared savings – but none adequately address the needs of small rural hospitals.
Footnotes
American Hospital Association. Annual Survey of Hospitals, 2017.↩︎
Although hospitals report how much of the ED cost is for “salaries” vs. “other costs,” some hospitals employ emergency room physicians while others contract with physician staffing firms, and hospitals may contract with temporary staffing agencies when they have vacancies for physicians, nurses, and other staff, so two hospitals can spend different amounts on salaries even with similar staffing and compensation levels.↩︎
As discussed below, some small Emergency Departments will use a nurse practitioner, physician assistant, or nurse with virtual or on-call physician support for some or all shifts.↩︎
Collins M. “Staffing an ED Appropriately and Efficiently.” ACEP Now (August 1, 2009).↩︎
There are 8,760 hours in the year (365 days x 24 hours); if one assumes that a full-time physician will work 2,000-2,200 hours per year (40-45 hours per week x 49-50 weeks per year), the hospital will need at least 4 full-time equivalent (FTE) physicians to staff the ED.↩︎
Hartmann M, Graziadei J. “Thirty Miles at Sea – Providing Consistent Care in an Inconsistent Environment.” New England Journal of Medicine 376(14): 1306-1307 (April 6, 2017).↩︎
Ibid.↩︎
Most hospitals schedule nurse staffing for patient care units in 12 hour shifts, and a nurse will typically work three 12-hour shifts per week. If a full-time nurse works 50 weeks over the course of the year, this represents a total of 1800 hours, and the time required for ongoing training means that the actual hours a nurse will spend delivering patient care will be lower than 1800. Since there are a total of 8,760 hours in the year (365 days x 24 hours/day), the hospital will need at least 4.9 nurses (8,760 / 1,800) to provide round-the-clock staffing.↩︎
About 60% of the total expenses at small rural hospitals are associated with direct patient services and 35% represent indirect costs. Since the total indirect costs are about 60% of the total direct costs, allocating the indirect costs to the direct costs will, on average, make the total cost of a service line 60% higher than its direct costs. The actual percentage will vary by service line, however, because each indirect cost center is allocated to the service lines based on the formulas intended to reflect the relative usage of the indirect services. For example, the hospital’s dietary services will be primarily used for inpatients, so most of the dietary costs will be allocated to the inpatient service line. The high cost of the physicians in the ED makes the direct cost in that service line relatively high, so the percentage of overhead costs is lower.↩︎
Use of clinic providers to staff the ED can be problematic for a busy clinic because some or all of the ED visits will occur at the same time as a scheduled clinic appointment. However, it also can be helpful financially for a clinic in a smaller community that does not have enough patients or scheduled visits to fully occupy the clinic providers. There is also an opportunity for greater continuity of care if the physician who treats the patient during the ED visit was already the patient’s primary care physician or if that physician begins seeing the patient in the clinic for follow-up care after the ED visit.↩︎
Galli R et al. “TelEmergency: A Novel System for Delivering Emergency Care to Rural Hospitals.” Annals of Emergency Medicine 51(3): 275-284 (March 2008).↩︎
For example, if a hospital with 10,000 visits during the entire year had 6,000 visits during three summer months and 4,000 visits during the remainder of the year, the number of visits during the summer would represent nearly 3 visits per hour on average, and this would likely require having two physicians and nurses on duty at all times. In contrast, the visits during the rest of the year would only represent one visit every 2 hours, and that would only require a single physician and nurse. The additional physician and nurse needed during the summer months would increase the total number of FTE physicians/nurses needed by 25% compared to an ED that received 10,000 visits spread evenly over the course of the year.↩︎
The “adjusted” spending amounts represent a reduction of 8.7% in the estimated amounts shown earlier in order to reflect three years of inflation, making them more representative of what costs in those years would have been, since the unit costs in the estimates were based on 2020 data. Increases in costs since 2020 willl cause the overall costs of operating Emergency Departments to increase beyond the amounts estimated here. Data are not shown for 15,000 visits because very few small rural hospitals have that many ED visits.↩︎
A small part of the variation in the chart is because the cost per visit is calculated for hospitals with visits ranging from 90-110% of the visit level shown. Some of the variation may also be due to the fact that the ED visit data came from the American Hospital Association survey and the cost data came from the Medicare cost reports.↩︎
Critical Access Hospitals are paid for ED visits in a different way by Medicare and some state Medicaid programs, but their payments are still tied to the number of visits made to the ED.↩︎
This represents only the payment for the services of the physicians, nurses, and other staff in the ED, not for lab tests, imaging studies, drugs, etc. that the patients received during the visit.↩︎
Some communities do operate “freestanding” emergency departments that are not part of an inpatient hospital. However, Medicare pays less for visits at these EDs than it pays for visit to a hospital ED, even though it will generally cost as much or more to operate a freestanding ED as a hospital-based ED (the level of staffing required will be the same, and the costs may well be higher because the ED can no longer rely on an inpatient unit to provide backup nursing support and to share general administrative costs). As a result, it is generally only feasible to operate a free-standing ED if it is able to get high per-visit payments from private health plans. This is harder to do in small rural communities than in larger communities because a low volume of visits makes the cost per visit very high.↩︎
Phillip PJ, Mullner R, Andes S. “Toward a Better Understanding of Hospital Occupancy Rates.” Health Care Financing Review 5(4): 53-61 (1984).↩︎
An average daily census of 2 patients is equivalent to 730 patient days during the year. If the average length of stay is 2.5 days, the 730 patient days represents 292 distinct patients. Since each patient will have to be both admitted and discharged, this means there will be 584 admissions and discharges during the year, for an average of 1.6 per day.↩︎
Cramer ME, Jones KJ, Hertzog M. “Nurse Staffing in Critical Access Hospitals: Structural Factors Linked to Quality Care.” Journal of Nursing Care Quality 26(4): 335-343 (2011).↩︎
The indirect cost ratio for the inpatient unit is larger than the ratio for the ED because the larger amount of space in the inpatient unit and higher use of certain central services such as dietary makes the indirect cost allocation higher for the inpatient unit. Also, the more expensive personnel in the ED will make the direct cost of the ED higher relative to other service lines, so the overhead ratio for the ED will be lower.↩︎
The “adjusted” spending amounts represent a reduction of 6% in the estimated amounts shown earlier in order to reflect two years of inflation, making them more representative of what costs in those years would have been, since the unit costs in the estimates were based on 2020 data. Increases in costs since 2020 will cause the overall costs to increase beyond the amounts estimated here.↩︎
Two hospitals can have the same average daily census with different total numbers of patients if one hospital has fewer admissions who stay slightly longer. The cost of inpatient services may be the same at the two hospitals because the average census is the same, and if so, the cost per day will be the same, but the cost per patient will be higher at the hospital with fewer admissions and a longer length-of-stay.↩︎
Critical Access Hospitals are paid for inpatient stays in a different way by Medicare and some state Medicaid programs, but inpatient revenues at Critical Access Hospitals are still tied to the number of inpatients.↩︎
The hospital will have an arrangement with an outside laboratory to process tests beyond the minimum that must be performed on site.↩︎
In small hospitals, each lab tech will need to perform most or all of the different tests that are done in the laboratory, whereas larger hospitals that perform a larger number of tests and a broader array of tests may have lab techs with more specialized training who focus on certain kinds of tests.↩︎
It is possible that there would be someone in a very small community who has the necessary training to work as a laboratory technician and who would be willing and able to work only part-time. A hospital might contract with an outside entity to provide laboratory services rather than employing lab techs directly, but the same considerations for staffing of essential on-site testing will apply regardless of who is actually employing the staff.↩︎
A lab tech on the night shift can perform tests that are needed immediately at night while also processing some of the non-urgent tests on specimens collected during the day, so having a lab tech working at night does not necessarily mean the hospital will need to hire an additional lab tech to work during the day.↩︎
The “adjusted” spending amounts represent a reduction of 6% in the estimated amounts shown earlier in order to reflect three years of inflation, making them more representative of what costs in those years would have been, since the unit costs in the estimates were based on 2020 data. Increases in costs since 2020 will cause the overall costs to increase beyond the amounts estimated here.↩︎
For example, there were 9,070 lab tests per 1,000 Medicare beneficiaries in 2018, but only 3,900 imaging studies. For younger patients, data from the Health Care Cost Institute show that in 2017, 1,238 lab/pathology services were delivered per 1,000 insured members compared to 334 radiology services. Health Care Cost Institute. 2017 Health Care Cost and Utilization Report. (February 2019).↩︎
The “adjusted” spending amounts represent a reduction of 6% in the estimated amounts shown earlier in order to reflect two years of inflation, making them more representative of what costs in those years would have been, since the unit costs in the estimates were based on 2020 data. Increases in costs since 2020 will cause the overall costs to increase beyond the amounts estimated here.↩︎
340B Drug Pricing Program Health Resources and Services Administration.↩︎
Delivering High-Value Healthcare Services in Rural Areas of Washington State: Phase 1 Findings and Recommendations of the Washington Rural Health Access Preservation (WRHAP) Project. Washington State Hospital Association, Washington State Department of Health, and Washington Health Care Authority (January 2017).↩︎
“Payment for Services Provided by Federally-Qualified Health Centers and Rural Health Clinics,” Social Security Act §1902(bb).↩︎
For example, some hospital RHCs have to fly in a physician to provide services during a portion of the week, and the cost of the travel makes this “part-time provider” very expensive.↩︎
The “adjusted” spending amounts represent a reduction of 8.7% in the estimated amounts in order to reflect three years of inflation, so they are more representative of what costs in those years would have been.↩︎
Private health plans will pay more for new patients, more for longer visits, and more when procedures are performed, but this is unlikely to be sufficient to offset the low payments for most visits.↩︎
Section 125 of the Consolidated Appropriations Act of 2021 allows a Critical Access Hospital or a hospital with less than 50 beds that is located in a rural area to be designated as a “Rural Emergency Hospital” if it provides 24-hour emergency medical care but no acute inpatient care. A Rural Emergency Hospital would be paid by Medicare for outpatient services at rates 5% higher than what other hospitals receive under the Outpatient Prospective Payment System, and the hospital would also receive an additional monthly “facility payment” based on the average difference between the amounts paid to Critical Access Hospitals under cost-based payment and the amounts they would have received under standard Medicare inpatient and outpatient payments.↩︎
Medicare Payment Advisory Commission. “Chapter 2: Using Payment to Ensure Appropriate Access to and Use of Hospital Emergency Department Services.” Report to the Congress: Medicare and the Health Care Delivery System, June 2018.↩︎
This assumes that the hospital could eliminate all of the direct costs and half of the overhead costs associated with the inpatient unit, and that non-Medicare payers pay the hospital the same percentage of its charges for inpatient care as those payers pay on average for all services. Even if it were assumed that all of the overhead costs allocated to the inpatient unit could be eliminated, the majority of small rural hospitals would still lose money by closing the inpatient unit.↩︎